Sirolimus Timing Calculator
Calculate your personalized safe start time for sirolimus based on your specific risk factors. This tool uses guidelines from the American Society of Transplantation to help determine when to begin sirolimus after surgery without compromising wound healing.
Your Personalized Recommendation
Recommended Start Time:
Risk Level:
Personalized Guidance
Why Sirolimus Slows Down Wound Healing
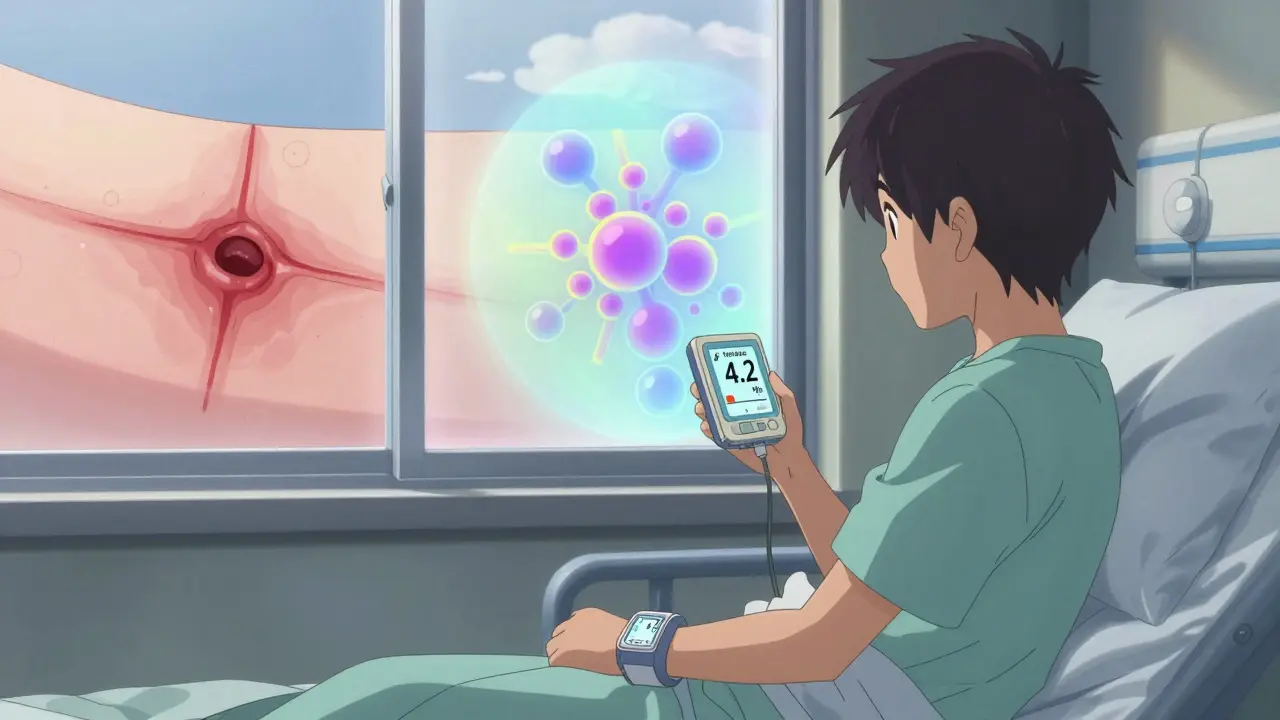
Sirolimus, also known as rapamycin, is a powerful immunosuppressant used after organ transplants to prevent rejection. But if you’ve had surgery recently, taking it too soon can seriously delay how fast your skin and tissues heal. The reason? It blocks a key cellular pathway called mTOR, which is essential for cell growth, blood vessel formation, and collagen production-all of which your body needs to close a wound properly.
Studies in rats show that when sirolimus is given at standard human doses (2.0 to 5.0 mg/kg/day), wound strength drops by up to 40%. That’s not a small drop. It means your incision is more likely to reopen, leak fluid, or get infected. In human tissue, sirolimus levels in the wound fluid are two to five times higher than in your bloodstream. That means the drug isn’t just circulating-it’s pooling right where you need healing the most.
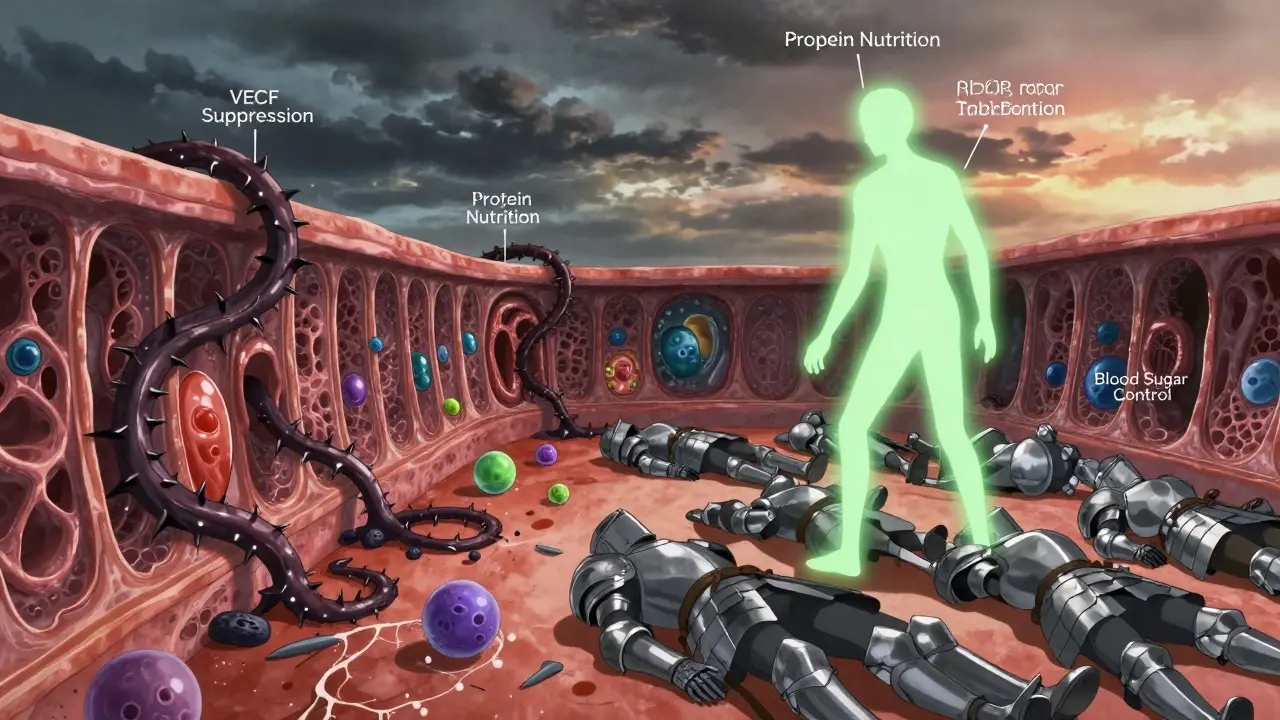
The damage happens at the cellular level. Sirolimus cuts down on VEGF, a protein that tells your body to grow new blood vessels. No new blood vessels? Less oxygen and nutrients reach the wound. It also stops fibroblasts from multiplying. These are the cells that make collagen, the scaffolding that holds your skin together. Without enough collagen, your scar is weak. And it doesn’t just affect skin. Muscle, fat, and even internal tissues heal slower.
When Do Most Doctors Wait to Start Sirolimus?
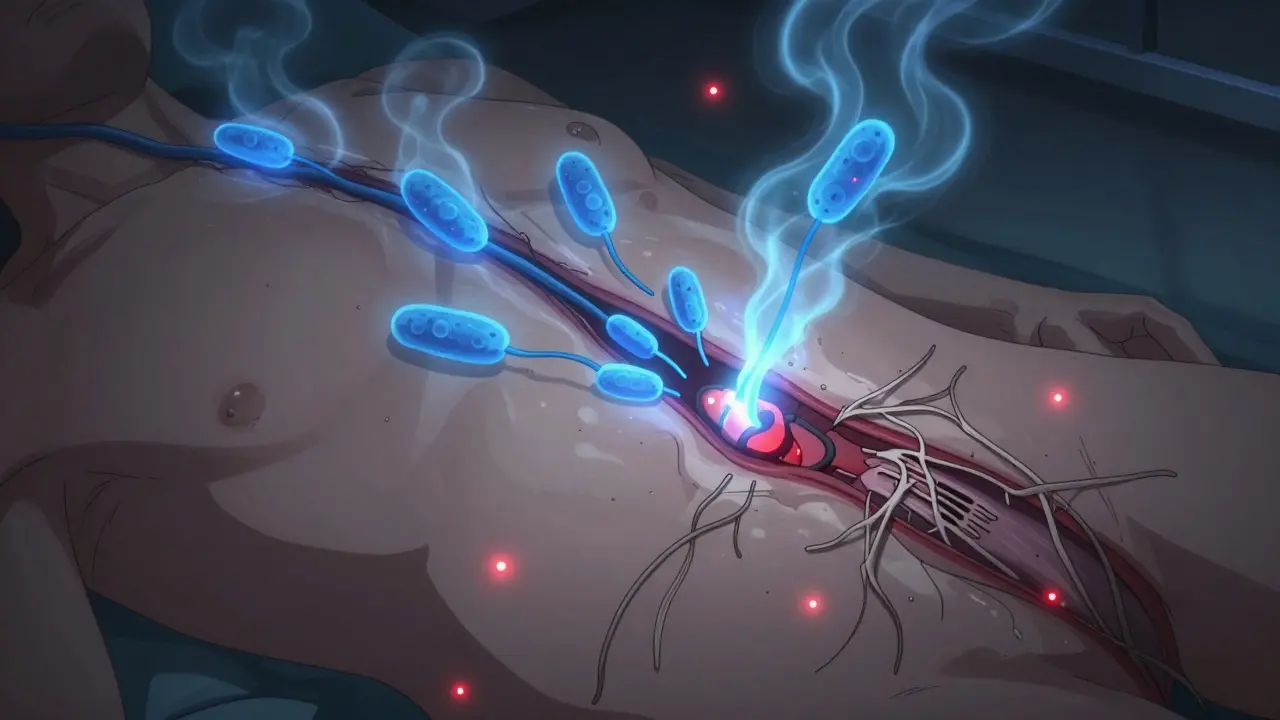
Most transplant centers don’t start sirolimus right after surgery. The standard advice? Wait at least 7 to 14 days. That’s not arbitrary. It’s based on what happens in the body during those first two weeks.
During the first 72 hours after surgery, inflammation kicks in. That’s normal. Then, around day 3 to 5, fibroblasts start moving in. By day 7, collagen begins laying down in a strong, organized pattern. If you give sirolimus before day 7, you’re hitting the body right when it’s trying to rebuild. That’s why many surgeons delay it until after the initial healing phase.
A 2009 study from Frontiers Partnerships found that many clinicians avoid sirolimus entirely during the first week post-transplant. That’s still the norm in many hospitals, especially for major surgeries like kidney or liver transplants. But it’s not a hard rule anymore. Some centers, especially academic ones, now start sirolimus as early as day 5 in low-risk patients-provided they’re young, healthy, and have no signs of poor healing.
What’s changed? Better monitoring. We now know that keeping sirolimus blood levels below 4-6 ng/mL during the first 30 days reduces complications without increasing rejection risk. That’s a game-changer. It means you don’t have to choose between safety and effectiveness-you can find a middle ground.
Who’s at Highest Risk for Complications?
Not everyone who takes sirolimus will have wound problems. But some people are far more likely to. The biggest red flag? Body mass index (BMI). Every point above 30 increases your odds of wound dehiscence-meaning your incision splits open-by nearly 2.5 times. That’s why obese patients are often advised to avoid sirolimus altogether, at least early on.
Other major risk factors include:
- Diabetes - High blood sugar slows cell repair and weakens immune defense.
- Smoking - Nicotine cuts off blood flow to the skin. Quitting at least 4 weeks before surgery makes a measurable difference.
- Protein malnutrition - If your body doesn’t have enough amino acids, it can’t make collagen. Low albumin levels are a clear warning sign.
- Older age - Healing naturally slows after 60, and sirolimus makes that worse.
- Previous poor healing - If you’ve had a wound break open before, you’re at higher risk again.
Here’s the thing: most of these are modifiable. You can’t change your age, but you can fix your diet, quit smoking, and control your blood sugar. Many transplant teams now require patients to meet certain health benchmarks before starting sirolimus. That might mean working with a dietitian for 6 weeks before surgery or getting a smoking cessation program approved.
What About Other Immunosuppressants?
Sirolimus isn’t the only drug that messes with healing. Steroids like prednisone also suppress inflammation and collagen production. Mycophenolate (CellCept) reduces white blood cell counts, making infections more likely. Antithymocyte globulin (ATG) can cause severe tissue swelling and delay healing for weeks.
So when doctors talk about wound complications, they’re often looking at a cocktail of drugs-not just sirolimus alone. That’s why some centers use sirolimus as a replacement for calcineurin inhibitors like tacrolimus or cyclosporine. Those drugs are nephrotoxic-they damage kidneys over time. Sirolimus doesn’t. So if you’re at risk for kidney failure long-term, switching to sirolimus after the wound has healed might be the better choice.
The trick is sequencing. Many patients start with tacrolimus right after transplant. Then, around week 3 or 4, if the wound looks good and labs are stable, they slowly taper off tacrolimus and add sirolimus. This gives the body time to heal before introducing the second hit.
What Do the Latest Guidelines Say?
Back in 2007, the FDA added a black box warning to sirolimus about wound healing complications. That scared a lot of doctors away from using it. But things have changed.
The American Society of Transplantation’s 2021 guidelines no longer recommend a blanket delay. Instead, they say: individualize timing based on surgical type, patient risk factors, and wound appearance. That’s huge. It means your doctor should be asking:
- Was this a major abdominal surgery or a minor skin procedure?
- Do you have diabetes or obesity?
- Are your wound edges closing cleanly?
- What’s your sirolimus trough level?
A 2008 Mayo Clinic study looked at 26 transplant patients who got sirolimus after dermatologic surgery-small skin procedures like mole removals. Only 7.7% had wound dehiscence. That’s higher than the 0% in the control group, but not statistically significant. And infection rates were similar. That suggests that for minor surgeries, the risk may be lower than we thought.
Meanwhile, a 2022 Wiley review called earlier fears about sirolimus “old myths.” The authors point out that with better dosing, better monitoring, and better patient selection, complications are now rare and manageable. In fact, some centers now start sirolimus as early as day 3 in patients with no risk factors and excellent wound healing.
What Should You Do If You’re on Sirolimus After Surgery?
If you’re recovering from surgery and taking sirolimus, here’s what matters most:
- Watch your wound daily. Look for redness, swelling, pus, or edges pulling apart. Don’t wait for your next appointment.
- Know your trough level. Ask your doctor for your last sirolimus blood test result. If it’s above 8 ng/mL, ask if lowering it could help your healing.
- Don’t smoke. Even one cigarette a day can cut blood flow to your wound by 30%.
- Eat protein. Aim for 1.2-1.5 grams of protein per kilogram of body weight daily. That’s about 80-100 grams for a 70kg person. Eggs, chicken, tofu, Greek yogurt, and whey protein shakes help.
- Control your blood sugar. If you’re diabetic, keep your HbA1c below 7%. High sugar = slow healing.
- Ask about alternatives. If your wound isn’t healing after 10 days, talk to your transplant team. Could you switch back to tacrolimus temporarily?
Remember: sirolimus isn’t the enemy. It’s a tool. Used right, it can protect your new organ for decades and lower your cancer risk. But used too early, without care, it can undo all the hard work of your surgery.
Can You Still Use Sirolimus Long-Term?
Absolutely. In fact, many patients stay on it for years. The key is timing. Once your wound is fully closed-usually by 4 to 6 weeks-the risk of complications drops dramatically. At that point, sirolimus’s benefits outweigh the risks.
It’s especially valuable for patients who:
- Have a history of skin cancer or other cancers
- Develop kidney damage from tacrolimus or cyclosporine
- Have high viral loads (like CMV or EBV) that other drugs don’t control well
Long-term, sirolimus users have lower rates of cancer and better kidney function than those on calcineurin inhibitors. That’s why many transplant teams plan to switch patients to sirolimus after the initial healing window. It’s not about avoiding it-it’s about using it at the right time, for the right person.
 Polypharmacy and Side Effects: How Taking Too Many Medications Increases Health Risks
Polypharmacy and Side Effects: How Taking Too Many Medications Increases Health Risks
 The Science Behind Maral Root: Why This Dietary Supplement Should Be in Your Arsenal
The Science Behind Maral Root: Why This Dietary Supplement Should Be in Your Arsenal
 What Are Biosimilars? A Simple Guide for Patients
What Are Biosimilars? A Simple Guide for Patients
 Clinical Trial Eligibility: How Biomarkers and Inclusion Criteria Shape Cancer Treatment
Clinical Trial Eligibility: How Biomarkers and Inclusion Criteria Shape Cancer Treatment
 What Is Medication Adherence vs. Compliance and Why It Matters
What Is Medication Adherence vs. Compliance and Why It Matters
Napoleon Huere
January 26, 2026 AT 05:31Sirolimus isn't evil-it's just a really intense roommate who shows up too early and messes with your clean-up crew. The mTOR pathway? That's your body's construction foreman. You don't send the foreman home till the foundation's set. That's just common sense, not science.
Shweta Deshpande
January 28, 2026 AT 04:14Oh my gosh, this is such a lifesaver! I just had my kidney transplant last month and was terrified to even think about sirolimus-now I feel way more confident. I’m already eating extra eggs and Greek yogurt, and I quit smoking cold turkey after reading this. My nurse even said my incision looks better than most 10-day-olds! Thank you for breaking it down like this-it’s like having a wise aunt who actually knows what she’s talking about 💕
Robin Van Emous
January 28, 2026 AT 19:49I’ve seen both sides. I’ve had patients on sirolimus heal fine. I’ve had others with perfect labs and perfect BMI who still had dehiscence. It’s not just the drug. It’s the whole system. The body doesn’t heal in a vacuum. Sleep. Stress. Hydration. Nutrition. All of it. You can’t just blame sirolimus. You’ve got to look at the whole picture.
James Nicoll
January 29, 2026 AT 11:42So let me get this straight… we’ve got a drug that prevents rejection, reduces cancer risk, and protects kidneys… but we’re scared to use it because it might make your skin take an extra week to heal? Sounds like we’re treating a transplant like it’s a bad Tinder date. Don’t rush. Don’t overcommit. Just… wait until the spark fades.
Uche Okoro
January 31, 2026 AT 02:45The mTOR inhibition cascade is a well-documented impediment to angiogenesis and fibroblast proliferation, mediated through downstream suppression of HIF-1α and TGF-β signaling. Clinical correlation is robust in high-BMI cohorts, particularly with concomitant glucocorticoid exposure. The 4–6 ng/mL therapeutic window is empirically validated in multicenter cohorts, but pharmacokinetic variability in South Asian populations remains underreported.
shivam utkresth
February 1, 2026 AT 10:47Bro, this is straight fire. I’m from a small town in India where half the patients get discharged with no one telling them to eat protein. My cousin got his liver transplant and was told to ‘take the pill’ and ‘go home’. No diet plan. No blood sugar check. No nothing. We’re lucky if they even know what ‘trough level’ means. This post should be translated into 10 languages and plastered on every clinic wall in the Global South.
John Wippler
February 2, 2026 AT 02:47You know what’s wild? The fact that we treat healing like a race. We want it fast. We want it perfect. We want it yesterday. But your body doesn’t care about your schedule. It cares about protein, sleep, and peace. Sirolimus isn’t the villain-it’s the guy who shows up late to the party and ruins the vibe. So don’t let him in until the house is clean. Your future self will thank you.
Aurelie L.
February 4, 2026 AT 02:00So… you’re saying I shouldn’t take my sirolimus until my scar looks like a straight line? And I have to eat 100 grams of protein? And not smoke? And check my blood sugar? And wait 14 days? Wow. I guess I’ll just die then.
Joanna Domżalska
February 5, 2026 AT 10:07Everyone’s acting like sirolimus is the devil. But if your body can’t heal without it being delayed, maybe your body is broken. Maybe you shouldn’t have gotten a transplant in the first place. This is just fear-mongering dressed up as medicine.
Josh josh
February 7, 2026 AT 03:15bella nash
February 8, 2026 AT 19:37SWAPNIL SIDAM
February 9, 2026 AT 12:49