Medication adherence isn’t just about taking your pills-it’s about being part of the plan
You’ve been prescribed a new medication. Your doctor says to take it once a day. You mean well. But life gets busy. You forget. You skip a dose because you felt fine yesterday. You stop taking it because the side effects made you miserable. Or maybe you just can’t afford it. You’re not lazy. You’re not stubborn. You’re human.
For decades, doctors called this compliance. If you didn’t follow the script exactly, you were labeled non-compliant-as if the problem was your failure to obey. But that language is outdated. And it’s dangerous.
Today, the medical world uses a different word: adherence. It’s not just a synonym. It’s a complete shift in thinking. And understanding the difference could save your life-or someone you love.
Compliance is a one-way street. Adherence is a partnership
Compliance means doing what you’re told. No questions. No input. You get a prescription. You take it. That’s it. If you don’t, you’re failing.
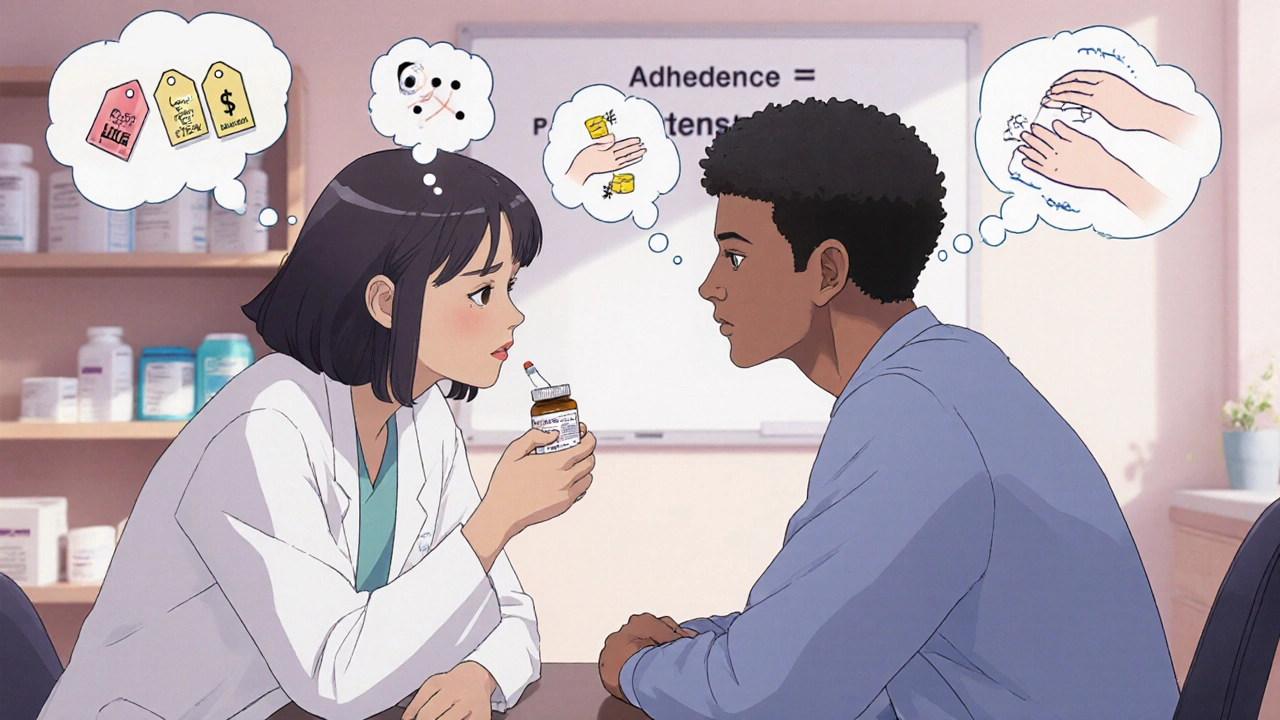
Adherence means you’re part of the decision. Your doctor asks: “What’s your schedule like?” “What worries you about this pill?” “Can you afford it?” Then they adjust. Maybe the dose changes. Maybe the timing shifts. Maybe a cheaper alternative is found. It’s not about perfect obedience. It’s about what works for you.
The American Pharmacists Association defines adherence as “the extent to which a patient’s behavior corresponds with agreed-upon recommendations.” Notice the word agreed-upon. That’s the key. It’s not a command. It’s a contract you helped write.
This shift didn’t happen overnight. In the 1990s, doctors started noticing something strange: even when patients were told exactly what to do, half of them stopped taking their meds within a year. The problem wasn’t ignorance. It was disconnection.
Why the switch from compliance to adherence? Because people aren’t robots
Think about your own life. You know you should exercise. You know you should eat less sugar. But you don’t always do it. Why? Because you’re tired. Because it’s expensive. Because you don’t like the taste. Because you’re stressed. These aren’t moral failures. They’re human realities.
Medications are the same. A 2023 study in the Journal of Clinical Pharmacy and Therapeutics found that 68% of patients who skipped doses did so because of side effects, cost, or confusion-not because they were rebellious.
Compliance ignores all that. It assumes if you just followed orders, you’d be fine. Adherence says: Let’s figure out why you’re struggling-and fix it together.
Take diabetes. A patient might stop taking metformin because it gives them stomach cramps. A compliance approach says: “Take it anyway.” An adherence approach says: “Let’s talk about your diet. Maybe we switch to a different drug. Or lower the dose. Or try a once-daily version.” The goal isn’t to force obedience. It’s to keep you alive and feeling better.
How do we measure adherence? It’s not just pill counts
Compliance used to be measured by counting pills. Did you take 30 pills this month? Yes? Good. No? Problem.
Adherence is more complex. It looks at four stages:
- Initiation: Did you start the medication at all?
- Implementation: Are you taking it at the right time, in the right dose?
- Persistence: Are you still taking it after weeks or months?
- Discontinuation: Did you stop-and why?
The American Medical Association says you’re considered adherent if you take at least 80% of your prescribed doses over a given period. That’s not perfection. It’s realistic.
Tools now track this in real time. MEMS caps (electronic pill bottles) log when you open them. Apps remind you. Pharmacies track refill patterns. Some systems even use AI to predict who’s likely to miss doses-based on income, zip code, past behavior, and even weather.
One 2024 study with 12,000 patients found that using a digital adherence tracker improved medication possession rates by 28.7%. That’s not a small win. That’s thousands of hospital visits prevented.
Why does this matter? Because lives are on the line
Non-adherence isn’t just inconvenient. It’s deadly.
The World Health Organization estimates that poor medication adherence causes 125,000 deaths in the U.S. every year. That’s more than car accidents. It’s more than HIV/AIDS. And it’s mostly preventable.
For people with high blood pressure, skipping doses leads to strokes. For those with heart failure, it means emergency room visits. For cancer patients, missing chemo cycles reduces survival odds by up to 30%.
But here’s the twist: it’s not the patient’s fault. It’s the system’s.
Doctors have 15-minute appointments. They’re rushed. They don’t ask about cost. They don’t check if the patient can read the label. They don’t know if the patient’s fridge is broken and the insulin is spoiling.
Adherence-based care changes that. It trains providers to listen. To ask: “What’s getting in your way?” Not “Why aren’t you doing what I told you?”
What does adherence look like in real life?
Here’s what works:
- Motivational interviewing: Instead of lecturing, providers ask open-ended questions: “What do you hope this medicine will do for you?”
- Shared decision-making tools: Apps that show side effect risks vs. benefits in plain language.
- Pill organizers with alarms: Simple, low-tech, and effective.
- Cost assistance programs: Pharmacies now offer $4 generic lists and manufacturer coupons.
- Text reminders: A 2023 Kaiser Permanente study found text alerts cut missed doses by 42%.
One clinic in Boston started asking every patient: “What’s one thing that makes it hard to take your meds?” Within six months, adherence rates jumped 37.6%. The answer? “I can’t afford it.” So they linked patients to free samples. Another said: “I forget because I’m on a night shift.” So they switched to morning dosing. No judgment. Just solutions.
Why compliance still lingers-and why it’s fading fast
Some places still use the word “compliance.” Prisons. Nursing homes. Some insurance forms. But even there, it’s changing.
The FDA and European Medicines Agency now require adherence data in clinical trials-not just compliance. Why? Because if a drug looks effective in a trial but patients in the real world stop taking it, the drug isn’t actually effective.
Medicare now ties 8% of hospital payments to adherence outcomes for chronic conditions like heart disease and COPD. Hospitals are being paid to keep patients out of the ER. That means they have to help them take their meds.
And in 2025, the American Medical Association added new billing codes (99487-99489) just for adherence counseling. For the first time, doctors get paid for talking to patients-not just prescribing.
By 2024, 87% of major U.S. health systems had officially switched to “adherence” in all their materials. The National Patient Advocate Foundation ran a campaign that got 47 organizations to retire the word “compliance” from their policies.

What you can do right now
If you’re on medication:
- Don’t stop taking it just because you feel better. Talk to your provider first.
- If it’s too expensive, ask: “Is there a generic? A coupon? A patient assistance program?”
- If you’re having side effects, don’t suffer in silence. Say: “This isn’t working for me.”
- Use a pillbox. Set a phone alarm. Text a friend to remind you.
- Bring your meds to your next appointment. Let your doctor see what you’re actually taking.
If you’re a caregiver or family member:
- Don’t nag. Ask: “What’s the hardest part about taking your pills?”
- Help them organize. Buy a pillbox. Set up a reminder system.
- Don’t assume they’re being difficult. They might be scared, overwhelmed, or broke.
It’s not about following rules. It’s about staying alive
Medication adherence isn’t a buzzword. It’s not a trend. It’s a lifeline.
Compliance treats patients like children. Adherence treats them like adults-with respect, dignity, and agency.
The science is clear: when patients feel heard, they take their meds. When they’re blamed, they shut down.
And when they take their meds? They live longer. They stay out of the hospital. They spend less money. They feel more in control.
This isn’t about perfect obedience. It’s about partnership. It’s about listening. It’s about building a plan that actually fits your life.
Because your health isn’t a checklist. It’s your life.
What’s the difference between medication adherence and compliance?
Compliance means following a doctor’s instructions without question-like a child obeying a parent. Adherence means working together with your provider to find a plan that fits your life, your schedule, and your needs. Adherence acknowledges your choices, your barriers, and your input. Compliance blames you if you don’t follow orders. Adherence asks, “What’s getting in your way?”
Is adherence the same as taking your pills on time?
It’s more than that. Adherence includes starting the medication, taking it correctly, continuing it over time, and knowing why you’re taking it. You can take your pills on time but still be non-adherent if you don’t understand why you’re taking them-or if you’ve stopped because you’re scared of side effects. Adherence looks at the whole picture, not just the dose.
Why do so many people stop taking their meds?
Cost is the #1 reason-nearly 1 in 4 Americans skip doses because they can’t afford them. Side effects come next. Then forgetfulness, confusion about instructions, or believing they don’t need it anymore because they feel fine. It’s rarely about laziness or rebellion. It’s about real-life barriers that aren’t being addressed.
Can technology help with medication adherence?
Yes. Electronic pill bottles that log when you open them, smartphone apps that send reminders, and smart pill dispensers like Hero Health have been shown to reduce missed doses by up to 42%. Even simple text message reminders cut non-adherence by 30%. These tools don’t replace human connection-they support it.
What should I ask my doctor about my meds?
Ask: “What’s this for?” “What happens if I miss a dose?” “Is there a cheaper option?” “What side effects should I watch for?” “How will I know if it’s working?” “Can we adjust the timing if I work nights?” These questions turn a prescription into a plan-and make you part of the team.
Next steps: Make adherence part of your routine
Start today. Grab your pill bottle. Look at the label. Do you know why you’re taking it? Can you afford it? Do you understand the side effects? If not, write down your questions and bring them to your next appointment.
Don’t wait until you feel worse. Don’t wait until you’re in the ER. Adherence isn’t about being perfect. It’s about being supported. And you deserve that.
 What to Do If a Child Swallows the Wrong Medication: Immediate Steps That Save Lives
What to Do If a Child Swallows the Wrong Medication: Immediate Steps That Save Lives
 How to Choose OTC Eye Drops for Allergies, Dryness, and Redness
How to Choose OTC Eye Drops for Allergies, Dryness, and Redness
 RexMD Sleep Aids and Fast Online Pharmacy Alternatives: Products, Doctor Reviews, and Delivery Insights
RexMD Sleep Aids and Fast Online Pharmacy Alternatives: Products, Doctor Reviews, and Delivery Insights
 Discover Hericium Erinaceus: The All-Natural Miracle Supplement You Need to Try Today
Discover Hericium Erinaceus: The All-Natural Miracle Supplement You Need to Try Today
 FDA-Approved Medications You Can Flush Down the Toilet (And Which Ones You Shouldn’t)
FDA-Approved Medications You Can Flush Down the Toilet (And Which Ones You Shouldn’t)
Sameer Tawde
November 18, 2025 AT 16:46We need more doctors who ask 'what's stopping you?' not 'why aren't you listening?'
Jeff Hakojarvi
November 20, 2025 AT 09:09they just kept sending her letters saying she was 'non-compliant.' like duh, the system is broken, not me.
Timothy Uchechukwu
November 20, 2025 AT 22:37if you cant follow simple instructions dont expect to live long
Ancel Fortuin
November 21, 2025 AT 01:28meanwhile the pharma companies are laughing all the way to the bank while we get 'text reminders' instead of real solutions.
next they'll be asking if your pillbox has enough emotional support
Samkelo Bodwana
November 21, 2025 AT 08:20Adherence isn’t just a buzzword-it’s a symptom of a deeper failure. We’ve outsourced care to algorithms and pills while abandoning human connection.
The fact that we now have billing codes for talking to patients says everything. We’re only now being paid to do what medicine should’ve always been about: listening.
I’ve worked in rural clinics where the biggest barrier to adherence wasn’t cost or side effects-it was the shame patients felt when they admitted they didn’t understand the instructions.
No one wants to say, 'I can’t read this label.'
So they nod. They take the pill. They don’t come back.
And then they end up in the ER.
We need more community health workers, more plain-language education, more time-not more tech.
Tech helps, sure. But a text reminder won’t fix the fact that your fridge is broken and your medicine is spoiling.
That requires a neighbor checking in. A clinic offering free coolers. A doctor who doesn’t rush.
Adherence isn’t about compliance. It’s about dignity. And dignity can’t be coded.
Angela J
November 23, 2025 AT 03:58i heard it on a podcast. they're already linking pill bottle data to your credit score.
you think this is about health? it's about control.
Sarbjit Singh
November 24, 2025 AT 20:08simple things work. no need for fancy apps. just love and patience. ❤️
Jonathan Gabriel
November 25, 2025 AT 03:41interesting. so if i call my cat 'a cohabitant' instead of 'a pet,' does that mean the cat suddenly starts doing laundry?
language doesn’t fix systemic failure.
if 68% of people skip meds due to cost, then the problem isn’t their 'behavior'-it’s that we let pharmaceutical monopolies charge $500 for a pill that costs $2 to make.
calling it 'adherence' is just rebranding negligence as empathy.
Don Angel
November 25, 2025 AT 12:58It’s so easy to fall into the trap of thinking people are just being lazy.
But the truth? Most people are doing their best with terrible options.
I’ve seen patients cry because they had to choose between insulin and rent.
No one should have to make that choice.
And no one should be shamed for it.
This shift to adherence? It’s not just medical-it’s moral.
We owe it to each other to do better.
benedict nwokedi
November 26, 2025 AT 12:22You want to know why people don't take their meds? Because they don't respect authority.
Because they think they know better.
Because they're addicted to their own narratives.
And now we're rewarding that with 'shared decision-making' and 'text reminders'?
The only thing that works is discipline.
And discipline is not 'inclusive.'
It's not 'empathetic.'
It's just... correct.
deepak kumar
November 26, 2025 AT 21:51My uncle was diabetic and stopped his meds because he thought sugar-free meant 'no sugar at all.' He didn't know 'sugar-free' meant 'no added sugar.'
His doctor never checked.
We fixed it with a simple WhatsApp voice note in Hindi.
No app. No billing code. Just someone who cared enough to explain.
Adherence isn't a system. It's a relationship.
Dave Pritchard
November 27, 2025 AT 14:16One patient said: 'I don't have a phone.'
So we gave her a paper calendar and a sticker chart.
Another said: 'I'm scared the pills will make me sick.'
We sat with her for 20 minutes, drew out how the meds work, and let her pick the time she felt safest taking them.
Adherence isn't about getting people to obey.
It's about making them feel like they belong in their own healing.
And that? That changes everything.