Ever heard of Zollinger-Ellison Syndrome? If not, you're not alone. It's not something that often comes up in dinner conversations, but for those affected, it can be a massive part of their lives. So, what's going on when someone has this syndrome? Basically, it's a condition where tumors in your pancreas or small intestine make way too much of a hormone called gastrin, leading to stomach ulcers and discomfort.
But hold up, not all tumors are the same. In this case, we're talking about pancreatic neuroendocrine tumors. Sounds a bit intimidating, right? Let's keep it simple. These are rare and usually slow-growing tumors that can really mess with the balance of things in your gut. They crank up gastrin production, and that's when the acid flows like it's got no brakes.
Folks with this condition often battle with symptoms like tons of ulcers and darn tricky-to-treat acid reflux. Knowing the signs is crucial because early diagnosis can make a world of difference. So, hang tight as we break down what exactly you should be looking out for, and more importantly, what you can do about it.
- What is Zollinger-Ellison Syndrome?
- The Role of Gastrin and Tumors in ZES
- Symptoms and Diagnosis
- Managing and Treating ZES
What is Zollinger-Ellison Syndrome?
Alright, let's get into the nitty-gritty of what Zollinger-Ellison Syndrome, or ZES, really is. At its core, it’s a rare condition caused by one or more tumors, called gastrinomas, popping up in your pancreas or small intestine. These little troublemakers produce too much gastrin, which is a hormone that tells your stomach to make acid. Think of it like your stomach is a super soaker, and these tumors turn up the pressure.
So, what does all that extra acid do? Well, it’s responsible for those nasty ulcers you might have heard about. Some folks think ulcers are just about stress or spicy food, but in the case of Zollinger-Ellison Syndrome, it's these gastrinomas causing havoc. The stomach lining gets battered by acid, causing peptic ulcers that are pretty stubborn and painful.
More About These Gastrinomas
Most of these tumors are found in the pancreas or duodenum – the first part of your small intestine. They might also pop up in lymph nodes about 20% of the time. Here's something wild: around two-thirds of these gastrinomas are malignant, meaning they can spread to other parts, most commonly the liver.
Who's at Risk?
Though anyone can develop ZES, it’s quite rare. We're talking about 1 in a million folks annually in the U.S. It doesn't pick favorites when it comes to gender, but it often rears its head between the ages of 20 and 50. Sometimes it runs in families due to genetic conditions like Multiple Endocrine Neoplasia type 1 (MEN1).
If you're wondering whether ZES is in your future, taking a look at family history and being vigilant about symptoms can go a long way. We're talking severe stomach pain, diarrhea, or recurring ulcers that don't respond to standard treatment.
Spotting the Symptoms
We can’t stress enough the importance of recognizing the signs early. Common symptoms go beyond just a tummy ache. They include:
- Severe and persistent abdominal pain
- Chronic diarrhea from acid reaching the intestines
- Weight loss, because constant acid and stomach pain can mess with your appetite
- Nausea or vomiting when those ulcers act up
The biggest challenge with ZES is that it can mimic other, more common digestive issues. If peptic ulcers are resistant to treatment or recurring, it's time to consider exploring the possibility of Zollinger-Ellison Syndrome.
The Role of Gastrin and Tumors in ZES
Alright, let's talk about what's really stirring the pot in Zollinger-Ellison Syndrome. The big player here is a hormone called gastrin. This hormone's main job is to tell your stomach to produce acid. Normally, our bodies know when to keep it chill, but in ZES, things get out of control.
So, why all the fuss about tumors? These specific troublemakers, often found in the pancreas or the small intestine—officially known as neuroendocrine tumors—start producing too much gastrin. This means your stomach is constantly on acid overload mode, which can lead to serious ulcer problems. Not fun, right?
Here's an interesting tidbit: While these tumors are rare and usually move at a snail’s pace, they are quite persistent. Once these tumors decide to stick around, they create a breeding ground for more and more acid, which spells even more pain and discomfort.
How Do These Tumors Affect the Body?
When gastrin levels spike due to these tumors, you get multiple, hard-to-manage ulcers. You might think, "Hey, pop a few meds and you're good to go." Unfortunately, that's not always the case. The ulcers in ZES don’t respond like your normal garden-variety ones. That’s why getting the right treatment is super crucial.
- First Stage: Tumors start forming in the pancreas or small intestine.
- Second Stage: Excess gastrin floods your system, causing a spike in stomach acid production.
- Final Stage: This overproduction leads to stubborn ulcers that can cause intense pain and discomfort.
So, in a nutshell, these tumors throw the body’s natural balance way out of whack, and it takes a game plan to get things back on track. Next, we'll dive into the signs and signals this condition sends your way. Stay tuned, because recognizing these signs early on can really make a difference in the journey to manage and treat ZES effectively.

Symptoms and Diagnosis
Spotting Zollinger-Ellison Syndrome can be tricky because it mimics other common gastrointestinal issues. However, knowing the tell-tale signs could save a lot of trouble down the road. So, what symptoms should raise a red flag?
Common Symptoms
- Frequent, hard-to-treat stomach ulcers that don't respond well to traditional treatments.
- Intense abdominal pain that feels like something's gnawing away inside.
- Persistent diarrhea which can be pretty uncomfortable.
- Heartburn that could rival the best fireworks show in town.
- Unexplained weight loss and fatigue, which might have you feeling worn out without any clear reason.
If these symptoms sound way too familiar, it might be time to talk diagnosis. Let's dive into how this condition is diagnosed.
Diagnosis How-To
The process of diagnosing Zollinger-Ellison Syndrome is like solving a mystery. It often starts with a blood test to measure gastrin levels. If they are sky-high, it’s a solid clue.
Doctors may also use imaging tests to hunt down the sneaky tumors in the pancreas or small intestine. These can be MRI or CT scans—kinda like having a high-tech photographer see what's happening inside.
Special Tests
Sometimes, experts might even perform an endoscopy, where a tube goes down your throat to take a peek and, if necessary, get a tissue sample. It’s not as scary as it sounds, and it can reveal a lot about what's going on.
If the idea of all these tests makes you anxious, don’t worry. Doctors deal with this all the time, and they’re pretty good at it. And hey, getting answers is one step closer to feeling better, right?
Managing and Treating ZES
Dealing with Zollinger-Ellison Syndrome can seem overwhelming, but there are effective strategies to keep it in check. The first step often revolves around taming that out-of-control stomach acid. You might think medications are your best friend here, and you're not far off.
Medications
People with ZES frequently rely on proton pump inhibitors (PPIs) — drugs that do a great job of reducing stomach acid. They help prevent more ulcers from popping up and give your digestive system some much-needed relief.
- PPIs: These include options like omeprazole or pantoprazole, taken regularly to curb acid production.
- H2 Blockers: Though secondary to PPIs, they’re another option which works by decreasing acid creation.
Surgical Options
Sometimes, surgery steps into the mix, especially if the tumors are messing with more than just your stomach. Surgeons might aim to remove pancreatic neuroendocrine tumors, giving the root cause of the syndrome a proper send-off. It's not always necessary, but for some, it could be the long-term game-changer they've been waiting for.
Monitoring
Keeping tabs on how things are going is crucial. Regular follow-ups with your healthcare crew help track progress and tweak treatments. They might run blood tests to measure the level of gastrin and imaging tests to check on the tumors. Staying on top of this stuff can mean catching changes before they turn into bigger issues.
Diet and Lifestyle
Let's not forget about the role of what you eat and how you live. A healthy gut often applauds a diet low in fats and spices. Steering clear of alcohol, caffeine, and smoking also works wonders. Think of it as giving your digestive system the peace and quiet it deserves!
Dealing with ZES might take some adapting, but with the right approach, folks can get back to focusing on what they love rather than what troubles their tummy.

 Folic Acid and Prenatal Vitamins: What You Need to Know About Medication Interactions in Pregnancy
Folic Acid and Prenatal Vitamins: What You Need to Know About Medication Interactions in Pregnancy
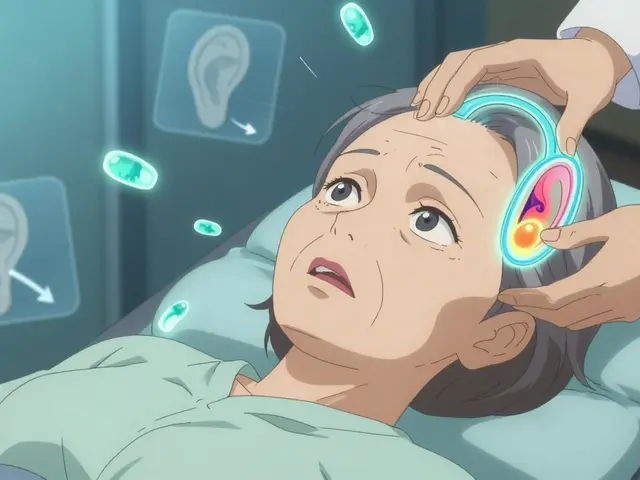 Vertigo and Dizziness: Understanding Inner Ear Disorders and How Vestibular Therapy Helps
Vertigo and Dizziness: Understanding Inner Ear Disorders and How Vestibular Therapy Helps
 How to Involve Grandparents and Caregivers in Pediatric Medication Safety
How to Involve Grandparents and Caregivers in Pediatric Medication Safety
 Social Anxiety Disorder: How Beta-Blockers and Behavioral Therapy Work Together
Social Anxiety Disorder: How Beta-Blockers and Behavioral Therapy Work Together
 Steroid-Induced Acne: Topical Treatments and Lifestyle Fixes That Actually Work
Steroid-Induced Acne: Topical Treatments and Lifestyle Fixes That Actually Work
Adam Craddock
July 18, 2025 AT 11:19This article presents a thorough overview of Zollinger-Ellison Syndrome (ZES), providing a solid foundational understanding of the pathophysiology behind the excessive gastric acid secretion linked to pancreatic neuroendocrine tumors. It's remarkable how these tumors not only escalate acid production but also complicate treatment due to multiple refractory ulcers. I wonder, what are the latest diagnostic markers or imaging modalities that have improved early detection?
Additionally, from a clinical standpoint, managing acid hypersecretion often requires proton pump inhibitors, but considering tumor burden, is surgical intervention the current gold standard, or have minimally invasive therapies advanced significantly? The article's mention of navigating these complexities is crucial for both patients and practitioners.
Kimberly Dierkhising
July 18, 2025 AT 12:19I appreciate the jargon-rich explanation of ZES linked to pancreatic NETs here. The exposition does a commendable job elucidating the biochemical cascade resulting in hypergastrinemia and consequential ulcerogenesis, often refractory to conventional methods. Clinically, the differentiation between sporadic ZES and MEN1-associated cases bears significant implications for management.
Moreover, the diagnostic armamentarium—ranging from gastrin serum assays to provocative tests such as secretin stimulation—plays a pivotal role in accurate detection. Imaging via somatostatin receptor scintigraphy or endoscopic ultrasound enhances tumor localization. This article successfully empowers readers by synthesizing complex clinical data into a digestible format.
Rich Martin
July 18, 2025 AT 13:19Listen up, the whole mess with ZES is one hell of a paradox. You got tumors spitting out gastrin like there's no tomorrow, wrecking the stomach's delicate balance and causing ulcers that just don't quit. It's not just about popping acid reducers like candy; the real problem is the tumors themselves, which seem hellbent on making life miserable.
What's maddening is how rare this condition is, leading a lot of docs to miss it or mistake the symptoms. Makes you wonder how many people are suffering in silence with this shotgun blast of acid demolishing their gut. Can we please ramp up awareness and research instead of treating symptoms in isolation?
Buddy Sloan
July 18, 2025 AT 13:46Wow, this article really hits home. I've seen firsthand how tough ZES can be for patients dealing with chronic ulcers and the stress it places on their quality of life. Managing not only the hyperacidity but also the emotional toll of tumor diagnosis is a complex journey.
One thing that stood out to me is the emphasis on comprehensive management strategies beyond just medications. Support systems and counseling can be just as critical. Anyone out there dealing with ZES: remember, you're not alone and there are communities and resources to lean on!
😊SHIVA DALAI
July 18, 2025 AT 14:12The clinical complexity of Zollinger-Ellison Syndrome as articulated here is nothing short of dramatic. The relentless secretion of acid due to the pancreatic tumors conjures a scenario all too harrowing for patients. Beyond the ulcerative battles, consider the implications of delayed diagnosis—how many lives might be lost or permanently impaired due to lack of early recognition?
This condition demands heightened vigilance by medical professionals and a multidisciplinary approach. The diagnostic nuances must be acknowledged and aggressively pursued. The article gave me chills contemplating the cascading damage unchecked acid can inflict on the gastrointestinal architecture.
Vikas Kale
July 18, 2025 AT 15:09From a biochemical and diagnostic perspective, this overview hits many critical points. The cohesion between gastrin oversecretion, resultant acid hyperproduction, and ulcer formation is textbook. However, the article omits some of the emerging molecular pathways implicated in tumor genesis and progression, which could offer avenues for targeted therapy.
Moreover, somatostatin analogs have shown promise in mitigating hormone secretion and tumor growth, beyond acid control with PPIs. I would have liked to see a deeper dive into these adjunctive therapeutic strategies. Also, do we have consensus on optimal surveillance imaging intervals post-treatment?
😊Deidra Moran
July 18, 2025 AT 16:09Honestly, this piece, while informative, glosses over some deeper, darker undercurrents. Why is it that so many cases of Zollinger-Ellison go undiagnosed, leading to severe outcomes? There's almost a conspiracy of ignorance in play, where pharmaceutical companies profit from symptomatic treatments rather than pushing for actual tumor eradication strategies.
I mean, how convenient that acid reducers flood the market while the root causes get sidestepped. Does anyone else feel like medical institutions are content with keeping patients on lifelong meds instead of tackling the entire tumor problem head-on?
Zuber Zuberkhan
July 18, 2025 AT 17:09Addressing the concerns about underdiagnosis — it's a multifaceted issue. ZES often mimics common gastrointestinal conditions, making clinical suspicion crucial. Enhanced awareness and protocol-driven diagnostic pathways are vital. Clinicians must balance aggressive investigation with prudent clinical judgment to avoid unnecessary testing.
On the therapeutic front, while resection can be curative, metastatic disease calls for multimodal treatment including somatostatin analogs, proton pump inhibitors, and sometimes peptide receptor radionuclide therapy (PRRT). The management is nuanced and evolving constantly.
Tara Newen
July 18, 2025 AT 18:09While I appreciate the scientific depth provided, I must emphasize that the American healthcare system's approach to ZES often falls short in timely diagnosis and equitable care. Nationally, many deserving patients delay care due to systemic barriers, impacting prognosis.
It's essential we advocate for more robust screening protocols in clinical practice, particularly for patients with familial syndromes like MEN1. Only by bolstering national awareness and resource allocation can we aspire to better outcomes for ZES sufferers.
Amanda Devik
July 18, 2025 AT 19:09This thread really underscores how complex and demanding living with ZES can be! For those managing this condition, integrating medical treatment with lifestyle modifications can make a meaningful difference.
Eating smaller meals, managing stress, and vigilant follow-ups empower patients to take control alongside their healthcare providers. Articles like this one offer valuable knowledge that helps demystify an otherwise intimidating diagnosis and foster hope through actionable steps.
Mr. Zadé Moore
July 18, 2025 AT 20:09The jargon is heavy but necessary—understanding the pathophysiology of ZES is not trivial. What frustrates me is the scientific community's slow pace adopting cutting-edge diagnostics and personalized treatment regimens for these patients.
Too often, clinical inertia impedes breakthroughs. We need swift translation of molecular insights into practice. Only then can we move from symptomatic management to true disease modification, potentially even prevention of tumor progression.