When your doctor talks about a new medicine to treat your arthritis, diabetes, or cancer, you might hear the word biosimilar. It sounds technical, maybe even scary. But here’s the truth: biosimilars aren’t new or experimental. They’re well-tested, FDA-approved copies of powerful biologic drugs - and they can help you save money without sacrificing safety or effectiveness.
What’s the difference between a biosimilar and a generic drug?
Most people know generics. They’re the cheaper versions of pills like ibuprofen or metformin. Generics are exact chemical copies. If you break open a generic pill, you’ll find the same molecules as the brand-name version. Biosimilars are different. They’re not copies in the same way. Why? Because biologic drugs aren’t made in a lab with chemicals. They’re made from living cells - human or animal cells grown in controlled environments. These drugs are huge, complex proteins, sometimes with sugar molecules attached. Think of them like a snowflake: no two are exactly alike, even when made by the same company. So a biosimilar isn’t identical to the original biologic. But it’s as close as science can get. The FDA requires proof that it works the same way, has the same side effects, and is just as safe. That’s not easy. It takes years of testing, thousands of lab analyses, and clinical trials with hundreds of patients.How do biosimilars get approved?
The FDA doesn’t just look at the final product. They dig into every step of how it’s made. The cell line used. The fermentation process. The purification methods. Even the way it’s packaged. Tiny changes in any of these steps can affect how the drug works in your body. Before a biosimilar gets approved, the manufacturer must prove:- The molecular structure matches the original biologic almost exactly
- It behaves the same way in lab tests (called bioactivity)
- It’s just as pure - no harmful contaminants
- Clinical studies show it works the same in patients
- Side effects are the same
Are biosimilars safe?
Yes. And the data backs it up. Biosimilars have been used in Europe for over 15 years. Millions of patients have taken them. Studies show no increase in side effects or loss of effectiveness over time. In the U.S., since Zarxio was approved in 2015, more than 30 biosimilars have been approved for conditions like rheumatoid arthritis, Crohn’s disease, psoriasis, and several types of cancer. The American Cancer Society, the Arthritis Foundation, and the FDA all agree: approved biosimilars are as safe and effective as the original biologics. If your doctor says it’s right for you, it’s not a gamble. It’s science.What conditions are treated with biosimilars?
Biosimilars are used for serious, long-term conditions where biologics are the standard treatment:- Rheumatoid arthritis - drugs like adalimumab and infliximab
- Crohn’s disease and ulcerative colitis - same drugs, same results
- Psoriasis - targeting immune system overactivity
- Diabetes - biosimilar insulins like Semglee (insulin glargine)
- Cancer - trastuzumab for breast cancer, bevacizumab for colon cancer
- Eye disease - drugs for macular degeneration
- Chronic kidney disease - to help make red blood cells
How much do biosimilars cost?
Original biologics can cost $10,000 to $20,000 a year. Some even more. Biosimilars typically cost 15% to 30% less. That’s a savings of $1,500 to $6,000 a year. Insurance companies often push for biosimilars because they save money. Some plans require you to try a biosimilar first before they’ll pay for the brand-name drug. That’s not a punishment - it’s a smart cost-control move that still puts your health first. In some cases, the original drug’s price has dropped too, just because biosimilars entered the market. That’s competition working the way it should.What do biosimilar names look like?
You’ll notice something odd when you see the name of a biosimilar. It’s almost the same as the original - but with four extra letters at the end. For example:- Original: adalimumab (Humira)
- Biosimilar: adalimumab-afzb (Cyltezo)
- Original: infliximab (Remicade)
- Biosimilar: infliximab-dyyb (Renflexis)
Can you switch from a biologic to a biosimilar?
Yes. And many people do. Studies show that switching from a brand-name biologic to a biosimilar doesn’t increase side effects or make the treatment less effective. In fact, the Arthritis Foundation says switching is safe and well-studied. Patients who switched for cost reasons didn’t have worse outcomes. But always talk to your doctor first. Never switch on your own. Your provider will check your condition, your history, and whether your insurance allows it.What’s an “interchangeable” biosimilar?
There’s a special category: interchangeable biosimilars. These can be swapped for the original drug at the pharmacy - without your doctor having to approve it each time. Think of it like a generic pill you can pick up off the shelf. The first one approved in the U.S. was Semglee, a biosimilar to insulin glargine (Lantus). It’s now available in pharmacies nationwide. More are expected soon. Interchangeable doesn’t mean “better.” It just means the FDA is confident enough to let pharmacists substitute it without asking the doctor.What should you do as a patient?
If your doctor suggests a biosimilar:- Ask: “Is this a biosimilar? What’s the brand name?”
- Ask: “Has this been used by others with my condition?”
- Ask: “Will my insurance cover it?”
- Ask: “Can I switch from my current drug?”
Final thought: You’re not taking a risk - you’re making a smart choice
Biosimilars aren’t a compromise. They’re a breakthrough. They bring the power of biologic medicine - once only available to those who could afford it - to more people. And they do it without cutting corners. The science is solid. The safety record is strong. The savings are real. If your doctor says a biosimilar is right for you, you’re not settling. You’re choosing smart care.Are biosimilars the same as generic drugs?
No. Generic drugs are exact chemical copies of small-molecule pills, like aspirin or blood pressure meds. Biosimilars are highly similar versions of complex biologic drugs made from living cells. They can’t be exact copies because of their size and structure, but they work the same way and have the same safety profile.
Are biosimilars safe to use?
Yes. The FDA requires rigorous testing before approval, including lab studies, animal tests, and clinical trials with hundreds of patients. Millions of people in Europe and the U.S. have used biosimilars without new or unexpected safety issues. Organizations like the American Cancer Society and the FDA confirm they’re as safe as the original biologics.
Can I switch from my current biologic to a biosimilar?
Yes, many patients do. Studies show switching doesn’t reduce effectiveness or increase side effects. But always talk to your doctor first. They’ll check your medical history and make sure the switch is right for you. Never switch on your own.
Why do biosimilars have strange names with four letters at the end?
Those four letters are a safety feature. They help doctors and pharmacists track exactly which product you’re taking if there’s a side effect or issue. For example, if you’re on infliximab-dyyb, the system knows it’s the biosimilar Renflexis, not the original Remicade. This helps keep everyone safe.
Do biosimilars cost less than the original biologics?
Yes. Biosimilars typically cost 15% to 30% less than the original biologic. That can mean savings of thousands of dollars a year. Some insurance plans require you to try a biosimilar first. In some cases, the original drug’s price has even dropped because of biosimilar competition.
What conditions can be treated with biosimilars?
Biosimilars treat serious chronic conditions including rheumatoid arthritis, Crohn’s disease, psoriasis, type 1 and type 2 diabetes (with insulin), certain cancers (like breast and colon cancer), macular degeneration, and kidney disease. They’re used when biologics are the standard treatment.
What’s the difference between a biosimilar and a bioidentical?
A bioidentical is made using the exact same production process as the original biologic - same cells, same steps, same additives. It’s essentially the same product made by a different company. A biosimilar is highly similar but made with a different process. Both are safe and approved, but biosimilars are more common because they’re easier to develop under current rules.
Will my insurance cover a biosimilar?
Most do. Many insurance plans encourage or require biosimilars because they’re cheaper. Some even require you to try a biosimilar before they’ll pay for the brand-name biologic. Check your plan’s formulary or ask your pharmacist. If your current drug is too expensive, a biosimilar could be a better option.
If you’re on a biologic and worried about cost, ask your doctor about biosimilars. You might be surprised how much you can save - without giving up anything in quality or care.
 From Tradition to Innovation: How Yin Chen Dietary Supplement is Changing Lives
From Tradition to Innovation: How Yin Chen Dietary Supplement is Changing Lives
 Cefaclor in the ICU - Uses, Dosing, and Key Considerations
Cefaclor in the ICU - Uses, Dosing, and Key Considerations
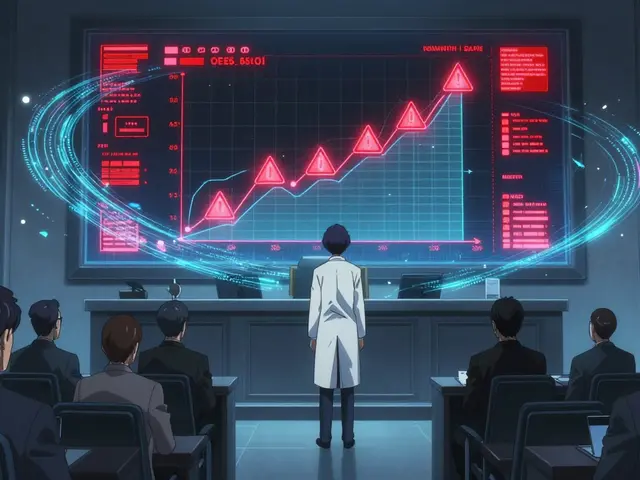 Drug Withdrawals and Recalls: Why Medications Get Removed from the Market
Drug Withdrawals and Recalls: Why Medications Get Removed from the Market
 Buy Cheap Generic Amoxicillin Online - Safe Guide 2025
Buy Cheap Generic Amoxicillin Online - Safe Guide 2025
Sangram Lavte
December 8, 2025 AT 09:42Biosimilars are a game changer for people like me who’ve been on Humira for years. The cost difference is insane - I’m saving over $5k a year without any drop in effectiveness. My rheumatoid arthritis hasn’t flared up since I switched.
Just make sure your doctor confirms it’s approved for your condition. No drama, just science.
Oliver Damon
December 9, 2025 AT 07:01The structural complexity of biologics makes biosimilars a triumph of analytical biochemistry. Unlike small-molecule generics, you’re not just replicating a molecular formula - you’re reverse-engineering a dynamic, post-translationally modified protein landscape with cellular context preserved.
The FDA’s comparability protocols are among the most rigorous in pharmacology. What we’re seeing isn’t just cost arbitrage - it’s regulatory science reaching parity with biological reality.
Kurt Russell
December 11, 2025 AT 05:03THIS IS HUGE. If you’re scared to switch because you think it’s ‘cheap stuff’ - STOP. You’re not getting a discount version, you’re getting the SAME MEDICINE at a fair price.
My cousin switched from Remicade to Renflexis for Crohn’s - same results, same side effects, same life. Now she’s not choosing between rent and her meds.
Share this with anyone who’s afraid. This isn’t just medicine - it’s justice.
Stacy here
December 12, 2025 AT 21:01Wait… so the government and Big Pharma are letting cheaper versions of life-saving drugs enter the market? That doesn’t add up.
Who’s really behind this? Are the four-letter suffixes really for safety… or are they tracking us? I read somewhere that the FDA gets funding from the same companies that make these drugs.
And why are they pushing this now? Coincidence that it’s right after the Inflation Reduction Act? Something’s off. I’m sticking with Humira. I’ve seen what happens when you trust the system.
Louis Llaine
December 12, 2025 AT 21:11So let me get this straight - you’re telling me we spent 20 years paying $20k/year for a drug… and now we find out it’s basically just a fancy copy?
And the reason we didn’t know this sooner was because… profit?
Wow. Just… wow. I feel so smart for not falling for this.
Jane Quitain
December 14, 2025 AT 05:04i just switched to the biosimilar for my insulin and omg it’s been so much better?? my blood sugar is way more stable and i’m not broke anymore 😭 i didn’t think it would work but my doc said it was totally safe and i’m so glad i listened
also i’m not a doctor but i read a lot of articles so… yeah
Kyle Oksten
December 15, 2025 AT 16:16The fact that people still question biosimilar safety reveals how little public understanding exists about biopharmaceutical development.
It’s not about trust - it’s about evidence. The clinical data from Europe alone spans over 15 years and millions of patient-years. If there were hidden risks, they’d be visible by now.
What’s being promoted here isn’t ideology - it’s pharmacovigilance at scale. The system is working.
Sam Mathew Cheriyan
December 16, 2025 AT 11:25lol biosimilars? more like biowhatever. they say it’s the same but i bet the cell lines are from some chinese lab and the sugar molecules are fake. i mean, why would they make it cheaper if it wasn’t sketchy?
my uncle in delhi took one and now he’s got weird rashes. not saying it’s this, but… you know? just saying.
also i think the four letters are for the CIA. they’re watching us.