Most people assume that if two pills have the same active ingredient, they work the same way. But what if the problem isn’t the drug itself - it’s what’s around the drug? In generic medications, the inactive ingredients - the fillers, dyes, preservatives, and binders - can vary wildly between brands, and when you’re taking multiple generics at once, those differences can add up in surprising - and sometimes dangerous - ways.
What Are Inactive Ingredients, Really?
Inactive ingredients, also called excipients, aren’t meant to treat anything. They’re there to make the pill hold its shape, dissolve at the right time, taste better, or last longer on the shelf. Common ones include lactose, propylene glycol, tartrazine (a yellow dye), and bisulfites. But here’s the catch: every generic manufacturer picks their own mix. Two versions of the same generic blood pressure pill might contain completely different excipients - even though they both say "amlodipine 10 mg" on the label.
The FDA doesn’t require generic drugs to match the inactive ingredients of the brand-name version or even each other. All they need to prove is that the active ingredient gets into your bloodstream within 80-125% of the original drug’s levels. That’s it. The rest? Up to the manufacturer.
Why This Matters When You Take Multiple Generics
Think of your medication routine like a puzzle. Each pill is a piece. Most pieces fit fine alone. But when you stack them together, the edges might start to fray.
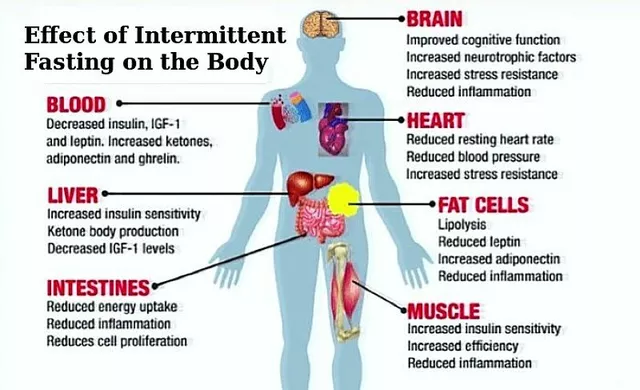
A 2020 study found that someone taking 10 prescriptions daily ingests an average of 2.8 grams of inactive ingredients every day. That’s more than half a teaspoon of non-medicinal chemicals - and it’s not just one type. You could be getting lactose from your thyroid pill, propylene glycol from your liquid painkiller, and tartrazine from your antidepressant - all on the same day.
For most people, this is harmless. But for those with sensitivities, it’s a different story.
- Lactose affects 65% of the global population to some degree. Even small amounts - 1-2 grams - can trigger bloating, cramps, or diarrhea in sensitive people.
- Propylene glycol is in nearly half of all liquid medications. It can cause headaches, nausea, or even kidney stress in high doses.
- Tartrazine, a common yellow dye, triggers allergic reactions in about 4% of people, including hives and asthma flare-ups.
- Bisulfites, used as preservatives, can cause severe breathing problems in 5-10% of asthmatics.
Now imagine you’re on three different generic pills - each with 50 mg of lactose. That’s 150 mg per dose. Multiply that by three times a day? You’re hitting 450 mg daily. For someone with mild lactose intolerance, that’s enough to cause daily discomfort. For someone with severe intolerance? It could mean missed work, ER visits, or worse.
Real Cases: When "Harmless" Ingredients Cause Real Problems
It’s not theoretical. In 2021, a 68-year-old woman in Ohio was hospitalized after switching to generic versions of her medications. She’d been on brand-name levothyroxine for years with no issues. When her insurance switched her to a cheaper generic, she started having heart palpitations and fatigue. Her doctor blamed stress. But when her pharmacist checked the ingredients, they found the new generic used a different binder that slowed absorption - dropping her thyroid levels by 30%. She wasn’t reacting to the drug. She was reacting to the formulation.
On Reddit’s r/pharmacy, users share stories like this regularly. One person, u/MedSafetyWatcher, described developing severe diarrhea after being prescribed three different generic painkillers - all containing lactose. He’d taken each one alone before with no problem. But together? The cumulative dose pushed him past his tolerance.
These aren’t rare. The FDA’s Adverse Event Reporting System logged over 1,200 cases from 2020-2023 where patients reported "unexpected gastrointestinal distress," "unexplained skin reactions," or "reduced medication effectiveness" - all linked to inactive ingredient combinations.

Brand vs. Generic: The Hidden Trade-Off
Brand-name drugs usually stick to the same excipients across batches. Generics? Not so much. One manufacturer might use cornstarch. Another might use potato starch. One might use a dye. Another might be dye-free. And because generics are cheaper - often 80-85% less expensive - insurers push them hard.
But here’s the problem: switching between generics isn’t always safe. A 2022 FDA review found cases where patients taking generic antiepileptic drugs had 15-20% lower peak blood levels due to excipient differences. That’s enough to trigger seizures in someone with epilepsy.
Even drugs with narrow therapeutic windows - like digoxin for heart failure or warfarin for blood thinning - can become unpredictable when the inactive ingredients change. A tiny shift in how fast the drug dissolves can mean the difference between effective treatment and life-threatening toxicity.
What Pharmacists Are Starting to Do About It
Pharmacists are on the front lines. In 2023, the American Pharmacists Association updated its guidelines to warn about "cumulative excipient exposure" in patients on multiple medications. They now recommend:
- Checking every medication’s full inactive ingredient list - not just the active one.
- Using databases like the FDA’s Inactive Ingredient Database or DailyMed to compare formulations.
- Calculating daily exposure to known allergens or irritants.
For example: if a patient is lactose intolerant, the pharmacist adds up all the lactose from every pill. If it’s over 1-2 grams per day, they look for alternatives. Some generics use mannitol or dextrose instead of lactose. It takes time, but it works.
A 2021 study in the American Journal of Health-System Pharmacy found that 78% of patients who switched to compatible generic formulations saw their symptoms disappear.
Why This Isn’t Common Knowledge
Most patients never see the full list of ingredients. Only 63% of medication package inserts fully disclose inactive ingredients, according to a 2021 JAMA study. Labels often say "other ingredients" and list nothing else. Even some pharmacists don’t know how to access the full data.
Manufacturers aren’t required to report excipient interactions to the FDA. And until recently, the agency didn’t track them. The FDA still claims that differences in inactive ingredients "have not been shown to affect safety or effectiveness" in most cases. But that’s based on broad population studies - not individual sensitivities.
Meanwhile, the European Medicines Agency took a stronger stance in 2024: manufacturers must now justify using excipients that affect more than 0.1% of the population. The U.S. is catching up - but slowly.

What You Can Do Right Now
If you’re on multiple generic medications, here’s what to do:
- Ask your pharmacist for the full list of inactive ingredients in each pill. Don’t settle for "it’s the same as the brand." It’s not.
- Look up your meds on DailyMed (dailymed.nlm.nih.gov) or the FDA’s Inactive Ingredient Database. Search by NDC code - it’s on the bottle.
- Track symptoms. Did your stomach upset start after switching to a new generic? Did your rash appear after adding a new medication? Write it down.
- Request alternatives. If you’re sensitive to lactose, ask for a lactose-free version. Same with dyes, gluten, or propylene glycol. Many generics offer them.
- Use one pharmacy. That way, your pharmacist can see all your meds in one system and spot overlaps.
It’s not about avoiding generics. They save billions and make medicine accessible. But it’s about being smart about which ones you take - especially when you’re on more than one.
The Future: AI, Transparency, and Change
In January 2024, the FDA launched the Inactive Ingredient Transparency Initiative. By December 2025, all manufacturers must list every excipient in digital product labeling. That’s a big step.
Tools like MedCheck AI, released in late 2023, can now scan your prescription list and flag potential excipient conflicts with 89.7% accuracy. Hospitals are starting to use them. Eventually, they’ll be in your pharmacy app.
By 2026, the European Union plans to require "excipient interaction risk assessments" for drugs commonly taken together - like blood pressure pills and diuretics. The U.S. may follow.
But until then, the power is in your hands - and your pharmacist’s.
Bottom Line
Generic drugs are safe - mostly. But they’re not all the same. When you take several at once, the invisible ingredients can pile up and cause real problems. You don’t need to avoid generics. You just need to know what’s in them. Talk to your pharmacist. Check the labels. Ask for alternatives. Your body will thank you.
 Buy Cheap Generic Coumadin Online - Safe Guide 2025
Buy Cheap Generic Coumadin Online - Safe Guide 2025
 The Impact of Seasonal Changes on Vitamin D Levels
The Impact of Seasonal Changes on Vitamin D Levels
 Zovirax Cream vs Topical Antiviral Alternatives: A Detailed Comparison
Zovirax Cream vs Topical Antiviral Alternatives: A Detailed Comparison
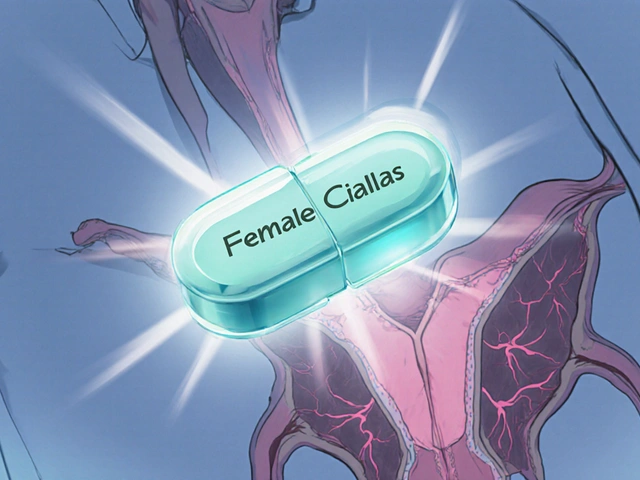 Female Cialis (Tadalafil) vs. Alternatives: Pros, Cons & Best Choices
Female Cialis (Tadalafil) vs. Alternatives: Pros, Cons & Best Choices
 Understanding Zollinger-Ellison Syndrome and Its Link to Pancreatic Tumors
Understanding Zollinger-Ellison Syndrome and Its Link to Pancreatic Tumors
Nnaemeka Kingsley
December 2, 2025 AT 02:27wait so my stomach issues since last year might be from my pills and not my diet? i always thought i was just bad with dairy but now i check my meds and three of em got lactose in em. whoa.
Jaswinder Singh
December 2, 2025 AT 17:08you people are freaking out over sugar and dyes while real killers like opioids and benzodiazepines are handed out like candy. this is a distraction tactic by big pharma to make you feel guilty for using generics. get real.
Bee Floyd
December 4, 2025 AT 06:55this is one of those posts that makes you pause and think - like, wow, we’re all just swallowing invisible stuff every day and assuming it’s fine. i never checked my meds’ ingredients before. now i’m gonna pull out my bottle of metformin and read the tiny print like it’s a treasure map. 🕵️♂️
Jeremy Butler
December 4, 2025 AT 18:13It is an epistemological imperative to interrogate the ontological assumptions underpinning pharmaceutical excipient standardization. The FDA's regulatory framework, predicated upon bioequivalence metrics, neglects the phenomenological experience of the individual patient, thereby constituting a systemic epistemic injustice.
Courtney Co
December 5, 2025 AT 23:15OMG I had no idea this was happening to me!! I’ve been so tired and bloated for months and my doctor just said ‘you’re aging’ but now I’m crying because I think it’s my meds!! I have like 7 pills a day and I just found out one has tartrazine and another has propylene glycol!! I’m so mad!!
Eric Vlach
December 7, 2025 AT 03:27my pharmacist just told me to switch to a different generic for my blood pressure med because the one i had had a dye that makes my skin itch. i didn’t even know dyes were in pills. now i ask for the full list every time. it’s not hard just ask. seriously
Souvik Datta
December 7, 2025 AT 12:28Science has always been about understanding the whole system, not just the active component. The human body is a complex ecosystem - and we treat medication like it's a bullet, when in reality it's a key that must fit multiple locks. The excipients? They're the rust, the dirt, the misalignment. We ignore them at our peril.
Priyam Tomar
December 9, 2025 AT 01:32everyone’s acting like this is new news. i’ve been warning people for years that generics are a crapshoot. if you’re on more than 3 meds you’re basically doing a chemical cocktail experiment on yourself. and the FDA doesn’t care. they’re just here to make sure the pills don’t explode.
Jack Arscott
December 10, 2025 AT 19:40so i checked my meds and one of my antidepressants has lactose?? 😳 i’m lactose intolerant but i never thought about pills. i’m switching to the lactose-free version tomorrow. thanks for the wake up call 🙏💊
Irving Steinberg
December 12, 2025 AT 12:16why are we even talking about this like it’s a big deal. just take the brand name if you’re that worried. it’s not like you can’t afford it. people need to stop being so dramatic about their stomachs
Lydia Zhang
December 13, 2025 AT 03:39my pharmacist already told me this last year. i just didn’t care enough to change anything.