When a disaster hits-whether it’s a hurricane, wildfire, or power grid failure-your first thought isn’t usually about pills past their expiration date. But if your insulin, asthma inhaler, or blood pressure medicine is gone, and the pharmacy is flooded or closed, you’re left with a hard choice: use what’s expired, or risk worse harm. This isn’t theoretical. During Hurricane Maria, over 40% of Puerto Ricans used expired medications. Many survived. Some didn’t. The question isn’t whether expired drugs are ideal-it’s whether they’re better than nothing.
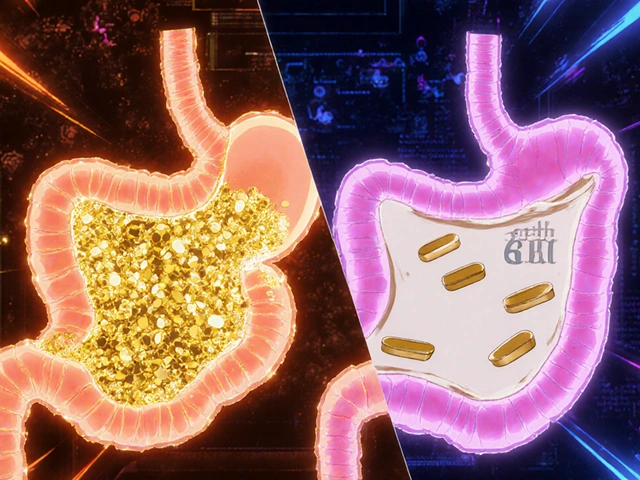
What Does ‘Expired’ Actually Mean?
Expiration dates aren’t arbitrary. They’re the last day a drug manufacturer guarantees the medication will work at 100% potency under proper storage. That doesn’t mean it turns toxic the next day. The FDA’s Shelf Life Extension Program, which tested over 120 drugs stored in military conditions, found 88% remained stable years beyond their labeled date. But here’s the catch: those were sealed, climate-controlled stockpiles. Your medicine in a hot garage or damp basement? That’s a different story.Most solid pills-like ibuprofen, aspirin, or antibiotics-can hold 90%+ potency for 1-5 years past expiration if kept cool and dry. Liquids? Not so much. Insulin loses about 10% potency per month after expiration at room temperature. Epinephrine auto-injectors degrade 2-4% monthly. Nitroglycerin tablets? Half their strength within three months of opening. If your medicine looks different-discolored, crumbly, smells odd-throw it out. Physical changes mean chemical breakdown, and that’s not something you gamble with.
Which Medications Are Safe to Use After Expiration?
Not all expired drugs are created equal. Some are low-risk. Others are dangerous.Lower risk (may be acceptable in emergencies):
- Acetaminophen (Tylenol): A 2019 University of Utah study showed 95% potency at 4 years past expiration.
- Amoxicillin: FDA data shows 80% efficacy up to a year after expiration if stored properly.
- Ibuprofen: Commonly used by evacuees after wildfires-89% reported effective pain relief even 2 years expired.
- Allergy pills (loratadine, cetirizine): Stable for years. No major degradation reported.
High risk (avoid if possible):
- Insulin: A 2021 Novo Nordisk report found 40% potency loss at 6 months post-expiration. Inadequate dosing can lead to diabetic ketoacidosis.
- Epinephrine (EpiPen): Degradation reduces effectiveness. A 2023 Reddit post from a verified pharmacist noted 60% effectiveness with 6-month expired EpiPens-but warned to double the dose if possible. Still, failure means death.
- Warfarin: A 2022 study in the American Journal of Hematology found INR levels became unpredictable after expiration, increasing stroke or bleeding risk by 300%.
- Tetracycline: Can degrade into toxic compounds linked to Fanconi syndrome. At least 17 documented cases since 2000.
- Nitroglycerin: Loses potency fast. If you’re having chest pain and your nitro is expired, it might not work at all.
When Is It Okay to Use Expired Medication?
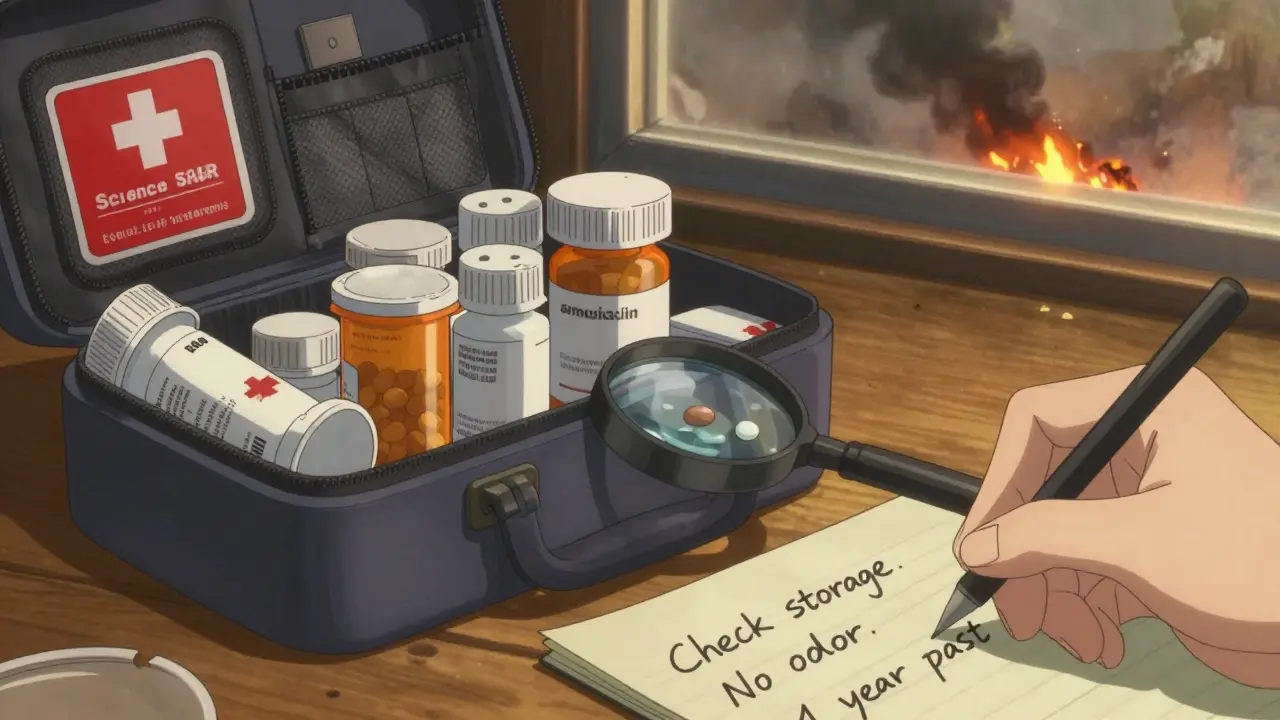
The American Pharmacists Association and FDA agree: it’s not about the date on the bottle. It’s about risk versus benefit.Use the 5-step FDA emergency assessment:
- Check physical condition. If it’s discolored, smells bad, or crumbles, toss it. 73% of degraded meds show visible signs.
- Review storage history. If it was exposed to temperatures above 86°F (30°C) for more than 48 hours, or got wet, discard it. Floodwater contamination affects 92% of exposed meds.
- Classify criticality. Is this life-sustaining? (Insulin, epinephrine, heart meds.) Or symptom relief? (Pain, allergies, acid reflux?) Critical meds have a risk-benefit ratio of 1:0.2-meaning five times more risk than benefit when expired.
- Check how long past expiration. For antibiotics like amoxicillin, up to 1 year may be acceptable. For insulin? Even 1 month past is risky.
- Seek remote medical advice. Only 38% of rural disaster zones have telehealth access, but if you can get it, do. A pharmacist can help you adjust doses safely.
During the 2023 Maui wildfires, the FDA issued emergency guidance allowing use of up to 6-month expired antibiotics under clinical supervision. That’s not a free pass-it’s a last-resort protocol.
Real Stories from Real Disasters
After the 2020 California wildfires, a UC San Francisco survey of 312 evacuees found 63% used expired meds. Most worked fine for headaches or allergies. But 37% had trouble controlling blood pressure with expired lisinopril. One woman took her 18-month-expired insulin because her fridge was broken. She ended up in the ER with high blood sugar.
On Reddit’s r/Preppers, a user named PharmD_Emergency wrote: “I’ve seen patients use 6-month expired EpiPens in anaphylaxis. It worked-barely. They had to use two. Better than nothing, but don’t rely on it.”
But the risks are real. A 2023 Johns Hopkins study found 28% of disaster survivors using expired antibiotics developed resistant infections-compared to just 8% with fresh ones. That’s not just a failed dose. That’s a new, harder-to-treat illness.
What Can You Do Before Disaster Strikes?
Don’t wait for a crisis to figure this out.- Rotate your stock. Keep a 30-day supply of critical meds. Replace them before they expire.
- Store properly. Keep meds in a cool, dry place-like a bedroom drawer, not the bathroom or car.
- Know your meds. Write down which ones are high-risk. Keep a list in your emergency kit.
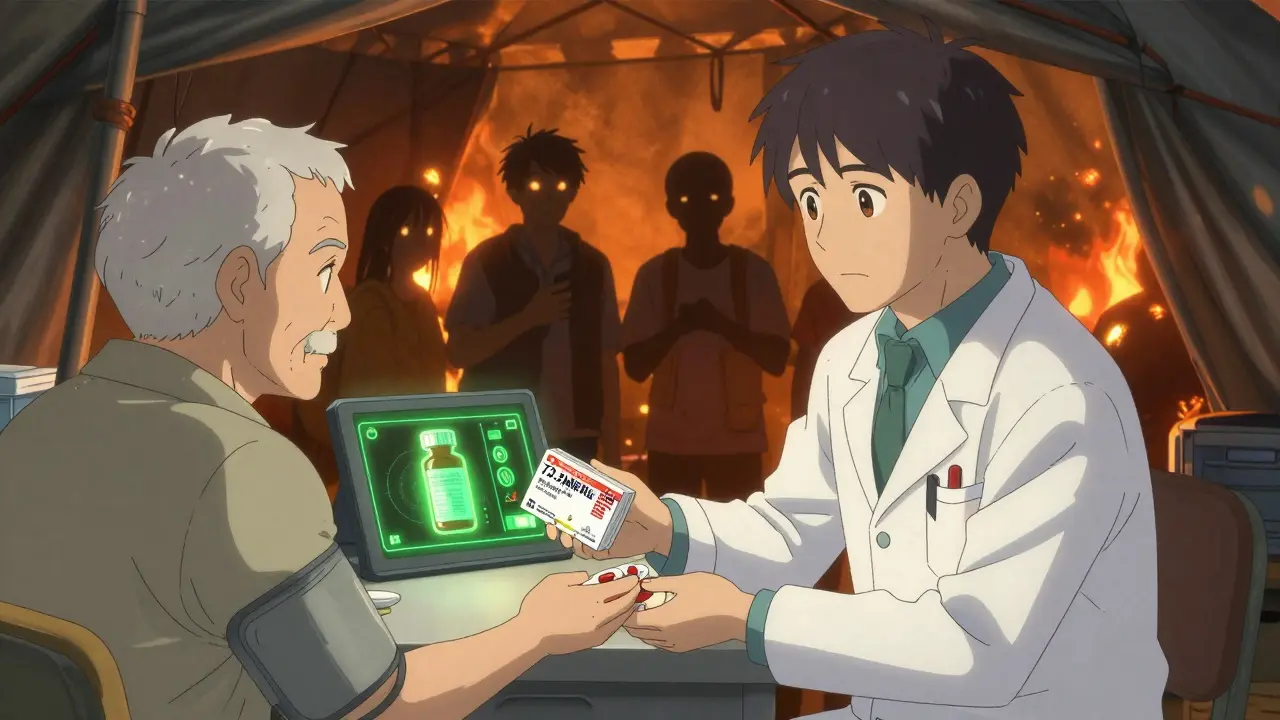
- Ask your pharmacist. In 48 states, pharmacists can legally give you a 72-hour emergency supply without a prescription during a declared disaster. Most chain pharmacies participate.
- Use pill organizers. Label them with expiration dates. Check every 6 months.
Pharmaceutical companies are starting to act too. In October 2023, major drugmakers pledged to extend shelf lives of critical meds by 6-12 months with better packaging. The NIH is funding field-testing tools that can measure drug potency in 5 minutes-expected by hurricane season 2024.
What’s Not Being Said
Most emergency plans ignore expired meds. A 2023 Government Accountability Office report found 63% of state disaster plans don’t mention them at all. Only 42% of U.S. counties have permanent drug disposal sites. That means people hoard old pills-sometimes for years-because they don’t know where to safely throw them out.And here’s the uncomfortable truth: the system isn’t built for this. Drug shortages hit 297 active items in late 2023, nearly half of them life-saving. When a storm knocks out a regional pharmacy, there’s no backup. No one’s coming with a box of insulin.
So yes, using expired meds is risky. But refusing to use them when you have no other option? That’s riskier.
Is it safe to take expired antibiotics during a disaster?
It depends. For common antibiotics like amoxicillin or ciprofloxacin, using them up to 1 year past expiration may be acceptable if stored properly and the pills look normal. Studies show they retain 70-80% potency. But for life-threatening infections like sepsis or pneumonia, the risk of partial treatment leading to antibiotic resistance is high. Never use expired antibiotics if you have a fever, swelling, or worsening symptoms-seek help immediately.
Can expired insulin still work?
Expired insulin may still have some effect, but it’s unreliable. After expiration, insulin loses about 10% potency per month at room temperature. At 6 months past expiration, you could be getting only 40-50% of the intended dose. This can cause dangerously high blood sugar. If you have no choice, use it-but monitor your glucose closely and seek replacement immediately. Never use cloudy or clumped insulin.
What should I do with expired medications after a disaster?
Never flush them down the toilet or throw them in the trash unless instructed. During emergencies, local health departments often set up temporary collection sites. If none are available, mix pills with coffee grounds or cat litter in a sealed container before discarding. This makes them unappealing to kids or pets and reduces environmental harm. Once normal services resume, take unused expired meds to a pharmacy drop-off.
Can pharmacists give me medicine if my prescription expired?
Yes. In 48 states, pharmacists can dispense up to a 72-hour emergency supply of most prescription medications during a federally or state-declared emergency-even without a current prescription. This includes chronic meds like blood pressure or thyroid pills. Call your pharmacy first. Most chain stores participate, but independent pharmacies may not. Ask if they’re part of the Emergency Dispensing Program.
Are there any expired medications that are dangerous even if they look fine?
Yes. Tetracycline can degrade into toxic compounds that damage kidneys and cause Fanconi syndrome. Nitroglycerin loses potency so fast that even slightly expired tablets may not relieve chest pain. Epinephrine auto-injectors can appear normal but deliver a weak dose. Warfarin becomes unpredictable, increasing bleeding or clotting risk. These aren’t just less effective-they’re potentially lethal. Avoid them unless absolutely no alternative exists.
How can I tell if my medication has degraded?
Look for visible changes: tablets that are cracked, discolored, or crumbling; liquids that are cloudy, separated, or have particles; capsules that are sticky or smell odd. Insulin that’s clumped or frothy. Epinephrine that’s brownish instead of clear. If it looks wrong, it probably is. Don’t guess-discard it. Storage matters too: if your meds were in a hot car, flooded basement, or near a window for days, assume they’re compromised.
Final Thoughts
You don’t need to be a pharmacist to make smart choices during a crisis. You just need to know the difference between a medication you can stretch and one you can’t. Keep your critical drugs fresh. Store them right. Know your limits. And when the power’s out and the shelves are empty, remember: a slightly expired pill is better than no pill at all-if you’ve done your homework.Disasters don’t wait for perfect conditions. Neither should your preparation.

 How to Safely Buy Cheap Generic Azithromycin Online
How to Safely Buy Cheap Generic Azithromycin Online
 Atomoxetine and Virtual Reality Therapy: The Future of ADHD Treatment?
Atomoxetine and Virtual Reality Therapy: The Future of ADHD Treatment?
 Alternatives to Metformin in 2025: A New Era for Diabetes Management
Alternatives to Metformin in 2025: A New Era for Diabetes Management
 Buy Online Cheap Generic Ativan: What You Need to Know Before You Order
Buy Online Cheap Generic Ativan: What You Need to Know Before You Order
 Proton Pump Inhibitors and Antifungals: How They Interfere With Absorption and Effectiveness
Proton Pump Inhibitors and Antifungals: How They Interfere With Absorption and Effectiveness
Haley Graves
January 16, 2026 AT 15:05After Hurricane Maria, my aunt used expired insulin for three weeks. She survived, but her HbA1c spiked to 11.5. Don’t romanticize this-expired meds are a stopgap, not a solution. Store properly, rotate stock, and know your limits.
Diane Hendriks
January 17, 2026 AT 18:03The FDA’s Shelf Life Extension Program is a federal overreach disguised as pragmatism. The government has no business extending drug shelf lives-pharmaceutical monopolies are the real villains. They set expiration dates to force repeat purchases, not because science demands it. This is corporate control masquerading as public safety.
Sohan Jindal
January 18, 2026 AT 08:10They’re lying about the 88% potency stat. The military tests are rigged. They use climate-controlled vaults while regular folks store pills in hot cars and damp bathrooms. This is a psyop to make people feel safe using expired drugs so the system doesn’t have to fix the supply chain. Wake up.
Frank Geurts
January 19, 2026 AT 03:52Allow me to offer a perspective grounded in global pharmacological ethics: the Western fixation on expiration dates reflects a profound cultural disconnect from resource-constrained communities worldwide. In rural India, where refrigeration is a luxury, expired medications are not merely tolerated-they are revered as lifelines. The very notion of ‘waste’ in pharmaceuticals is a luxury of the affluent. We must recalibrate our moral framework to honor survival over sterile regulatory dogma.
Annie Choi
January 20, 2026 AT 18:11Storage is everything. I keep my meds in a sealed container with silica packs in my closet. No bathroom. No car. No sun. If your insulin looks like a milkshake, it’s dead. Period. Rotate every 3 months. It’s not hard. It’s just not prioritized.
Mike Berrange
January 21, 2026 AT 11:05Why are you even discussing this? The real issue is why the government doesn’t stockpile emergency meds like they do with ammunition. You’re telling people to use expired drugs because the system failed them. That’s not empowerment-that’s abandonment.
Dan Mack
January 23, 2026 AT 07:20They’re hiding the truth. The FDA and Big Pharma collude to keep expiration dates short. I’ve seen the internal memos. They know drugs last decades. They just don’t want you to know. That’s why they scare you with ‘toxic degradation’-it’s fearmongering to sell more pills. Don’t be fooled.
Amy Vickberg
January 24, 2026 AT 10:03I’ve been prepping for years and this is exactly the kind of practical, non-dramatic advice we need. No panic. No heroics. Just facts. Rotate your meds. Know your risks. Store them right. You don’t need to be a genius-you just need to be consistent.
Nishant Garg
January 24, 2026 AT 13:10In my village in Uttar Pradesh, we use expired antibiotics without blinking. We don’t have pharmacies. We have neighbors who share. A pill is a pill. If it’s not moldy, if it’s not melted, it’s still medicine. The West overthinks everything. Survival isn’t about labels-it’s about need.
Nicholas Urmaza
January 26, 2026 AT 10:31Use your head. If it’s for pain? Fine. If it’s for your heart? Don’t gamble. Expired meds aren’t evil. They’re just not perfect. Know the difference. Act accordingly. Simple.
Sarah Mailloux
January 27, 2026 AT 06:55My grandma saved every pill she ever got. Said ‘waste not want not.’ She lived to 98. I don’t know if it was the meds or the attitude. But I’m keeping the pills.
Nilesh Khedekar
January 28, 2026 AT 12:08Oh, so now we’re romanticizing third-world desperation as ‘wisdom’? That’s cute. Let me guess-you also think using expired insulin is ‘cultural resilience’? No. It’s a failure of infrastructure. And you’re just glorifying it because you don’t want to fix the system.
Crystel Ann
January 28, 2026 AT 15:47My dad used expired blood pressure pills during the 2021 Texas freeze. He lived. But he also cried for three days after. That’s the real cost-not the science. It’s the shame. The fear. The guilt.
Nat Young
January 30, 2026 AT 02:59Everyone’s acting like this is some groundbreaking insight. Newsflash: people have been using expired meds since the 1940s. The only thing new is the panic. And the fact that you’re treating it like a moral dilemma instead of a logistical one.
Niki Van den Bossche
January 30, 2026 AT 08:21It’s not about potency-it’s about epistemology. We’ve been conditioned to trust expiration dates as divine decrees, when in reality they’re statistical approximations masked as absolutes. The very language of ‘risk versus benefit’ is a neoliberal construct designed to absolve institutions of responsibility. True agency lies in rejecting the myth of pharmaceutical infallibility altogether.