When a teenager starts taking ADHD medication, parents often feel relief-finally, their child can focus in class, stop blurting out answers, or finish homework without constant nagging. But that relief can quickly turn to worry when the child stops eating, loses weight, or stops growing like they used to. These aren’t rare side effects. They’re common. And they need to be tracked, not ignored.
Why ADHD Medications Affect Growth and Appetite
Stimulant medications like methylphenidate (Ritalin, Concerta) and amphetamines (Adderall, Vyvanse) work by boosting dopamine and norepinephrine in the brain. That helps with focus and impulse control. But those same chemicals also affect the hypothalamus-the part of the brain that regulates hunger, sleep, and metabolism. The result? Appetite drops. Meals get skipped. Calories disappear.Studies show 50 to 80% of teens on these meds experience noticeable appetite suppression. It’s not just "not hungry." It’s often a full-blown lack of interest in food during school hours. One 14-year-old on Vyvanse eats one granola bar at lunch and doesn’t touch anything until after 5 p.m., when the medication wears off. That’s not unusual. That’s the pattern.
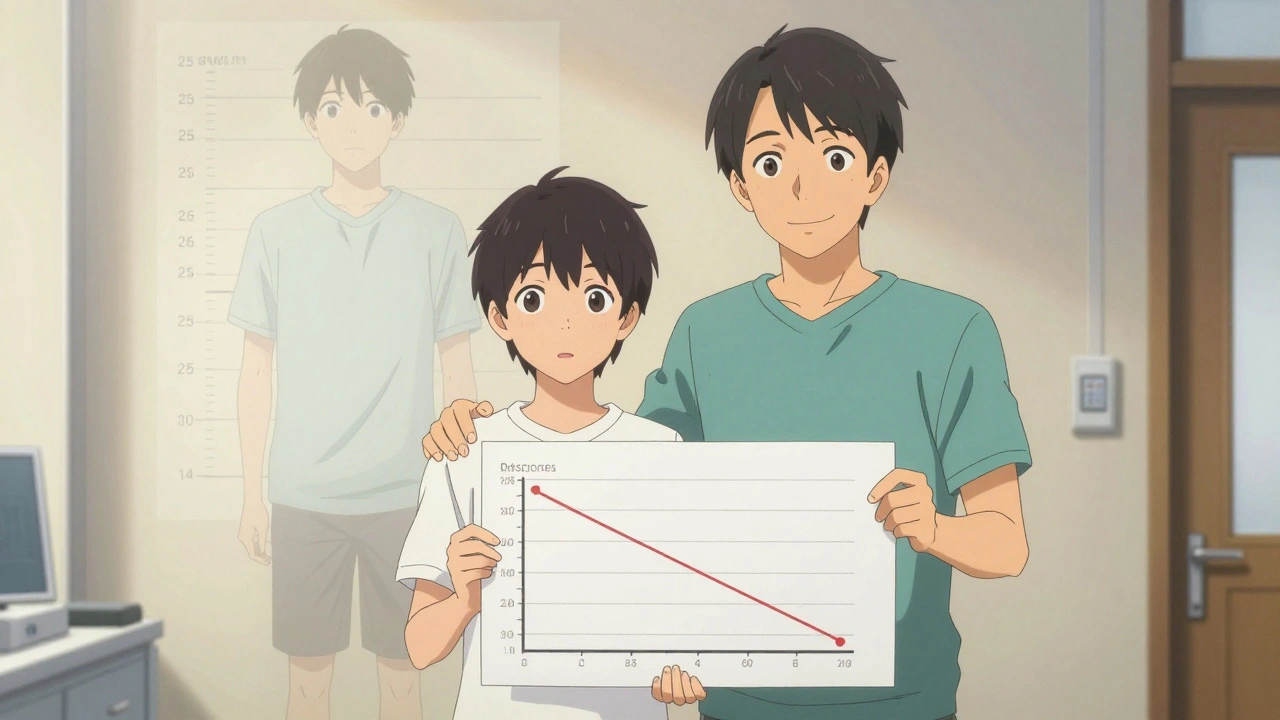
Growth is affected too. Long-term use of stimulants is linked to a small but measurable reduction in height. The data shows teens on these meds may end up 0.5 to 1 inch shorter than they would have been without treatment. That sounds small, but for a teenager already on the lower end of the growth curve, it matters. The most significant impact happens in the first 12 to 24 months. After that, the slowdown tends to stabilize.
How Much Growth Is Really Lost?
Not all studies agree. Some show a clear 2.5 cm (about 1 inch) reduction in adult height among teens who stayed on medication continuously. Others, like a 2017 study, found no difference in final height between medicated and non-medicated teens. So what’s going on?The key is duration and timing. The 2023 follow-up to the famous MTA study found that 89% of teens who experienced early growth delays caught up to their genetic potential by age 25. Only 11% had persistent shortening-more than 1.5 cm. That’s important. It means most of the time, the body catches up. But catching up doesn’t happen if you’re still on the same high dose, year after year, without breaks.
Extended-release formulations like Concerta or Adhansia XR don’t cause more suppression than immediate-release versions. But amphetamines (like Adderall and Vyvanse) tend to have a slightly stronger effect on growth than methylphenidate. A 2019 meta-analysis found amphetamines led to 1.7 cm less height after three years, compared to 1.1 cm for methylphenidate. That’s not a huge difference, but for a teen already struggling to grow, it can tip the scale.
Appetite Loss: More Than Just Skipping Lunch
Appetite suppression isn’t just about eating less. It’s about nutritional gaps. A teen on medication might skip breakfast because they’re not hungry, eat a tiny lunch, and then snack heavily after school-often on chips, candy, or sugary drinks. That’s not nutrition. That’s calorie dumping.One parent on Reddit described her son’s day: "He eats one granola bar at school. Sometimes skips lunch. Then at 6 p.m., he eats enough for three people." That’s not a healthy pattern. It leads to poor nutrient intake during the day, blood sugar spikes at night, and long-term risks for metabolic health.
CHADD’s 2022 survey found 19% of parents reported their child lost more than 10% of their body weight on stimulants. One girl dropped from the 50th to the 15th percentile in weight over eight months. Her pediatrician switched her to atomoxetine (Strattera), a non-stimulant. Her weight stabilized within three months.
Non-stimulants like Strattera, guanfacine, or clonidine don’t suppress appetite the same way. But they’re also less effective-about 30 to 40% less-for core ADHD symptoms. So it’s a trade-off: better appetite, worse focus.

Monitoring Growth: What Doctors Should Be Doing
The American Academy of Pediatrics says this clearly: Measure height and weight at baseline, then every 3 months for the first year, then every 6 months after that. That’s not optional. It’s standard care.But not all clinics do it. A 2021 survey found 92% of pediatric practices now use electronic growth charts, which is good. But if the numbers aren’t reviewed at every visit, the chart is just a file folder. Growth velocity-the rate of growth over time-is what matters more than a single measurement.
If a teen’s height z-score drops by more than 0.5 or their weight z-score drops by more than 1.0 in six months, it’s a red flag. That’s when you need to act. Not wait. Not hope it gets better.
Some doctors recommend "medication holidays"-taking breaks during summer, holidays, or weekends. A 2020 study found 73% of pediatric psychiatrists support this. And research shows 87% of teens who take a break recover 75% of their expected growth rate within six months. That’s powerful. It means growth suppression isn’t always permanent.
What Parents Can Do Right Now
You don’t have to wait for the next appointment. Here’s what works:- Feed before the medication hits. Give a high-calorie, protein-rich breakfast before the first dose. Eggs, peanut butter toast, smoothies with nut butter and banana-these are better than cereal.
- Plan calorie-dense snacks. Keep cheese sticks, trail mix, whole milk yogurt, or avocado slices handy. These pack calories without needing big portions.
- Make dinner the main meal. Let your teen eat as much as they want after school. Don’t restrict. Don’t judge. This is recovery time.
- Track food intake. Use a simple notebook or app. Note what they eat, when, and how much. Patterns show up fast.
- Don’t force food. Pressure makes kids associate meals with stress. Instead, offer choices: "Would you rather have grilled cheese or tuna salad?"
In severe cases, doctors may prescribe cyproheptadine, an old antihistamine that also stimulates appetite. It’s not perfect-it can cause drowsiness-but for teens losing weight rapidly, it’s a bridge.
When to Consider Switching Medications
Not every teen needs to stay on stimulants. If growth or appetite issues are severe and persistent, switching is a valid option.Atomoxetine (Strattera) is the most common non-stimulant alternative. It doesn’t suppress appetite or growth. But it takes weeks to work, and it’s less effective for hyperactivity and impulsivity. It’s better for teens who struggle mostly with focus and organization.
Newer options like viloxazine (Qelbree) and the 2023 FDA-approved Adhansia XR show promise in reducing appetite suppression. Adhansia XR, for example, had 18% less weight loss in clinical trials than older amphetamines.
And now, pharmacogenetic testing is starting to help. Companies like Genomind use genetic tests (like CYP2D6) to predict how a teen will metabolize stimulants. In their 2022 trial, teens whose dosing was adjusted based on genetics had 40% fewer growth-related side effects. It’s not mainstream yet-but it’s coming.
The Bigger Picture: Benefits vs. Risks
It’s easy to focus on the numbers: 1 inch shorter, 10 pounds lighter. But what’s the alternative?Untreated ADHD increases the risk of academic failure, substance abuse, car accidents, depression, and unemployment. A teen who can’t focus in class is more likely to drop out. One who can’t control impulses is more likely to get into trouble. Medication reduces those risks by 50 to 60%.
Dr. Joseph Biederman from Harvard put it plainly: "The height reduction seen in some studies is clinically insignificant compared to the benefits in school, relationships, and future success." He’s right. But that doesn’t mean we ignore the side effects. It means we manage them.
This isn’t about choosing between health and medication. It’s about optimizing both. Growth isn’t just a number on a chart. It’s a sign that your teen is thriving-not just surviving.
Do ADHD medications permanently stunt growth?
Most teens who experience growth suppression while on stimulant medication catch up by their mid-20s. Studies show only about 11% have persistent height reduction of more than 1.5 cm. Growth delays are usually temporary, especially if medication is paused during breaks or adjusted in dosage.
How often should height and weight be checked for teens on ADHD meds?
The American Academy of Pediatrics recommends checking height and weight at the start of treatment, then every 3 months during the first year, and every 6 months after that. If growth slows significantly, more frequent monitoring is needed.
Can I just stop the medication if my teen stops growing?
Stopping medication abruptly isn’t recommended. It can cause a rebound in symptoms and affect school performance or emotional stability. Instead, talk to your doctor about adjusting the dose, switching medications, or trying scheduled breaks (like during summer). These are safer, more controlled approaches.
Are non-stimulant ADHD meds better for growth and appetite?
Yes. Non-stimulants like atomoxetine (Strattera), guanfacine, and viloxazine (Qelbree) don’t typically suppress appetite or slow growth. But they’re also less effective for core ADHD symptoms-about 30-40% less than stimulants. They’re a good option if appetite or growth is a major concern and symptoms are moderate, not severe.
What foods should I give my teen on ADHD medication?
Focus on calorie-dense, nutrient-rich foods eaten before the medication kicks in-like scrambled eggs with cheese, peanut butter on whole-grain toast, smoothies with banana and almond butter, or yogurt with granola and nuts. Keep snacks like cheese sticks, trail mix, and hummus with veggies available after school. Avoid sugary snacks that cause energy crashes.
Is it normal for my teen to eat a lot after school?
Yes. Many teens on stimulants eat very little during the day because their appetite is suppressed. When the medication wears off, hunger returns strongly. This is normal. Don’t restrict evening meals. Instead, make them balanced and nutrient-rich to support recovery and growth.
Can pharmacogenetic testing help reduce side effects?
Yes. Genetic testing for enzymes like CYP2D6 can show how quickly a teen metabolizes stimulants. Teens who are slow metabolizers may need lower doses to avoid side effects. A 2022 trial showed a 40% reduction in growth-related side effects when dosing was guided by genetic testing.
What’s Next?
The next few years will bring more precision to ADHD treatment. Genetic testing, new drug formulations, and better growth-tracking tools will make it easier to balance symptom control with healthy development. But right now, the best tool you have is consistent monitoring, open communication with your teen, and a willingness to adjust.ADHD medication isn’t a one-size-fits-all fix. It’s a tool. And like any tool, it works best when you pay attention to how it’s being used-and what it’s doing to your child’s body along the way.
 Digital Therapeutics and Medication Interactions: What You Need to Know in 2026
Digital Therapeutics and Medication Interactions: What You Need to Know in 2026
 Pharmacy Counseling: What to Learn When Picking Up Generics
Pharmacy Counseling: What to Learn When Picking Up Generics
 Peru Balsam: The Life-Changing Dietary Supplement You Need to Experience
Peru Balsam: The Life-Changing Dietary Supplement You Need to Experience
 Buy Cialis Professional Online: Your Guide to Secure Purchase
Buy Cialis Professional Online: Your Guide to Secure Purchase
 Serum Sickness-Like Reactions to Antibiotics: What Parents and Doctors Need to Know
Serum Sickness-Like Reactions to Antibiotics: What Parents and Doctors Need to Know
Heidi Thomas
December 5, 2025 AT 13:48Alex Piddington
December 6, 2025 AT 01:12Libby Rees
December 7, 2025 AT 01:48Dematteo Lasonya
December 7, 2025 AT 13:59Rudy Van den Boogaert
December 8, 2025 AT 19:53Gillian Watson
December 9, 2025 AT 00:41Jordan Wall
December 10, 2025 AT 15:25Gareth Storer
December 12, 2025 AT 14:03Pavan Kankala
December 13, 2025 AT 11:45Martyn Stuart
December 15, 2025 AT 01:03