When Sofosbuvir is described as a nucleotide analog inhibitor of the hepatitis C virus (HCV) NS5B polymerase, it revolutionized the cure rates for chronic HCV infection, pushing sustained virologic response (SVR) beyond 95% in most genotypes. Yet the story doesn’t end there. Researchers, pharma companies, and public‑health agencies are already racing toward the next wave of therapies that promise even shorter courses, higher barriers to resistance, and broader access worldwide. Below we break down the most exciting advances on the horizon, explain how they differ from the sofosbuvir era, and give you a realistic sense of when these options might hit the clinic.
Why the Search for “Next‑Gen” HCV Drugs Matters
Even though current regimens cure the vast majority of patients, three gaps persist:
- Hard‑to‑treat populations: people with decompensated cirrhosis, renal failure, or HIV‑HCV co‑infection often require dose adjustments or face higher side‑effect risks.
- Resistance‑associated substitutions (RAS): a small but growing subset of patients develop viral mutations that blunt the efficacy of existing direct‑acting antivirals (DAAs).
- Global elimination goals: the World Health Organization aims to cut new infections by 80% and mortality by 65% by 2030, a target that demands cheaper, easier‑to‑deliver cures.
Addressing these issues drives the pipeline we’ll explore next.
Pan‑Genotypic Regimens on the Verge of Approval
Since the launch of sofosbuvir/velpatasvir (Epclusa) in 2016, the industry has focused on simpler, pan‑genotypic combos that work across all HCV genotypes (1‑6) without the need for genotype testing. Two candidates stand out:
- Glecaprevir/pibrentasvir (G/P) extended‑release formulation: The current G/P tablets already offer an 8‑week cure for most patients. A new once‑monthly injection version is in Phase III, aiming to turn a two‑minute office visit into a single dose.
- ABT‑530 (glecaprevir) + ABT‑333 (pibrentasvir) high‑potency tablet: Early data suggest SVR rates of 99% even in patients with severe liver disease, with a potential 4‑week treatment window.
Both combos target the NS3/4A protease and NS5A protein, respectively, delivering a double‑hit that raises the genetic barrier to resistance.
Emerging Mechanisms: Beyond the Classic DAA Targets
Most current DAAs, including sofosbuvir, lock onto the NS5B polymerase or NS5A replication complex. New classes aim at different viral steps:
- Capsid assembly inhibitors (e.g., JNJ‑6379): These molecules prevent the virus from forming a stable capsid, halting the life cycle before RNA replication even begins.
- Host‑targeted agents like cyclophilin inhibitors (Alisporivir): By modulating host proteins the virus depends on, the risk of viral resistance drops dramatically.
- RNA‑directed CRISPR‑Cas13 therapies: Early preclinical work shows that a single‑dose inhaled CRISPR system can cleave HCV RNA inside hepatocytes, offering a potential cure without the need for long‑term drug exposure.
While still in early trials, these mechanisms could eventually replace or augment the DAA toolbox.

Ultra‑Short Treatment Courses: The 3‑Week Dream
Clinical trials are testing whether ultra‑short regimens can still achieve >95% SVR. A noteworthy study from 2024 combined a high‑dose NS5B polymerase inhibitor with a next‑gen NS5A blocker for just three weeks, reporting 96% cure in genotype‑1 patients. If larger Phase III studies confirm these numbers, the standard 8‑12‑week courses may become optional for many, reducing costs and improving adherence.
Price, Access, and the Path to Global Elimination
Even the most effective drug is useless if people can’t afford or reach it. The next wave aims to address this on three fronts:
- Manufacturing innovations: Continuous flow chemistry is slashing production costs for nucleotide analogs by up to 40%.
- Tiered pricing models: Several manufacturers have pledged volume‑based discounts for low‑ and middle‑income countries, aligning with WHO’s 2030 goals.
- Point‑of‑care formulations: The injectable G/P we mentioned earlier can be stored at room temperature for six months, opening the door to mobile clinics and remote outreach.
These strategies, combined with the scientific advances, make a realistic case for worldwide HCV eradication within the next decade.

Comparison of Upcoming Therapies vs. Sofosbuvir‑Based Regimens
| Attribute | Sofosbuvir + Velpatasvir (Epclusa) | Glecaprevir/Pibrentasvir Injection (Projected) | Capsid Assembly Inhibitor (JNJ‑6379) | CRISPR‑Cas13 RNA Therapy |
|---|---|---|---|---|
| Genotype Coverage | Pan‑genotypic (1‑6) | Pan‑genotypic (1‑6) | Pan‑genotypic (pre‑clinical) | Pan‑genotypic (pre‑clinical) |
| Standard Treatment Duration | 8‑12 weeks | 1 dose (monthly) | 4‑8 weeks (trial) | Single inhaled dose |
| Route of Administration | Oral tablets | Subcutaneous injection | Oral tablets | Inhalation |
| Resistance Barrier | High (NS5A + NS5B) | Very high (dual protease/NS5A) | Moderate (novel target) | Minimal (viral genome editing) |
| Key Safety Concerns | Fatigue, headache | Injection site reactions | Potential off‑target effects | Immune activation risk |
What Patients Should Ask Their Provider
When a new drug is on the horizon, it’s easy to feel both hopeful and confused. Here are five quick questions to keep the conversation focused:
- Am I a candidate for a shorter‑duration regimen, or do I need the standard 8‑12‑week course?
- Is there a risk of resistance with my current genotype, and would a next‑gen drug reduce that risk?
- Will my insurance cover the upcoming therapy, or are there patient‑assistance programs?
- If I have kidney disease, which of the new agents are safest?
- Can I enroll in a clinical trial for a novel therapy, and what are the logistics?
Being prepared with these questions helps you and your clinician weigh the benefits against any unknowns.
Mini‑FAQ
When might the injectable G/P formulation be available?
Regulatory filings are slated for early 2026, with a U.S. launch expected by Q4 2026 pending FDA approval.
Are capsid assembly inhibitors safe for patients with cirrhosis?
Phase II data show comparable safety to existing DAAs, but larger trials are still needed to confirm liver‑specific tolerability.
Could CRISPR‑Cas13 replace oral DAAs entirely?
In theory, a single CRISPR dose could cure HCV, but safety, delivery, and regulatory hurdles mean it’s at least a decade away from routine use.
What happens if a patient develops resistance to sofosbuvir?
Current guidelines recommend adding a high‑potency NS5A inhibitor (e.g., pibrentasvir) and extending therapy to 24 weeks, often achieving cure despite the RAS.
How do pricing models differ for next‑gen therapies?
Manufacturers are moving toward outcome‑based contracts: pay‑once the virus is undetectable at 12 weeks post‑treatment, reducing financial risk for payers.
In short, the future of hepatitis C treatment looks brighter than ever. From single‑dose injectables to gene‑editing cures, the pipeline is tackling the remaining gaps that sofosbuvir left behind. Keep an eye on clinical‑trial registries, talk to your liver specialist about eligibility for emerging options, and stay hopeful-eradication is within reach.
 Ischemia and Sleep Apnea: Risks, Symptoms, Tests, and Treatment (2025 Guide)
Ischemia and Sleep Apnea: Risks, Symptoms, Tests, and Treatment (2025 Guide)
 Affordable Rifaximin Alternatives for IBS-D and Traveler’s Diarrhea Relief
Affordable Rifaximin Alternatives for IBS-D and Traveler’s Diarrhea Relief
 8 Alternatives to Prelone: Discovering Better Options
8 Alternatives to Prelone: Discovering Better Options
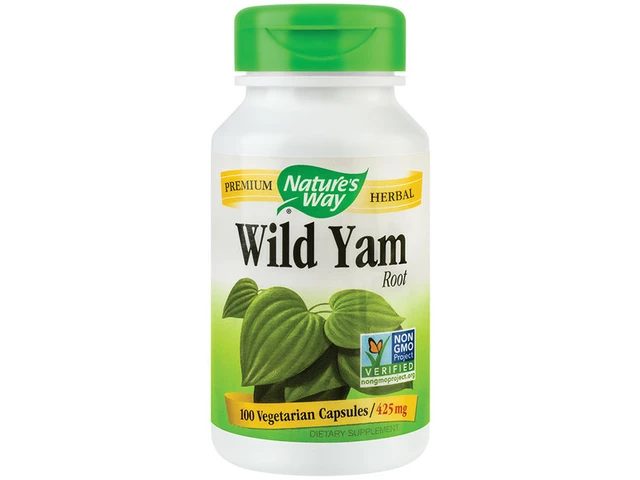 Wild Yam: The Unsung Hero of Natural Dietary Supplements
Wild Yam: The Unsung Hero of Natural Dietary Supplements
 Buspirone Tapering Guide: How to Reduce Anxiety Medication Safely
Buspirone Tapering Guide: How to Reduce Anxiety Medication Safely
Edward Brown
October 25, 2025 AT 15:46They want us to think the cure is done and forget the shadows behind each new pill the big pharma labs push into the market it’s a cycle of profit masked as progress
ALBERT HENDERSHOT JR.
October 25, 2025 AT 17:10The evolution of hepatitis C therapeutics showcases how collaborative science can transform a once‑fatal disease into a curable condition.
Recent data on pan‑genotypic regimens underscore the power of targeting multiple viral proteins simultaneously, which not only improves efficacy but also fortifies the barrier against resistance.
Moreover, the shift toward shorter, even ultra‑short treatment courses reflects a patient‑centric mindset, aiming to reduce pill burden and improve adherence.
From a public‑health perspective, these advances align perfectly with the WHO’s elimination targets for 2030.
The injectable formulation of glecaprevir/pibrentasvir, for instance, could simplify outreach in remote settings by eliminating the need for daily oral dosing.
Capsid assembly inhibitors such as JNJ‑6379 represent an innovative mechanistic class that interferes with viral particle formation, expanding our therapeutic toolbox beyond the classic NS5A/NS5B targets.
Host‑targeted agents like cyclophilin inhibitors remind us that leveraging host biology can mitigate the risk of viral escape mutations.
While CRISPR‑Cas13 RNA editing remains experimental, its potential for a single‑dose cure is an exciting glimpse into the future of precision medicine.
It is also encouraging to see manufacturers embracing tiered pricing and outcome‑based contracts, which could make these breakthroughs accessible to low‑ and middle‑income countries.
The continuous‑flow chemistry improvements that cut production costs by up to forty percent illustrate how manufacturing innovation can complement clinical innovation.
In practice, clinicians should assess individual patient factors-such as renal function, decompensated cirrhosis, or co‑infection-to select the most appropriate regimen.
Engaging patients in shared decision‑making, especially regarding treatment duration and potential side effects, enhances therapeutic success.
The emerging data suggest that a three‑week high‑dose regimen may soon be viable for select genotypes, further shrinking the treatment window.
As we look ahead, integrating these novel agents into real‑world practice will require robust surveillance for resistance patterns and safety signals.
Ultimately, the convergence of scientific ingenuity, manufacturing efficiency, and equitable pricing promises to bring us closer to global HCV eradication.
Keep the optimism grounded in data, and stay hopeful :)
Suzanne Carawan
October 25, 2025 AT 18:33Oh great, another miracle pill that will magically appear next year while we’re still waiting for the current ones to be affordable for everyone.
Kala Rani
October 25, 2025 AT 19:57Sure, because the only thing pharma cares about is world health, not their bottom line.
Donal Hinely
October 25, 2025 AT 21:20Yo the next gen HCV game‑changer is gonna slam the competition like a bhangra drum solo at a TED talk, single‑dose injectables will blast through the barriers and make the old oral pills look like grandma’s tea‑bags.
Octavia Clahar
October 25, 2025 AT 22:44Listen, while the hype is fun, let’s not forget the patients who already struggle with insurance hoops – a pricey injection might be a nightmare if you’re on a fixed income.
Lionel du Plessis
October 26, 2025 AT 00:07From a pharmacokinetic standpoint the sub‑Q depot formulation offers a prolonged half‑life reducing Cmax variability and enhancing adherence metrics.
Andrae Powel
October 26, 2025 AT 01:31In plain terms the capsid assembly inhibitor works by stopping the virus from building its protective shell so even if some viral RNA slips through it can’t package itself properly – this adds another layer of protection against resistance and complements the protease‑NS5A combos already in use.
Leanne Henderson
October 26, 2025 AT 02:54Hey everyone! 😊 I just wanted to highlight how crucial it is for patients to bring up their concerns about treatment length, potential side effects, and insurance coverage early on – the more we discuss, the better the outcomes! 🙌
Greg Galivan
October 26, 2025 AT 03:18Shorter cures are cool but don’t expect miracles overnight.