What Your Heart’s Calcium Score Really Means
Most people think heart disease shows up with chest pain or a heart attack. But for many, the warning signs are already there-hidden in the walls of their arteries-years before any symptoms appear. That’s where a simple, quick CT scan comes in. A coronary calcium score doesn’t show blockages. It shows something even more telling: calcium deposits in your coronary arteries. These deposits aren’t just random minerals. They’re the hardened remains of plaque, the sticky buildup that can eventually lead to a heart attack.
The scan takes less than five minutes. You lie on a table, EKG leads stick to your chest to sync the images with your heartbeat, and you hold your breath for 10 to 15 seconds. No needles. No contrast dye. No fasting, other than avoiding caffeine and smoking for a few hours before. It’s painless. And it’s one of the most powerful tools we have to catch heart disease before it’s too late.
How the Score Is Calculated-and What It Tells You
The result isn’t just a number. It’s a snapshot of your arterial health over time. The score uses something called the Agatston method, developed in the 1990s. It looks at how much calcium is there and how dense it is. A score of zero means no detectable calcium. That’s the best-case scenario. But if your score is above zero? That’s not normal. It means you have some form of coronary artery disease, even if you feel fine.
Here’s what the numbers mean in practical terms:
- 0: No detectable plaque. Low risk.
- 1-10: Minimal plaque. Still low risk, but it’s a sign to pay attention.
- 11-100: Mild plaque. You’re not in immediate danger, but your arteries are already changing.
- 101-400: Moderate plaque. Your risk of a heart event is 75% higher than someone with no calcium.
- 401+: Extensive plaque. High risk. This isn’t just a warning-it’s a red flag.
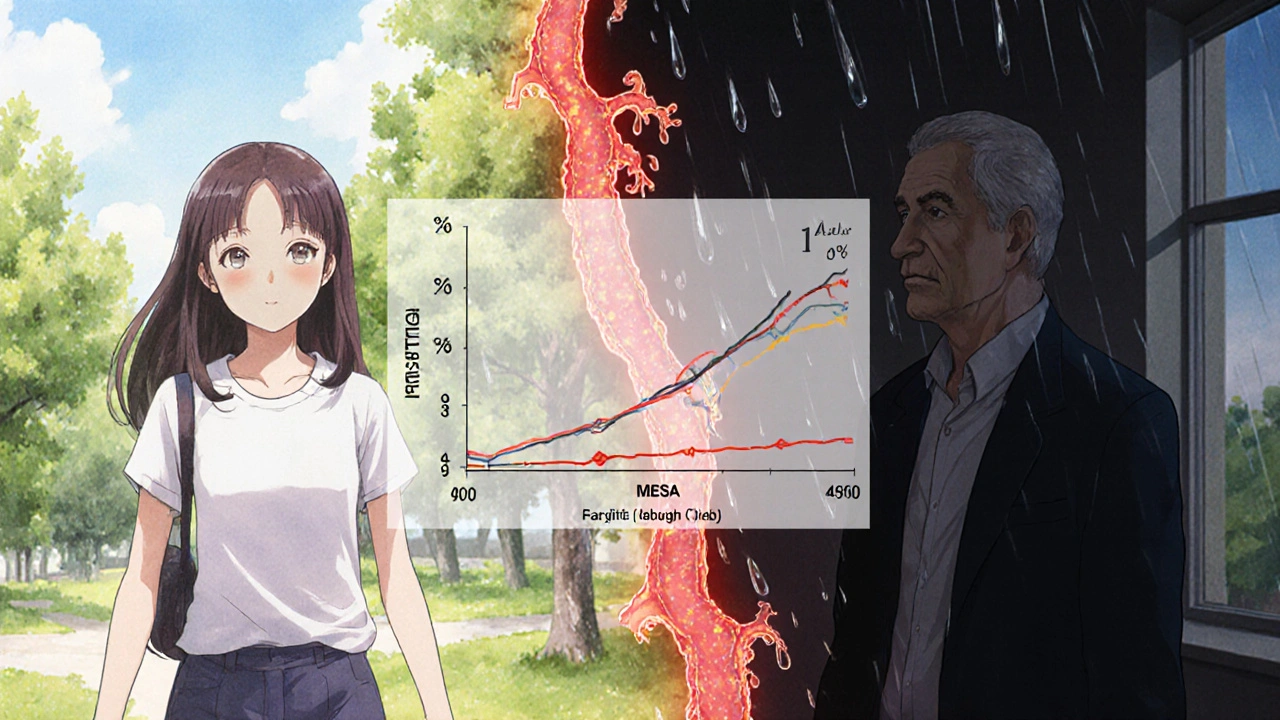
But here’s the twist: your score doesn’t just stand alone. It’s compared to others your age, sex, and ethnicity using the MESA Percentile. Two 55-year-old men can both have a score of 150-but one might be at the 90th percentile (meaning 90% of men his age have less calcium), while the other is at the 40th. That makes all the difference in how your doctor treats you.
Why This Test Beats Traditional Risk Calculators
Doctors have used tools like the Pooled Cohort Equations for years to estimate heart disease risk. They look at cholesterol, blood pressure, smoking, and diabetes. But here’s the problem: they get it wrong a lot. Studies show these calculators misclassify 20-30% of people who are actually at risk.
That’s where the coronary calcium score changes everything. In one study published in Circulation, adding a calcium score to traditional risk factors reclassified nearly half of people labeled as “intermediate risk.” Some were moved to high risk-meaning they needed statins. Others were moved to low risk-meaning they could avoid unnecessary medication.
One cardiologist at Mayo Clinic put it plainly: “The scan can see the plaque and help estimate heart attack risk more accurately.” It doesn’t guess. It shows.
What the Scan Can’t See-and What Comes Next
Here’s the catch: calcium scoring only sees calcified plaque. About 20-30% of plaque is soft and hasn’t hardened yet. That kind of plaque is just as dangerous-it can rupture and trigger a heart attack-but it won’t show up on this scan.
If your score is high or your doctor suspects more than just calcium buildup, they might recommend a coronary CT angiography (CCTA). That test uses contrast dye and gives a full picture of your arteries, including soft plaque. But it also means more radiation and a higher cost. For most people, the calcium score is the right first step.
And if your score is above 100? That’s when treatment changes. Guidelines from the American College of Cardiology say you should be on a statin, even if your cholesterol looks fine. If your score is above 300, you need a high-intensity statin. No exceptions. This isn’t about cholesterol numbers anymore. It’s about what’s actually in your arteries.
Real People, Real Scores, Real Changes
On Reddit’s heart disease community, people share their scores like war stories. One user, 52, had a score of 142-higher than 78% of men his age. He’d ignored his doctor’s advice to quit smoking and take a statin for years. After seeing his score, he quit cold turkey. He started the medication. He changed his diet. He didn’t wait for a heart attack to make a move.
Another woman, 61, had a score of 8. Her doctor said it was nothing. But she was a non-smoker, healthy weight, no diabetes. She was confused. She got a second opinion. Turns out, her family history of early heart disease made that small amount of calcium a red flag. She started walking daily and got her LDL under control.
These aren’t rare cases. A 2023 survey of patients found 68% said their calcium score was the wake-up call they needed. For many, it’s the first time they truly understood their risk wasn’t theoretical. It was measurable. And it was theirs to change.
Who Should Get Tested-and Who Doesn’t Need It
This isn’t a test for everyone. If you’re 30 and healthy, with no family history, no high blood pressure, no high cholesterol-you probably don’t need it. But if you’re between 40 and 75, and you have even one risk factor-high LDL, smoking, diabetes, high blood pressure, or a family history of early heart disease-this test is worth asking for.
Even better: if you’re labeled “intermediate risk” by your doctor’s calculator, this test is your next step. It’s the tiebreaker. It tells you whether you’re truly at risk or just flagged by a flawed algorithm.
There are exceptions. People with chronic kidney disease often have calcium deposits from their disease, not from plaque. Their score can be misleading. And if you’ve already had a heart attack, bypass surgery, or stent-you don’t need this test. You’re already in treatment mode.
Insurance, Cost, and Access
Here’s the frustrating part: Medicare doesn’t cover it. Most private insurers only cover it if you have specific risk factors-and even then, you might get stuck with a $100-$300 bill. In 2023, 41% of commercially insured patients faced partial or no coverage.
But the cost of skipping it? Much higher. A heart attack can cost over $1 million in lifetime care. This scan costs less than a new pair of sneakers. And it might save your life-or at least give you the push you need to change before it’s too late.
Some imaging centers offer it as a direct-pay service for $99. If your doctor recommends it and your insurance won’t pay, ask if they can help you find a low-cost provider. Many hospitals have financial assistance programs.
The Future of Calcium Scoring
Technology is getting better. New AI software cuts radiation exposure by 40% without losing image quality. Studies are underway to define exact thresholds for when to start statins based on score alone. The NIH is tracking 10,000 people over five years to see exactly how scores predict outcomes.
Right now, only 15% of eligible patients get tested. Why? Lack of awareness. Insurance barriers. Doctors not bringing it up.
But the data is clear: if you’re in the middle-risk zone, this test changes everything. It turns guesswork into action. It turns fear into control.
You don’t need to wait for symptoms. You don’t need to hope your cholesterol is good enough. You can know-right now-what’s happening inside your heart.
Frequently Asked Questions
Is a coronary calcium scan the same as a heart CT angiogram?
No. A coronary calcium scan only looks for calcium in the arteries. It doesn’t use contrast dye and doesn’t show blockages. A CT angiogram (CCTA) uses contrast dye to show the full structure of your arteries, including soft plaque and narrowing. The calcium scan is a screening tool. The angiogram is a more detailed diagnostic test.
Can a calcium score be too high? What if it’s over 1,000?
A score over 1,000 means you have extensive calcified plaque. That’s a very high risk for a heart attack within the next 5-10 years. It doesn’t mean you’re going to have one-but it does mean you need aggressive treatment: high-intensity statins, strict blood pressure control, and lifestyle changes. Your doctor will likely refer you to a cardiologist for further evaluation.
Do I need to do this test more than once?
Usually not. Unless you’re on aggressive treatment and your doctor wants to track progress, repeating the scan every 3-5 years is enough. Calcium builds slowly. If your score was 120 at 50 and 130 at 55, that’s normal progression. A big jump-like from 50 to 300 in two years-would be unusual and worth investigating.
If my score is zero, am I completely safe from heart disease?
No. A zero score means no calcified plaque-but it doesn’t rule out soft plaque, which can still rupture and cause a heart attack. It also doesn’t protect you from other heart problems like arrhythmias or heart failure. But for most people, a zero score means very low risk of a heart attack from artery blockage. It’s a strong sign you’re doing something right.
Can I get a calcium score without a doctor’s order?
Yes. Many imaging centers allow direct-to-consumer testing. You can walk in and pay out of pocket-typically $99 to $150. But it’s better to discuss results with your doctor afterward. A score isn’t just a number-it’s part of your health story. Your doctor can help you interpret it in context of your blood pressure, cholesterol, family history, and lifestyle.
What to Do Next
If you’re between 40 and 75 and have risk factors for heart disease, ask your doctor about a coronary calcium score. Don’t wait for symptoms. Don’t assume your cholesterol is enough. This test gives you real data-not a guess.
If your score is above zero, don’t panic. Use it. Let it be the reason you start walking every day. The reason you finally get your blood pressure checked. The reason you take that statin your doctor recommended but you kept putting off.
Your arteries don’t lie. And now, you can finally see what’s really happening inside them.

 Wholesale Economics: How Generic Drug Distribution and Pricing Really Work
Wholesale Economics: How Generic Drug Distribution and Pricing Really Work
 Discover Hericium Erinaceus: The All-Natural Miracle Supplement You Need to Try Today
Discover Hericium Erinaceus: The All-Natural Miracle Supplement You Need to Try Today
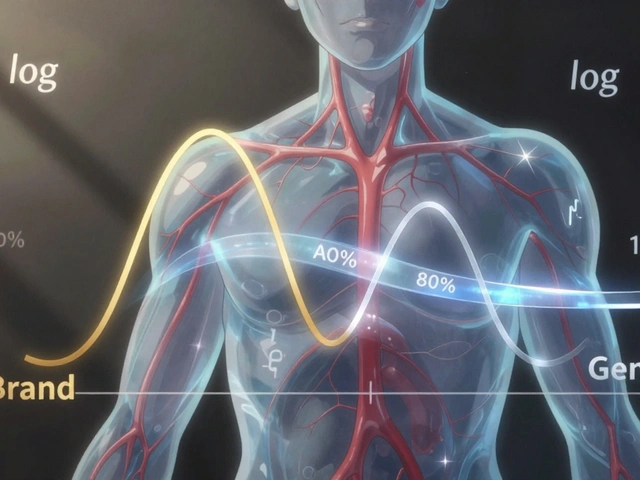 The 80-125% Rule: Understanding Bioequivalence Confidence Intervals for Generic Drugs
The 80-125% Rule: Understanding Bioequivalence Confidence Intervals for Generic Drugs
 OTC Diarrhea Treatments: When to Use and When to See a Doctor | Safe Self-Management Guide
OTC Diarrhea Treatments: When to Use and When to See a Doctor | Safe Self-Management Guide
King Over
November 19, 2025 AT 11:13Johannah Lavin
November 20, 2025 AT 15:10Shiv Karan Singh
November 22, 2025 AT 02:05Ravi boy
November 22, 2025 AT 14:19Katie Magnus
November 23, 2025 AT 22:13Matthew Karrs
November 24, 2025 AT 00:12Matthew Peters
November 24, 2025 AT 15:59Liam Strachan
November 25, 2025 AT 10:09Nosipho Mbambo
November 27, 2025 AT 08:03Kristi Bennardo
November 29, 2025 AT 06:28