Every year, millions of people take prescription drugs. Most do fine. But for some, things go wrong - unexpected rashes, heart palpitations, liver damage, even death. The FDA doesn’t wait for a pattern to emerge in clinical trials. It watches what happens in the real world. And the main tool it uses? The FDA Adverse Event Reporting System, or FAERS.
What is FAERS and Why It Matters
FAERS is the FDA’s public database for tracking side effects from drugs and biologics after they’re approved and sold to the public. Think of it as a giant, ongoing safety net. Clinical trials involve thousands of people over months or years. But once a drug hits the market, millions use it. Different ages, health conditions, medications, lifestyles - all of that can trigger side effects no one saw before. The system has been running since 1969. As of late 2023, it held over 30 million reports. About 2 million new ones are added every year. That’s not just noise - it’s the early warning system for drug safety. When enough people report the same rare reaction, the FDA can investigate. Maybe the label needs a stronger warning. Maybe the drug gets pulled. FAERS made that possible for drugs like Vioxx, Actos, and even some COVID-19 vaccines. But here’s the catch: FAERS doesn’t prove a drug caused the side effect. It just shows a report happened. A person took Drug X and had a seizure. That’s data. But was it the drug? The person’s other meds? An underlying condition? FAERS can’t answer that. It only flags patterns for further study.How Reports Get Into FAERS
There are two main ways reports get into FAERS: from drug makers and from the public. Pharmaceutical companies are legally required to report any adverse event they hear about - whether from a doctor, a patient, or a clinical trial. About 75% of reports come from them. They submit structured electronic reports using a global standard called ICH E2B(R3), which includes details like the patient’s age, gender, the drug name and dose, the adverse event (coded in MedDRA terminology), and the outcome. The other 25% come from healthcare professionals and patients through the FDA’s MedWatch program. Anyone can file a report. A nurse sees a patient with sudden kidney failure after starting a new blood pressure med? They can report it. A parent notices their child developed a rash after taking an antibiotic? They can report it too. You don’t need to be a doctor. You just need to notice something unusual. The FDA requires four basic things for a report to be accepted: one identifiable patient, one identifiable reporter, one adverse event, and one suspect drug. If any of those are missing, the report gets flagged or discarded.Public Access Tools: Dashboard vs. Raw Data
The FDA doesn’t lock FAERS behind a paywall. It gives the public two main ways to use the data: the FAERS Public Dashboard and downloadable raw data files. The FAERS Public Dashboard is designed for anyone - no coding needed. You can search by drug name, adverse event, patient age group, or time period. It shows charts, graphs, and tables. Want to know how many people reported liver injury after taking Lipitor between 2020 and 2023? Type it in. The dashboard pulls the numbers and visualizes them. It’s fast, intuitive, and perfect for initial exploration. A patient advocate, a student, or a journalist can use it in under an hour. But if you want to dig deeper - if you’re a researcher, a data scientist, or a public health analyst - you need the raw data. The FDA releases quarterly data extracts in ASCII and XML formats. These files are huge - between 1 and 5 gigabytes each. You can’t open them in Excel. You need programming tools like Python or R, plus libraries to parse XML and handle missing data. You also need to understand MedDRA, the medical terminology system used to code every adverse event. Learning MedDRA takes 40 to 60 hours for most people. It’s not just learning terms - it’s learning how they’re organized in hierarchies. For example, “headache” is a term. But “migraine” and “tension headache” are separate, more specific terms under a broader category.
What FAERS Can’t Tell You
FAERS is powerful - but it’s not perfect. Experts warn against misusing it. First, there’s no denominator. You can’t calculate how often a side effect actually occurs. Let’s say 500 people report a rare skin reaction after taking Drug A. Sounds scary. But how many people took Drug A? Ten million? One hundred million? Without that number, you can’t tell if it’s a spike or just noise. Second, reporting is biased. Serious events get reported more often. People report side effects when they’re scared, not when they’re fine. Doctors report more than patients. And drug companies report only what they’re legally required to - not everything they see. Third, data quality varies. About 30% of reports have missing or inconsistent info. A patient’s age might be listed as “unknown.” A drug name might be misspelled. One report says “aspirin,” another says “acetylsalicylic acid.” The system doesn’t always catch it. And finally, FAERS can’t prove causation. A report says someone took Drug X and had a stroke. That doesn’t mean Drug X caused the stroke. Maybe they had high blood pressure. Maybe they were smoking. Maybe it was a coincidence. FAERS only shows associations. It’s a starting point - not an endpoint.How Experts Use FAERS
Academic researchers use FAERS to find signals that might lead to new studies. In 2021, Columbia University researchers used machine learning on FAERS data to spot a possible link between a common antidepressant and a rare heart rhythm disorder - something no clinical trial had caught. That finding led to follow-up studies and a warning update. Patient advocacy groups use it too. In 2022, a group noticed a cluster of reports linking a diabetes drug to sudden weight loss. They dug into the data, found 120 similar cases over three years, and pushed the FDA to investigate. The result? A new safety alert. Pharmaceutical companies use FAERS daily - but not through the public dashboard. They use commercial platforms like Oracle Argus or ArisGlobal that pull in FAERS data along with global databases, electronic health records, and claims data. These tools can spot patterns faster, filter out noise, and integrate with internal safety systems. But they cost tens of thousands of dollars a year. That’s why FAERS remains vital for universities, small labs, and nonprofits.What’s Changing in 2025
The FDA is working to fix FAERS’ biggest weaknesses. In January 2024, it switched to ICH E2B(R3), which adds more detail to each report - like exact dosing schedules and more precise event coding. That helps reduce ambiguity. By late 2024, the FDA plans to release a new API that lets developers connect directly to the dashboard’s analysis tools - no need to download massive files. And by Q3 2025, they’re adding natural language processing to let users search with plain English, like “What drugs cause memory loss in elderly women?” instead of hunting through MedDRA codes. The bigger shift? Integrating FAERS with real-world data. The FDA’s Sentinel Initiative is linking FAERS reports with insurance claims and electronic health records. That means they’ll soon know not just that someone had a side effect - but how many people were taking the drug, what else they were on, and what their overall health looked like. That’s the next leap: turning FAERS from a report collection into a true safety intelligence system.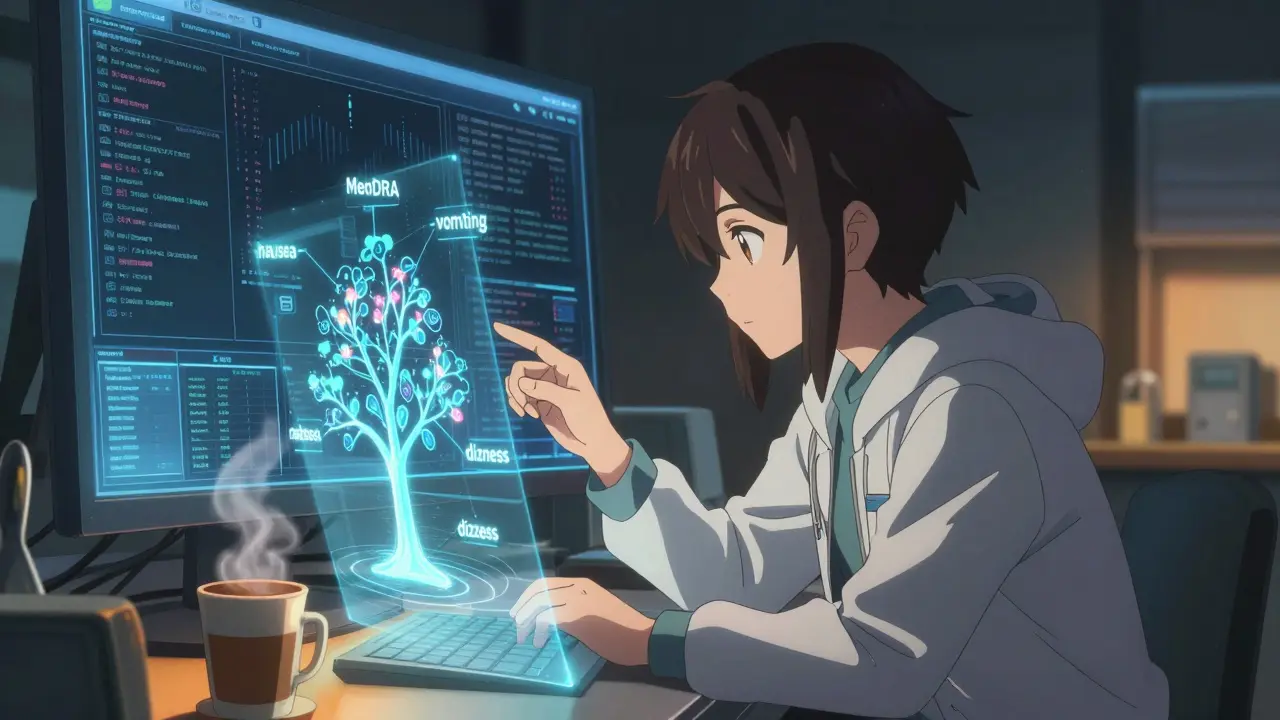
How to Get Started
If you’re a patient, caregiver, or curious member of the public:- Go to the FAERS Public Dashboard (no login needed).
- Search for a drug you’re taking or interested in.
- Look at the frequency of reported side effects. Don’t panic over a single report. Look for patterns over time.
- Use the filters: age, gender, outcome. See if certain groups report more issues.
- Start with the dashboard to get a sense of the data.
- Download the quarterly data extracts from the FDA’s website.
- Learn MedDRA basics - the FDA offers free training modules.
- Use Python or R to clean and analyze the data. Libraries like pandas and xml.etree are essential.
- Always remember: correlation ≠ causation. Look for statistical signals, not just numbers.
- Report any unusual side effect you see - even if you’re not sure. Your report could be the one that triggers a safety alert.
- Use MedWatch online or call 1-800-FDA-1088.
- Don’t wait for the FDA to act. Your input matters.
Common Mistakes and How to Avoid Them
- Mistake: Assuming a high number of reports means a drug is dangerous. Fix: Compare it to the total number of prescriptions. A drug taken by 10 million people will naturally have more reports than one taken by 100,000.
- Mistake: Ignoring MedDRA hierarchy. Fix: Don’t just search for “nausea.” Look at the broader category “gastrointestinal disorders” - you might find more relevant reports.
- Mistake: Using outdated data. Fix: Always use the latest quarterly release. Data is updated every three months.
- Mistake: Not checking for duplicate reports. Fix: The same patient might be reported multiple times by different doctors. The FDA removes duplicates, but raw data doesn’t.
Final Thoughts
FAERS isn’t a perfect system. It’s messy, incomplete, and sometimes frustrating. But it’s also one of the most transparent safety tools in the world. No other country gives the public this level of access to post-market drug safety data. It’s not about blaming drugs. It’s about understanding them better. Every report is a story - a person’s experience. And when enough stories line up, they become science. FAERS turns those stories into action. Whether you’re a patient worried about your medication, a student studying public health, or a researcher chasing a hidden risk - FAERS gives you the tools to ask better questions. And sometimes, that’s the first step to safer medicine.Can I report a side effect I experienced from a drug?
Yes. Anyone - patients, caregivers, or healthcare providers - can report adverse events to the FDA through the MedWatch program. You don’t need to be a doctor. Go to the FDA’s MedWatch website or call 1-800-FDA-1088. Even if you’re unsure whether the drug caused the issue, report it. Your report could help identify a new safety signal.
Is the FAERS Public Dashboard free to use?
Yes. The FAERS Public Dashboard is completely free and requires no registration. You can search for drugs, view trends, and download charts without paying anything. It’s designed for public use - students, journalists, patients, and advocates.
Why do some drugs have more reports than others?
Drugs that are taken by more people naturally have more reports. A widely prescribed statin like atorvastatin will have thousands of reports simply because millions take it. A rare cancer drug might have only a few dozen reports - not because it’s safer, but because fewer people use it. Always compare reports to usage volume, not just raw numbers.
Can I trust FAERS data to decide whether to take a medication?
No. FAERS data alone should not guide personal medical decisions. It shows reports - not proven risks. Always talk to your doctor or pharmacist. They can interpret the data in context of your health history, other medications, and individual risk factors.
How often is FAERS data updated?
The FDA releases new FAERS data quarterly - every three months. The Public Dashboard updates with each release, and raw data files are posted on the FDA website. Always check for the most recent quarter when analyzing trends.
What’s the difference between FAERS and MedWatch?
MedWatch is the program you use to report adverse events - it’s the reporting system. FAERS is the database that stores all those reports. Think of MedWatch as the mailbox and FAERS as the filing cabinet. Reports submitted via MedWatch go into FAERS for analysis.

 Diarex vs Alternatives: Which Hair Loss Treatment Performs Best?
Diarex vs Alternatives: Which Hair Loss Treatment Performs Best?
 Compare Adalat (Nifedipine) with Alternatives: What Works Best for High Blood Pressure
Compare Adalat (Nifedipine) with Alternatives: What Works Best for High Blood Pressure
 FDA’s Abbreviated New Drug Application Process Explained: How Generic Drugs Get Approved
FDA’s Abbreviated New Drug Application Process Explained: How Generic Drugs Get Approved
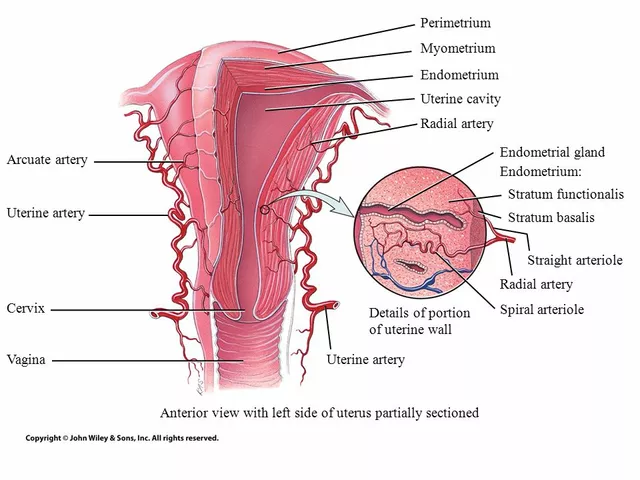 The Connection Between Overgrowth in the Uterine Lining and Migraines
The Connection Between Overgrowth in the Uterine Lining and Migraines
Becky Baker
December 26, 2025 AT 07:15This whole FAERS system is a joke. The FDA lets anyone report anything and then acts like it's gospel. My cousin took a statin and got a rash - they put it in the database like it was proof the drug kills people. Meanwhile, real science gets buried under noise. We need real data, not crowd-sourced panic.
Amy Lesleighter (Wales)
December 26, 2025 AT 09:44just wanted to say i used the dashboard last week after my mom had a weird reaction to her blood pressure med. found 3 other people with the same thing. didn't know what to do until i saw the pattern. its not perfect but it saved her. dont ignore the little reports. they add up.
Peter sullen
December 27, 2025 AT 04:45It is imperative to underscore, with the utmost gravity, that the FAERS database, while inherently imperfect and statistically confounded, remains an indispensable pillar of pharmacovigilance in the post-marketing surveillance ecosystem. The absence of a denominator, coupled with reporting bias and heterogeneity in data integrity, necessitates rigorous multivariate modeling prior to any inferential conclusion. One must never conflate association with causation - a cardinal sin in epidemiological analysis.
Steven Destiny
December 28, 2025 AT 14:03Stop being so scared of data. If you're not using FAERS, you're not doing your job. Whether you're a patient or a researcher, this is your weapon. The FDA didn't build this for bureaucrats - they built it for YOU. Use it. Fight for your safety. Don't wait for someone else to do it.
Fabio Raphael
December 29, 2025 AT 01:26I’ve been digging into FAERS data for my thesis on antidepressants and heart rhythms. It’s messy, yeah - half the reports have no age, some drug names are misspelled as ‘seratol’ or ‘prozacx’. But when you clean it, the patterns start whispering. One report might mean nothing. But 120? That’s a conversation the FDA can’t ignore anymore.
sakshi nagpal
December 31, 2025 AT 01:22As someone from India, I find it inspiring that the FDA makes this data public. In my country, such transparency is rare. Even with its flaws, FAERS empowers ordinary people. I shared the dashboard with my aunt who was worried about her diabetes meds - she felt heard for the first time.
Brittany Fuhs
January 1, 2026 AT 03:39Anyone who thinks this database is 'helpful' is either naive or paid by Big Pharma. The FDA lets pharmaceutical companies control 75% of the input. They filter, they delay, they bury. And now they want us to trust this? Please. Real safety comes from independent labs - not corporate-fed reports masquerading as science.
Sophia Daniels
January 1, 2026 AT 12:06FAERS is the internet’s version of a fever dream - but somehow, it works. Picture this: a grandma in Ohio reports her husband’s brain fog after a new cholesterol pill. Three months later, a grad student in Portland spots a spike. Now the FDA’s got a warning. That’s not magic - that’s people. Real people. Not robots. Not suits. People. And that’s why I’ll keep reporting. Even if my spelling’s trash.