When you’re taking five or more medications every day, it’s not just a numbers game-it’s a ticking time bomb for your health. This isn’t hypothetical. In the U.S., nearly half of adults over 65 are on five or more prescriptions, and that number is climbing. For many, these drugs are lifesavers: blood pressure pills, diabetes meds, heart medications. But when they pile up, the risks don’t just add up-they multiply. Polypharmacy-the regular use of five or more drugs-is now one of the biggest hidden dangers in modern medicine, especially for older adults.
Why Five Medications Is a Red Flag
There’s nothing magical about the number five. It’s not a law. But it’s the threshold doctors use because the data doesn’t lie. People taking five or more medications are twice as likely to have a serious fall. Their risk of hospitalization jumps by 24%. Their chance of an adverse drug event-like confusion, dizziness, internal bleeding, or kidney damage-goes up with every extra pill. A 2016 study in BMJ Open found that people on 10 or more drugs had a 28% higher risk of dying within a year than those on just one to four. That’s not a small increase. That’s life-or-death. The problem isn’t always that the drugs are bad. It’s that they’re too many. Take heart disease, for example. The right combination-beta blocker, statin, aspirin, ACE inhibitor-can cut death risk by 50-60%. That’s appropriate polypharmacy. But if that same patient is also on a sleep aid, an antacid, a painkiller, an antidepressant, and a supplement their cousin swore by? That’s where things unravel. Each new drug adds another layer of risk, another chance for interaction, another side effect that gets mistaken for a new illness.The Domino Effect: Medication Cascades
One of the most dangerous traps in polypharmacy is the medication cascade. It starts with a side effect. Maybe a blood pressure pill makes you dizzy. So your doctor prescribes a drug to treat the dizziness. That new drug causes dry mouth, so you’re given a saliva stimulant. Then you get constipation from that, so now you’re on a laxative. Before long, you’re on eight pills to fix problems created by the original five. A 2019 JAMA Internal Medicine study found that 30-40% of inappropriate prescriptions in older adults are part of these cascades. And often, no one ever steps back to ask: What if we just stopped the first one? This isn’t just about doctors missing something. It’s about fragmented care. You see a cardiologist, a rheumatologist, a neurologist, and your primary care doctor. Each one focuses on their piece of your health. No one’s looking at the whole puzzle. And most patients don’t know to ask for a full review. One patient, Martha, 72, told UCI Health: “I was taking 17 pills a day and couldn’t remember which ones I’d taken. I felt like a pharmacy on legs.”Who’s Most at Risk?
Older adults are the most vulnerable-not because they’re frail, but because their bodies change. As we age, our kidneys and liver don’t process drugs as efficiently. Fat and muscle ratios shift. The brain becomes more sensitive to sedatives and anticholinergics. That’s why the American Geriatrics Society’s Beers Criteria lists specific drugs that should be avoided in seniors, like benzodiazepines (for sleep or anxiety), certain antihistamines, and NSAIDs like ibuprofen. These drugs account for nearly half of all inappropriate prescriptions in older adults. But it’s not just seniors. People with multiple chronic conditions-diabetes, heart failure, arthritis, depression-are also at high risk. A 2021 study in the Journal of General Internal Medicine found that patients on 10 or more medications were 3.2 times more likely to skip doses. Why? Cost. Complexity. Side effects. Robert, 68, said his monthly meds cost $400. He had to choose between his heart medicine and food.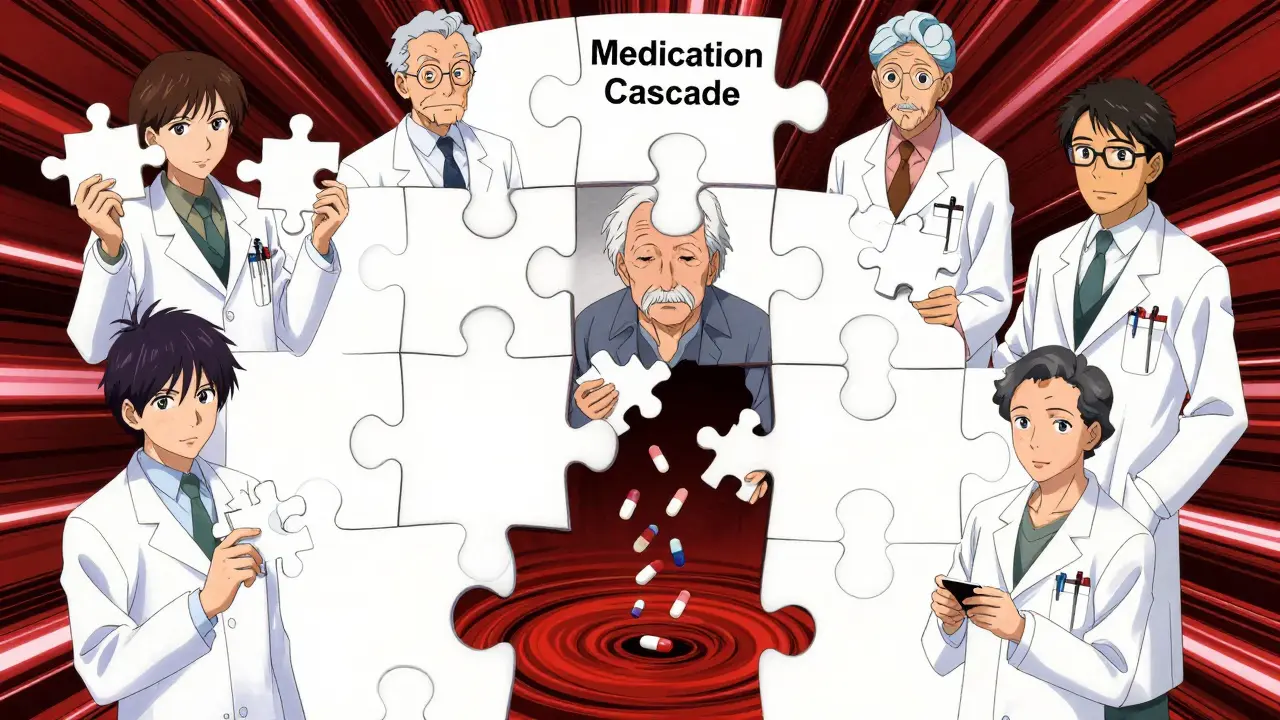
The Hidden Costs: More Than Just Money
Polypharmacy doesn’t just hurt your body-it hurts your life. Medicare’s 2022 survey showed that 48% of people on five or more drugs believed at least one side effect was caused by their meds. Nearly 30% said those side effects made them pull back from social activities. They stopped going to church, visiting friends, even walking the neighborhood. That’s not just a health issue. That’s isolation. That’s depression. That’s a loss of independence. And the financial toll? In 2022, patients taking 5-9 medications spent an average of $317 per month. Those on 10+ spent over $5,200 a year. That’s more than most people pay for rent in some areas. The U.S. spends $300 billion a year on avoidable costs tied to polypharmacy-hospital stays, ER visits, nursing home admissions-all preventable.What Can You Do? The Power of Deprescribing
The good news? You don’t have to live like this. There’s a solution called deprescribing. It’s not about stopping all your meds. It’s about stopping the ones that don’t belong. The process is simple: review, reduce, monitor.- Review: Bring every pill, capsule, patch, and supplement to your doctor-or better yet, your pharmacist. Include over-the-counter drugs, herbal teas, and vitamins. Many people don’t think of aspirin or melatonin as “medications,” but they can interact dangerously.
- Reduce: Work with your provider to identify which drugs might be unnecessary. The Beers Criteria, the STOPP/START guidelines, and tools like MedWise (an FDA-approved decision support system) help flag risky combinations. For example, if you’re on a statin, a blood thinner, and an NSAID, your risk of stomach bleeding skyrockets. One of those might be replaceable or removable.
- Monitor: Don’t just stop a drug cold. Taper slowly. Track how you feel. Did your dizziness go away? Did your appetite come back? Did your sleep improve? These are your real indicators-not what a chart says.

When Is Polypharmacy Actually Necessary?
Let’s be clear: not all multiple medications are bad. If you’ve had a heart attack, you likely need four or five drugs to prevent another. If you have advanced diabetes with kidney disease and high blood pressure, you may need six or seven. The goal isn’t to minimize drugs-it’s to minimize unnecessary drugs. The European Society of Cardiology says that when polypharmacy is tailored to a patient’s specific conditions, it can improve outcomes by 30-40%. But that only happens when the treatment plan is intentional, coordinated, and reviewed regularly. That’s the difference between appropriate and dangerous polypharmacy.What’s Being Done to Fix This?
Change is happening, slowly. In 2020, Medicare started requiring plans to review patients on eight or more medications. The 2022 SUPPORT Act expanded medication management for high-risk beneficiaries. The American Geriatrics Society’s “Choosing Wisely” campaign has already cut inappropriate prescribing by 22% in clinics that use it. New tools are emerging too. MedWise, approved by the FDA in 2022, scans your full drug list and flags dangerous interactions in seconds. The NIH is funding $15 million to develop standardized deprescribing protocols for 15 high-risk drug classes by 2026. But progress depends on you. No algorithm will ask you if you’re sleeping better. No app will notice you’ve stopped walking your dog.Your Next Steps
If you or a loved one is on five or more medications, here’s what to do now:- Make a complete list of everything you take-including doses and times.
- Bring it to your primary care provider and ask: “Which of these are still necessary? Could any be stopped safely?”
- Ask for a referral to a pharmacist who specializes in geriatric medication reviews. Many hospitals offer this for free.
- If you’re feeling dizzy, confused, tired, or nauseous, don’t assume it’s just aging. Say: “Could this be from my meds?”
- Track how you feel after any medication change. Write it down. Bring it back.
What exactly is polypharmacy?
Polypharmacy means taking five or more medications regularly. It’s not just about the number-it’s about whether those drugs are still needed, safe together, and helping you. For some people, like those recovering from a heart attack, five meds are life-saving. For others, it’s a dangerous mix of unnecessary or overlapping drugs.
Can taking too many pills really cause falls?
Yes. Medications like sedatives, blood pressure drugs, and anticholinergics can cause dizziness, low blood pressure, or confusion-especially in older adults. Studies show polypharmacy increases fall risk by 1.5 to 2 times. Falls are the leading cause of injury-related death in seniors, and many are directly tied to medication side effects.
What are the most dangerous drug combinations?
Common dangerous combos include: NSAIDs (like ibuprofen) with blood thinners (like warfarin), which raise bleeding risk; benzodiazepines (like Xanax) with opioids or sleep aids, which can cause dangerous breathing suppression; and anticholinergics (like diphenhydramine in sleep aids) with other drugs that slow the nervous system, leading to confusion or urinary retention. The Beers Criteria lists over 40 high-risk drugs for older adults.
How do I know if a medication is no longer needed?
Ask yourself: Why was this prescribed? Is the condition still active? Has it been years since the last check-up? If a drug was started for a short-term issue (like an infection or temporary pain) and never re-evaluated, it may be unnecessary. Also, if you’re taking a drug for a side effect of another drug, that’s a red flag for a medication cascade.
Can I just stop a medication on my own?
No. Stopping some drugs suddenly can be dangerous. Blood pressure meds, antidepressants, and seizure medications can cause serious withdrawal effects. Always talk to your doctor or pharmacist first. They can help you taper safely, if needed.
Is deprescribing safe?
Yes, when done properly. Studies show that carefully removing unnecessary medications improves quality of life, reduces side effects, and doesn’t increase the risk of disease worsening. In fact, patients often feel better-more energy, clearer thinking, fewer stomach issues-after deprescribing.
How often should I review my medications?
At least once a year, if you’re on five or more medications. If you’ve had a hospital stay, changed doctors, or started feeling different (tired, confused, unsteady), review them immediately. Don’t wait for your annual check-up.

 Pelvic Floor Dysfunction and Urinary Difficulty: Causes, Symptoms, and Treatment
Pelvic Floor Dysfunction and Urinary Difficulty: Causes, Symptoms, and Treatment
 Top Natural Remedies for Asthma Relief: Magnesium, Caffeine, and Herbal Solutions Backed by Science
Top Natural Remedies for Asthma Relief: Magnesium, Caffeine, and Herbal Solutions Backed by Science
 Safe Buspirone Tapering: Steps, Timelines, and Tips for Success
Safe Buspirone Tapering: Steps, Timelines, and Tips for Success
 Can Tazarotene Reduce Wrinkles? Anti‑Aging Benefits Explained
Can Tazarotene Reduce Wrinkles? Anti‑Aging Benefits Explained
 Rheumatoid Arthritis: Understanding Autoimmune Joint Damage and Modern Biologic Treatments
Rheumatoid Arthritis: Understanding Autoimmune Joint Damage and Modern Biologic Treatments
Jocelyn Lachapelle
December 16, 2025 AT 21:23People think aging means slowing down. But sometimes it just means being overmedicated.
Nupur Vimal
December 18, 2025 AT 17:41Sai Nguyen
December 20, 2025 AT 12:43Benjamin Glover
December 20, 2025 AT 20:58Raj Kumar
December 21, 2025 AT 16:39Melissa Taylor
December 22, 2025 AT 16:48John Samuel
December 23, 2025 AT 04:41Michelle M
December 24, 2025 AT 19:22Christina Bischof
December 25, 2025 AT 01:40Lisa Davies
December 25, 2025 AT 20:38John Brown
December 25, 2025 AT 23:27Mike Nordby
December 26, 2025 AT 02:19