When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But what you don’t see is the strict, often invisible system keeping the label on that bottle accurate, up-to-date, and legally identical to the original. The FDA doesn’t just approve generic drugs for safety and effectiveness-it demands their labeling match the brand-name drug down to the last word, with very few exceptions. This isn’t about copying for convenience. It’s about safety, consistency, and legal accountability across millions of prescriptions filled every day.
Identical Labeling Is the Rule, Not the Exception
The FDA requires that every generic drug’s labeling be exactly the same as its Reference Listed Drug (RLD)-the original brand-name product it’s modeled after. This rule comes straight from Section 505(j)(2)(A)(v) of the Federal Food, Drug, and Cosmetic Act and is written into 21 CFR 314.94(a)(8). That means the indications, dosage instructions, warnings, contraindications, adverse reactions, and clinical pharmacology sections must be word-for-word identical. No rewording. No simplifying. No adding extra notes. If the brand-name label says "may cause dizziness," so must the generic. If it warns about interactions with grapefruit juice, the generic has to say the same thing.
There are only three places where differences are allowed: the manufacturer’s name and address, the National Drug Code (NDC) number, and minor formatting changes required by packaging machines. Everything else? Locked in. This ensures that a doctor prescribing a generic drug isn’t working with outdated or altered safety information. It also means pharmacists, nurses, and patients all get the same critical details regardless of which version they’re using.
The Physician Labeling Rule (PLR) Changes Everything
Since 2006, all new prescription drug labels in the U.S. must follow the Physician Labeling Rule (PLR). This isn’t just a style guide-it’s a rigid structure. The PLR forces labels into 24 standardized sections, including "Highlights of Prescribing Information," "Recent Major Changes," "Boxed Warnings," and detailed subsections for use in pregnant women, elderly patients, or those with kidney disease. Generic drugs don’t get to pick and choose. When the RLD updates to PLR format, the generic must follow-within the timeline allowed by the FDA.
For example, if a brand-name heart medication adds a new boxed warning about liver toxicity in 2024, the generic version must update its label to match that exact wording. The FDA doesn’t wait for the generic manufacturer to catch up. The clock starts ticking the moment the RLD update is approved. And if the generic doesn’t comply? That’s a violation. In fiscal year 2024, labeling issues made up 37% of all complete response letters the FDA sent back to generic drug applicants-meaning nearly four in ten applications were delayed because of labeling errors.
Who’s Responsible for Keeping Labels Updated?
The burden falls entirely on the generic manufacturer. Unlike brand-name companies, which can submit a "Changes Being Effected" (CBE) supplement to update safety information before FDA approval, generic manufacturers must wait. They can’t act until the RLD’s label changes and the FDA approves that update. Then-and only then-can the generic company submit its own labeling supplement to match it.
This creates a dangerous lag. A 2024 study in JAMA Internal Medicine found that this delay affects 9,400 generic drugs, covering 89% of all prescriptions in the U.S. Safety updates often take 6 to 12 months to reach generic versions. In 2022, when valsartan-a common blood pressure drug-was recalled due to a cancer-causing impurity, generic manufacturers couldn’t update their labels to warn patients until after the brand company’s update was approved. Patients on generics were left in the dark for months.
The FDA has proposed a rule to fix this, allowing generic makers to update labels independently when new safety data emerges. But as of January 2025, that rule is still pending. Until then, the system remains broken.
Monitoring Changes Isn’t Optional-It’s a Full-Time Job
Generic drug companies can’t afford to miss a single update. They’re required to monitor the FDA’s Drugs@FDA database, which holds approved labeling documents for 2,850 reference listed drugs as of January 2025. Updates are posted weekly, usually every Tuesday. But it’s not enough to just check the site. Many companies also subscribe to FDA electronic alerts that notify them when labeling changes occur in their specific therapeutic areas.
Leading generic manufacturers dedicate 3 to 5 full-time regulatory staff for every 50 approved products just to track these updates. Smaller companies struggle. One survey found that 68% of regulatory affairs professionals in the generic industry report difficulty keeping up with labeling changes across multiple drug classes. And it’s not just about accuracy-it’s about speed. The FDA categorizes labeling changes into three types:
- Prior Approval Supplements (PAS): Require 10 months of FDA review. Used for major changes like new safety warnings.
- Changes Being Effected (CBE): Can be implemented after 30 days. Used for minor updates like dosage adjustments.
- CBE-30: Can be implemented immediately, with notification to the FDA within 30 days.
Getting the category wrong means delays, fines, or even warning letters. Between January 2023 and December 2024, the FDA issued 47 warning letters specifically for labeling discrepancies in generic drugs.
What Happens When Labels Don’t Match?
Outdated or mismatched labels aren’t just a paperwork problem-they’re a patient safety risk. Imagine a patient on a generic statin who reads the label and sees no mention of muscle pain as a side effect. But the brand-name version has a boxed warning about rhabdomyolysis. The patient ignores the symptoms, ends up in the hospital, and later finds out the label was never updated. That’s not hypothetical. It’s happened.
Regulatory agencies don’t take this lightly. The FDA’s Division of Labeling Review reviews about 1,200 ANDA applications every year. If a label doesn’t match the RLD-even by a comma-the application gets rejected. Companies that fail to update labels after an RLD change risk enforcement actions: product seizures, import bans, or even criminal penalties in extreme cases.
And it’s not just the FDA watching. Pharmacists are increasingly noticing the problem. On Reddit’s r/pharmacy, dozens of users have posted about receiving complaints from patients who noticed differences between brand and generic labels. One pharmacist wrote: "I had a patient ask me why her generic metformin didn’t mention the B12 deficiency risk that’s on the brand label. I checked Drugs@FDA. The brand updated it six months ago. The generic? Still outdated. I had to call the manufacturer’s hotline just to confirm it wasn’t a printing error. It wasn’t. It was just neglected."
The Future: AI, QR Codes, and a New System
The FDA is trying to fix the system. In January 2025, it released draft guidance under the MODERN Labeling Act to help generics update labels when the original brand product has been discontinued. There are over 1,200 such withdrawn RLDs, affecting 3,500 generic products-many of which still carry outdated labels because no one knows what to replace them with.
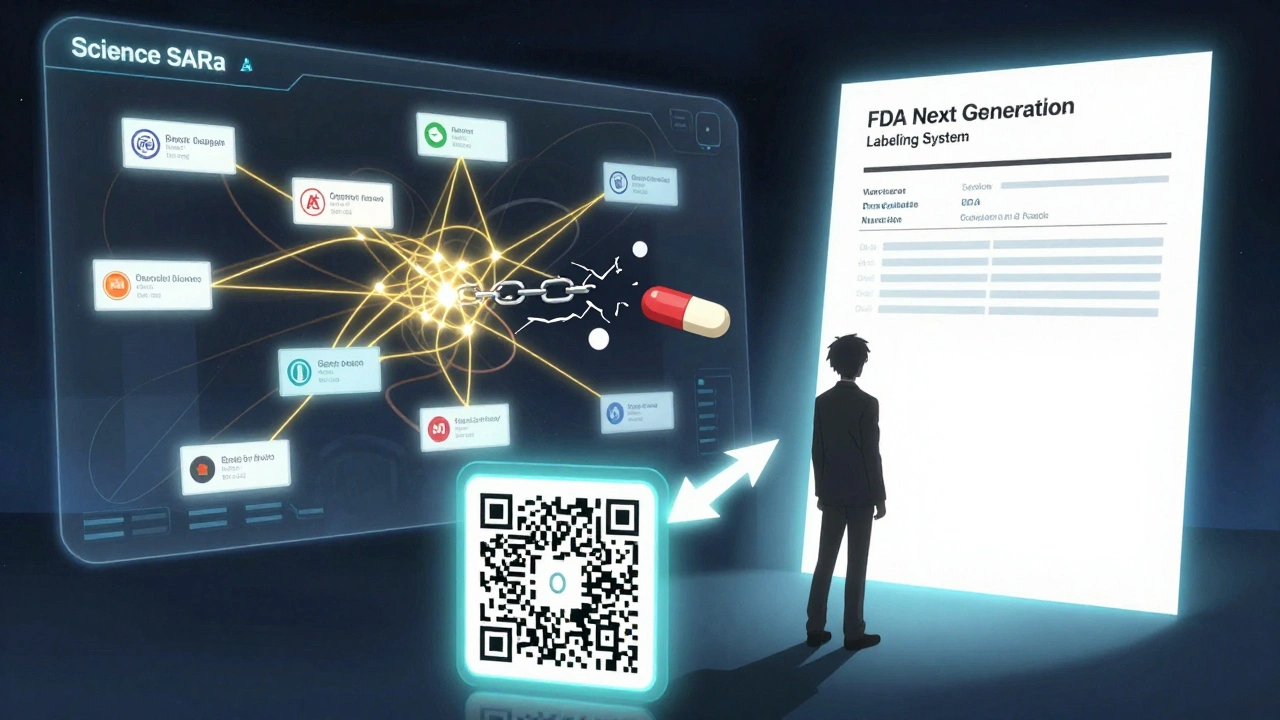
Also coming in 2025: mandatory electronic labeling. Generic drug manufacturers must now include a URL or QR code on medication guides that links directly to the current FDA-approved labeling in PDF format. The link must use HTTPS and point to the official document on Drugs@FDA. No redirects. No landing pages. Just the label.
By Q3 2025, the FDA plans to launch its Next Generation Generic Drug Labeling System, which will use AI to automatically detect changes in RLD labels and notify generic manufacturers in real time. Beta testing starts in April 2025 with 15 major companies. If it works, it could cut labeling delays from months to days.
Why This Matters to You
Over 92% of prescriptions in the U.S. are filled with generic drugs. That’s 6 billion prescriptions a year. Most of them are safe. But the labeling system holding them together is fragile. It was designed for a time when drug updates were rare. Today, safety alerts come weekly. Drug interactions are discovered in real time through electronic health records. Patients expect transparency.
Until the FDA’s proposed rule allowing generic manufacturers to update labels independently becomes law, patients are stuck with a system that prioritizes uniformity over timeliness. The cost of this delay? Lives. And money. Generic drugs save the U.S. healthcare system $647 billion a year. But if safety information is delayed, those savings vanish in ER visits, hospitalizations, and lawsuits.
The answer isn’t to stop using generics. It’s to fix the labeling rules. Until then, if you’re on a generic drug, check the label. Compare it to the brand version on Drugs@FDA. If something’s missing-especially a warning-ask your pharmacist. You might be the one who catches the gap before someone gets hurt.
Can generic drug labels be different from brand-name labels?
No, not in content. Generic drug labels must be identical to the Reference Listed Drug (RLD) in all clinical information-indications, warnings, dosage, side effects, and contraindications. Only the manufacturer’s name, address, and National Drug Code (NDC) number can differ. Any other changes require FDA approval and must still match the RLD exactly.
Why can’t generic manufacturers update their labels when new safety data comes out?
Under current FDA rules, generic manufacturers cannot independently update labeling. They must wait for the brand-name drug’s manufacturer to update its label and for the FDA to approve that change. Only then can the generic company submit a labeling supplement to match it. This creates delays of 6-12 months, which has been criticized as a patient safety risk. A proposed FDA rule would allow generics to update labels independently, but it’s still pending as of early 2025.
How do I check if my generic drug’s label is up to date?
Go to the FDA’s Drugs@FDA database at https://www.accessdata.fda.gov/scripts/cder/daf/. Search for your drug’s brand name, then click on the "Labeling" link. Compare that to the printed label on your generic bottle. If the brand label has a new warning or dosage change that’s missing from your generic, contact your pharmacist or the manufacturer. You can also check for electronic links or QR codes on the packaging-these should lead directly to the current FDA-approved label.
What happens if a generic drug’s label is outdated?
If the FDA finds that a generic drug’s label doesn’t match the Reference Listed Drug, it can issue a complete response letter, reject the application, or issue a warning letter. Companies may face product recalls, import bans, or legal action. Between 2023 and 2024, the FDA issued 47 warning letters specifically for labeling violations in generic drugs. Outdated labels also put patients at risk if critical safety information is missing.
Are QR codes required on generic drug packaging now?
Yes. As of 2025, the FDA requires generic drug manufacturers to include a URL or QR code on medication guides that links directly to the current FDA-approved labeling in PDF format. The link must use HTTPS and point to the official document on Drugs@FDA. This ensures patients and providers can always access the most up-to-date safety information, even if the printed label is outdated.
How often does the FDA update generic drug labeling requirements?
The FDA doesn’t change the core labeling rules often, but it updates guidance documents and enforcement priorities regularly. Major changes come through new legislation, like the 2020 MODERN Labeling Act, or through draft guidance, like the January 2025 update on withdrawn reference listed drugs. Labeling changes for individual drugs are updated weekly on Drugs@FDA, and manufacturers are expected to monitor those updates continuously.

 Velpatasvir and Hepatitis C: What’s New in Treatment and Research
Velpatasvir and Hepatitis C: What’s New in Treatment and Research
 Arrhythmia Procedures: Catheter Ablation and Device Therapy Explained
Arrhythmia Procedures: Catheter Ablation and Device Therapy Explained
 How Effective Is Calcipotriene for Treating Nail Psoriasis?
How Effective Is Calcipotriene for Treating Nail Psoriasis?
 How Medicines Work and When They’re Safe to Use
How Medicines Work and When They’re Safe to Use
 Generic Drug Patents: How Exclusivity Periods Vary Across Countries
Generic Drug Patents: How Exclusivity Periods Vary Across Countries
Ashley Skipp
December 12, 2025 AT 20:13Generic labels gotta be exact same as brand or its a lawsuit waiting to happen
sandeep sanigarapu
December 14, 2025 AT 15:25India follows same rule. Generic must match brand label exactly. Patient safety first. No exceptions.
Adam Everitt
December 14, 2025 AT 17:48its wild how a comma can trigger a warning letter. the system is broken but no ones got the guts to fix it
Donna Anderson
December 15, 2025 AT 23:45my mom got a generic blood pressure med and the label didnt mention the dizziness risk. she almost fell down the stairs. i called the pharmacy and they had no idea the label was outdated. this isnt just paperwork its life or death
Rob Purvis
December 16, 2025 AT 03:10It’s critical to understand that the FDA’s requirement for identical labeling isn’t about bureaucracy-it’s about preventing harm. When a patient receives a generic drug, they’re relying on the label to inform them of potential interactions, contraindications, and side effects. If even one word is missing, misaligned, or delayed, the entire safety net fails. This isn’t a minor administrative oversight; it’s a systemic vulnerability that puts millions at risk every year. And the fact that generic manufacturers can’t act until the brand-name company updates first? That’s a delay that can literally kill someone.
It’s also worth noting that pharmacists are on the front lines of this problem. They’re the ones getting calls from confused patients who notice discrepancies between the brand and generic labels. Many pharmacists spend hours cross-referencing Drugs@FDA just to confirm whether a label is current. That’s not what they went to school for. That’s not part of their job description. But they do it anyway because they care.
The proposed FDA rule allowing generics to update labels independently is long overdue. It’s not just about efficiency-it’s about equity. Patients who can’t afford the brand-name drug shouldn’t be forced to accept outdated safety information. And the QR code requirement? That’s a small but brilliant step. It means even if the printed label is wrong, the patient can still access the correct information instantly. Technology is finally catching up to the reality of modern pharmacology.
But we still have a long way to go. Smaller generic manufacturers don’t have the resources to hire 3-5 full-time regulatory staff per 50 products. They’re drowning in paperwork, missing updates, and risking enforcement actions. The FDA needs to provide better tools, automated alerts, and maybe even subsidized compliance support. This isn’t just a regulatory issue-it’s a public health crisis disguised as a paperwork problem.
And yes, patients should check their labels. But shouldn’t we expect the system to protect them without requiring them to become amateur regulators? We’ve automated everything else-why not this?
Lawrence Armstrong
December 16, 2025 AT 05:19QR codes are a game changer. I scanned mine last week and found a new warning about kidney issues that wasn't on the bottle. Called my doc right away. 🛑💊
wendy b
December 17, 2025 AT 11:27It is a matter of profound concern that the regulatory framework governing generic drug labeling remains archaic in the face of modern pharmacovigilance standards. The notion that a manufacturer must await approval from the originator entity before updating safety information is not only inefficient but ethically indefensible. One must question the priorities of an agency that permits such delays in the dissemination of critical clinical data.
Nathan Fatal
December 17, 2025 AT 17:26Went through this exact thing last year with a generic anticoagulant. The brand added a black box warning about bleeding risk in elderly patients. Our company had to wait 11 months before we could update our label. During that time, three patients on our version had major bleeds. One died. The FDA didn’t penalize us because we followed the rules. But the rules are the problem. We’re not the villains here. The system is.
And yeah, the QR code thing? Brilliant. But it’s not enough. What if the patient doesn’t have a phone? What if they’re blind? What if they’re in a rural area with no internet? Printed labels still matter. We need real-time sync, not just a link. The FDA’s AI system might help, but it needs to be mandatory, not optional. And it needs to include alerts for pharmacists, not just manufacturers.
Also-why do we still use paper labels at all? Why not digital prescribing with dynamic labels tied to the patient’s EHR? We’re in 2025. This shouldn’t be this hard.
Levi Cooper
December 19, 2025 AT 05:36So you’re telling me some guy in a lab in Ohio is getting paid to make sure a generic pill says "may cause dizziness" instead of "might cause dizziness"? That’s the most ridiculous thing I’ve ever heard. We’re spending billions to police commas while people can’t afford insulin. Fix the system or shut it down.