When your heart skips, races, or pounds out of rhythm, it’s not just annoying-it can be dangerous. Arrhythmias like atrial fibrillation (AFib) affect over 37 million people worldwide, and for many, pills alone aren’t enough. That’s where catheter ablation and device therapy come in. These aren’t last-resort options anymore. For thousands of patients, they’re life-changing treatments that restore normal rhythm, cut hospital visits, and even lower the risk of death.
What Catheter Ablation Actually Does
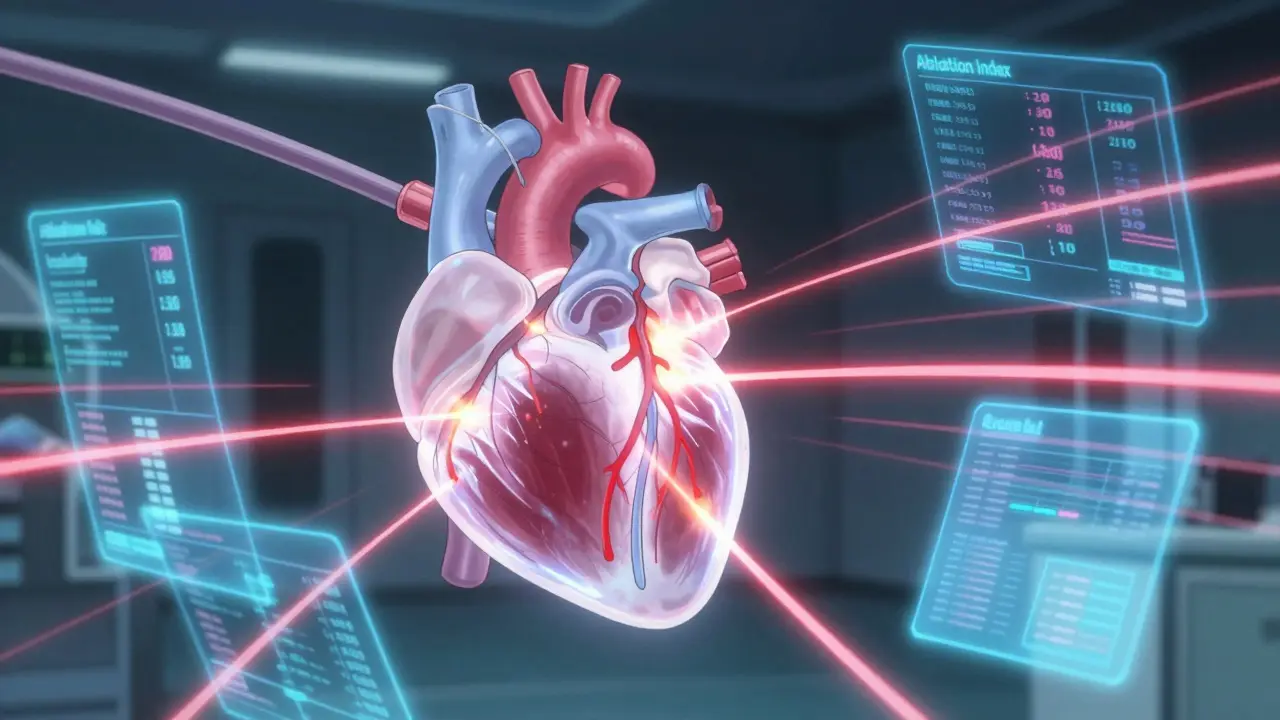
Catheter ablation isn’t open-heart surgery. It’s a minimally invasive procedure where thin, flexible wires (catheters) are threaded through a vein in your groin or neck and guided to your heart. Once in place, the tip delivers energy-either heat (radiofrequency) or cold (cryoablation)-to destroy tiny areas of heart tissue that are causing the erratic signals. Think of it like trimming a faulty wire in a circuit board. The goal isn’t to fix the whole heart, just the spots causing the short-circuit. For atrial fibrillation, doctors target the pulmonary veins, where abnormal electrical triggers often start. By creating a ring of scar tissue around them (called pulmonary vein isolation), they block those signals from spreading. This isn’t new tech. The first successful ablation was done in 1989. But today’s tools are smarter. Modern catheters like the THERMOCOOL SMARTTOUCH a radiofrequency ablation catheter with contact force sensing and Ablation Index technology, manufactured by Biosense Webster measure how hard the tip is pressed against heart tissue. Too little pressure? The burn won’t stick. Too much? You risk damaging the heart wall. The Ablation Index combines pressure, time, and power into one number, telling the doctor in real-time if the lesion is strong enough.How Cryoablation Compares
Not all ablations use heat. The Arctic Front Advance a cryoballoon ablation system by Medtronic that uses nitrous oxide to freeze tissue is a balloon-shaped device that inflates inside the pulmonary vein and freezes it from the inside out. It’s faster-procedures take 90 to 120 minutes versus 150 to 180 for radiofrequency. And because it freezes a larger area at once, it can treat multiple veins in one go. But it has trade-offs. Freezing can accidentally affect the phrenic nerve, which controls your diaphragm. That’s why doctors monitor it by pacing the nerve during the procedure. If it starts twitching, they stop and adjust. The risk is low-1.5% to 3%-but it’s real. There’s also the HeartLight a laser balloon system with built-in camera for direct visualization of tissue, which uses light instead of heat or cold. It lets doctors see exactly where they’re treating, but it takes longer and isn’t as widely used.Device Therapy: Pacemakers and ICDs
Not every arrhythmia needs ablation. Some patients need a different kind of help: a device implanted in the chest. Pacemakers small devices that send electrical pulses to maintain a steady heart rate are used for slow rhythms like bradycardia. They’re not for AFib, but they can help when AFib causes the heart to beat too slowly. For fast, dangerous rhythms like ventricular tachycardia or fibrillation, an Implantable Cardioverter Defibrillator (ICD) a device that detects life-threatening arrhythmias and delivers a shock to restore normal rhythm is the standard. It’s like having a personal emergency response team inside your chest. If your heart goes into cardiac arrest, the ICD zaps it back to life. These devices aren’t perfect. They can deliver shocks when they shouldn’t. They can get infected. They need regular checkups. But for high-risk patients-those with heart failure or prior cardiac arrest-they cut sudden death risk by up to 50%.Why Ablation Beats Pills for Many
For years, doctors treated AFib with antiarrhythmic drugs. But those pills often don’t work well. They can cause side effects like lung damage, thyroid problems, or liver toxicity. And even when they do work, they rarely cure the problem. A 2020 analysis of 1,797 patients showed catheter ablation cut AFib recurrence by 58% compared to medication. Hospital stays for heart problems dropped by 44%. For patients with heart failure and reduced pumping power (HFrEF), the benefit was even bigger: a 48% lower risk of death. One study found patients who had ablation improved their heart’s pumping ability by over 5%-something drugs rarely do. Their walking distance increased. Their anxiety dropped. One patient on Reddit said, “After my second ablation, I went from daily palpitations to zero episodes in 9 months. The mental relief is as valuable as the physical.” The CABANA trial a large randomized study that found no overall mortality benefit from ablation in all AFib patients, highlighting the need for careful patient selection sometimes gets cited to say ablation isn’t better than drugs. But that trial included low-risk patients who didn’t need it. The real winners are those with symptoms, failed meds, or heart failure.
Cost, Recovery, and Real-World Outcomes
Ablation isn’t cheap. In the U.S., it costs between $16,300 and $21,300. But over time, it pays for itself. Patients stop taking expensive drugs. They miss fewer workdays. They don’t go to the ER as often. Studies show ablation becomes cost-effective after just 3 to 8 years. Recovery is usually quick. Most people go home the same day or the next. You’ll feel sore in the groin for a few days. You’ll need to avoid heavy lifting for a week. But within a month, most return to normal activity. Complications happen in about 8% of cases. The most serious is cardiac tamponade-bleeding around the heart. It occurs in 1.2% of procedures and usually needs drainage. Stroke risk is low, under 0.5%, especially with modern anticoagulation protocols. Patient satisfaction is high. On Healthgrades, 78% of people who had ablation recommend it. The average rating is 4.3 out of 5. The biggest complaints? Recovery took longer than expected, or they had temporary discomfort during the procedure.What’s Next? Pulsed Field Ablation and AI
The next big thing is Pulsed Field Ablation (PFA) a non-thermal ablation technology using electrical pulses to target heart cells while sparing surrounding tissue. The Farapulse PFA system an FDA-approved pulsed field ablation device that showed 85.9% freedom from AF at 12 months with no esophageal injuries got FDA approval in September 2023. It uses electrical pulses instead of heat or cold, so it doesn’t burn or freeze. That means less risk to nearby structures like the esophagus or nerves. Procedures are faster-under 80 minutes. Early results show 86% success at one year. It’s not everywhere yet, but it’s the fastest-growing new tech in electrophysiology labs. In the future, AI-assisted mapping software like Medtronic’s AI Path, expected to launch in 2025, that uses machine learning to predict lesion quality and optimize ablation patterns will help doctors see exactly where to ablate. Think of it like GPS for the heart. It will make procedures even more precise and reduce the need for repeat treatments.Who Should Consider These Procedures?
You’re a good candidate for catheter ablation if:- You have symptoms like palpitations, fatigue, or shortness of breath from AFib
- You’ve tried at least one antiarrhythmic drug and it didn’t work or caused side effects
- You have heart failure and AFib (this group sees the biggest mortality benefit)
- You want to avoid lifelong medication
- You’ve had a cardiac arrest or dangerous ventricular arrhythmia
- You have severe heart failure and a low ejection fraction
- Your doctor says you’re at high risk for sudden death

What If It Doesn’t Work?
Ablation isn’t always a one-time fix. About 20% to 30% of patients need a second procedure, especially if they have persistent AFib. That’s why it’s called “arrhythmia management,” not “arrhythmia cure.” But even if rhythm isn’t perfect, many patients feel better-fewer episodes, less medication, more energy. If ablation fails, doctors can try again with newer tools, switch to a different ablation type, or combine it with device therapy. Some patients end up with a pacemaker plus ablation. Others get an ICD for added protection.Access and Equity
Here’s the hard truth: not everyone can get this care. In the U.S., rural areas have 60% fewer ablation centers than cities. If you live outside a major metro, you might need to travel hundreds of miles. Insurance coverage varies. Medicare pays about $18,500 per procedure, but private insurers sometimes deny it unless you’ve tried meds first. Still, adoption is rising. In Europe, 78% of centers now offer ablation as first-line treatment for paroxysmal AFib-up from 35% in 2015. The Heart Rhythm Society predicts ablation will become the standard first treatment for all symptomatic AFib patients by 2030.Final Thoughts
Catheter ablation and device therapy aren’t just medical procedures-they’re tools that return control to patients. They don’t just fix heart rhythms. They fix lives. You can ride a bike again. Sleep through the night. Stop worrying every time your chest flutters. That’s the real value. The data is clear. For the right person, these treatments work better than pills. They save lives. They reduce suffering. And with new technologies like pulsed field ablation on the horizon, they’re only getting better.Is catheter ablation safe for older adults?
Yes. Age alone isn’t a barrier. Studies show patients over 75 benefit just as much as younger ones, especially if they have heart failure. The main concerns are kidney function and bleeding risk, not age. Doctors assess each person individually. Many patients in their 80s have successful ablations with low complication rates.
Can I stop taking blood thinners after ablation?
Not right away. Even if your rhythm is normal, you still have the same stroke risk as before-until your heart fully recovers. Most doctors keep patients on blood thinners for at least 2 to 3 months after ablation. After that, if you’ve stayed in normal rhythm and have low stroke risk, they may consider stopping. Never stop on your own.
How long does it take to recover from an ablation?
Most people feel back to normal in 1 to 2 weeks. You’ll have soreness in the groin for a few days. Avoid heavy lifting or strenuous exercise for a week. Some patients feel tired or have occasional skipped beats for a few weeks-that’s normal as the heart heals. Full recovery takes about a month. If you still have symptoms after 3 months, talk to your doctor about a possible repeat procedure.
Do I need to stay in the hospital overnight?
Usually not. Most ablations are outpatient procedures. You’ll be monitored for 4 to 6 hours after the procedure, then go home the same day if you’re stable. Some patients stay overnight if they have other health issues or if the procedure was complex. Your doctor will decide based on your condition.
What’s the difference between a pacemaker and an ICD?
A pacemaker treats slow heart rates by sending small electrical pulses to keep your heart beating regularly. An ICD treats fast, life-threatening rhythms by delivering a strong shock to reset your heart. Some devices do both-called CRT-D devices. If you have heart failure and arrhythmia risk, your doctor may recommend one that combines pacing and defibrillation.
Can I exercise after an ablation or device implant?
Yes, and you should. Most patients are encouraged to resume light walking within a few days. After 2 to 4 weeks, you can return to moderate exercise. Avoid contact sports or heavy lifting for 6 weeks if you have an ICD. Many patients return to competitive sports after clearance from their electrophysiologist. Exercise improves heart health and reduces arrhythmia triggers.
Are there alternatives to ablation and devices?
The main alternative is medication-antiarrhythmic drugs and rate-control pills. But these often have side effects and don’t cure the problem. For some, a surgical maze procedure is an option, but it’s more invasive than ablation. Lifestyle changes like weight loss, alcohol reduction, and sleep apnea treatment can help, especially in early-stage AFib. But for moderate to severe cases, ablation and devices are the most effective options.
 Transform Your Health with Gamma Butyrolactone (Gbl): The Game-Changing Dietary Supplement You Need to Know About
Transform Your Health with Gamma Butyrolactone (Gbl): The Game-Changing Dietary Supplement You Need to Know About
 What to Do If a Child Swallows the Wrong Medication: Immediate Steps That Save Lives
What to Do If a Child Swallows the Wrong Medication: Immediate Steps That Save Lives
 How Medicines Work and When They’re Safe to Use
How Medicines Work and When They’re Safe to Use
 How to Involve Grandparents and Caregivers in Pediatric Medication Safety
How to Involve Grandparents and Caregivers in Pediatric Medication Safety
 Inactive Ingredient Interactions in Generic Medications: What You Need to Know
Inactive Ingredient Interactions in Generic Medications: What You Need to Know
Sue Stone
January 21, 2026 AT 23:48Been through two ablations for AFib. First one didn’t stick, second one? Life changed. No more meds, no more panic attacks when my chest flutters. Just normal sleep, normal walks, normal life. Wish I’d done it sooner.
Oladeji Omobolaji
January 23, 2026 AT 04:00Over here in Nigeria, we don’t even have access to this stuff. My uncle had AFib and died because they couldn’t do the procedure. It’s not just about tech-it’s about who gets to use it.
Vanessa Barber
January 23, 2026 AT 19:28So ablation is better than pills? Really? That’s what the industry wants you to believe. I’ve seen people get zapped and still end up in the ER. Don’t believe the hype.
Stacy Thomes
January 24, 2026 AT 04:43IF YOU’RE STRUGGLING WITH AFIB-DON’T WAIT. I was exhausted all the time. After ablation? I ran a 5K. I cried. This isn’t just medicine-it’s freedom.
dana torgersen
January 24, 2026 AT 22:52you know… i think… the real issue isn't the tech… it's that we've forgotten… that the heart… isn't just a pump… it's… connected… to everything… your stress… your sleep… your soul… and ablation… it's like… patching a leak… but not fixing the dam…
Dawson Taylor
January 25, 2026 AT 04:53Success rates vary by phenotype. Paroxysmal AFib responds better than persistent. Patient selection remains critical.
Andrew Smirnykh
January 27, 2026 AT 03:58I’ve read a lot on this. What’s interesting is how much the tech has evolved-not just the tools, but how we understand the heart’s wiring. It’s not just about burning tissue anymore. It’s about precision, mapping, timing. We’re moving from brute force to smart intervention.
charley lopez
January 27, 2026 AT 21:46RF ablation with contact force sensing demonstrates improved lesion continuity compared to conventional methods, per 2022 HRS consensus guidelines. Ablation Index correlates with durable pulmonary vein isolation.
Janet King
January 28, 2026 AT 12:02Patients with heart failure and reduced ejection fraction benefit the most from ablation. This is well-documented in multiple studies. Do not delay treatment if you qualify.
Kerry Moore
January 29, 2026 AT 08:53Thank you for sharing this. I’ve been researching this for my father. He’s 78, has AFib and mild heart failure. The data on mortality reduction in his group is encouraging. I’ll bring this to his cardiologist.
Laura Rice
January 29, 2026 AT 21:57My mom had the cryo balloon last year. She was scared but the docs were so calm. She got to go home the same day. Now she dances in the kitchen. I just want everyone to know: this stuff works. Don’t be afraid.
Sallie Jane Barnes
January 30, 2026 AT 19:31For anyone considering this: talk to your electrophysiologist. Ask about your specific rhythm type, your heart function, your risk factors. This isn’t one-size-fits-all. But if you’re symptomatic and meds failed-you owe it to yourself to explore it.
Anna Pryde-Smith
February 1, 2026 AT 19:09Ugh. I hate how medical companies push these procedures like they’re magic. My cousin got an ICD and got shocked for no reason three times. Now he’s terrified to leave the house. This isn’t a cure-it’s a gamble with wires and zaps.