If your child swallows the wrong medication, time is the most critical factor. Not minutes. Not seconds. Time-the time between ingestion and getting expert help-can mean the difference between a routine visit to the ER and a life-threatening emergency. Every year, over 60,000 children under five end up in emergency rooms because of accidental medication ingestion. Many of these cases are preventable. But when it happens, knowing exactly what to do-right now-can save a life.
Step 1: Call Poison Control Immediately
Do not wait. Do not Google symptoms. Do not call your pediatrician first. Pick up your phone and dial 800-222-1222. That’s the Poison Help line in the United States, staffed 24/7 by toxicology experts who have handled over 1.9 million cases in 2022 alone. They know what’s in that pill, what it does to a child’s body, and what to do next. You don’t need to know the exact dose or name of the medication-they’ll guide you through identifying it.While you’re on the phone, look around. Find the medication container. If it’s spilled, check the floor, the couch, the toy box. Write down the name, strength, and how many pills or milliliters are missing. If it’s a patch, check the child’s skin, especially the inside of the mouth or behind the ear-patches can stick there after being sucked on. This information matters. The Poison Control specialist will ask for it.
Step 2: Remove Any Remaining Substance-But Don’t Induce Vomiting
If there’s any pill, liquid, or patch still in your child’s mouth, gently remove it with your fingers. Don’t force it. Don’t stick your fingers down their throat. Just wipe or pull it out. Then rinse their mouth with water. Don’t make them spit it out-swallowing a little water helps wash away residue.Here’s what you must not do: do not make your child vomit. Not with syrup of ipecac. Not with your finger. Not with salt water. Not with anything. The American Academy of Pediatrics stopped recommending vomiting as a treatment in 2004. Why? Because it rarely helps, and it often makes things worse. Studies show vomiting causes aspiration pneumonia in 7% of attempts. It can burn the throat if the substance is caustic. It can send a pill deeper into the airway. And it delays real treatment. Poison Control experts will tell you if vomiting is ever appropriate-and in nearly every case, it’s not.
Step 3: Watch for These Warning Signs
Not all medication ingestions look the same. Some kids seem fine at first. That’s dangerous. Many life-threatening reactions start quietly. Watch closely for these signs:- Difficulty breathing, fast or shallow breathing
- Unconsciousness or extreme drowsiness
- Seizures or twitching
- Pupils that are unusually large or tiny
- Excessive drooling or foaming at the mouth
- Pale, cold, or bluish skin
- Heartbeat that’s too slow (under 50 bpm) or too fast
- Persistent vomiting or nausea
- Unexplained lethargy lasting more than 20 minutes
If you see any of these, call 911 immediately. Don’t wait for Poison Control to tell you to go. If your child is not breathing, start CPR. If they’re having a seizure, clear the area, lay them on their side, and protect their head. Do not put anything in their mouth.

Step 4: What Happens at the Hospital
Even if your child seems okay, most hospitals will keep them under observation for at least 12 hours if the medication is unknown or potentially dangerous. Why? Because some drugs-like heart medications, antidepressants, or diabetes pills-can cause delayed reactions. A child might look fine at 2 p.m. and go into cardiac arrest by 8 p.m.Doctors will monitor vital signs every 15 minutes at first. Blood tests will check for drug levels, liver damage, and blood sugar. For certain drugs, specific antidotes are used:
- Naloxone for opioid overdoses (like oxycodone or fentanyl patches)
- Octreotide for sulfonylurea pills (used for diabetes)
- Sodium bicarbonate for tricyclic antidepressants
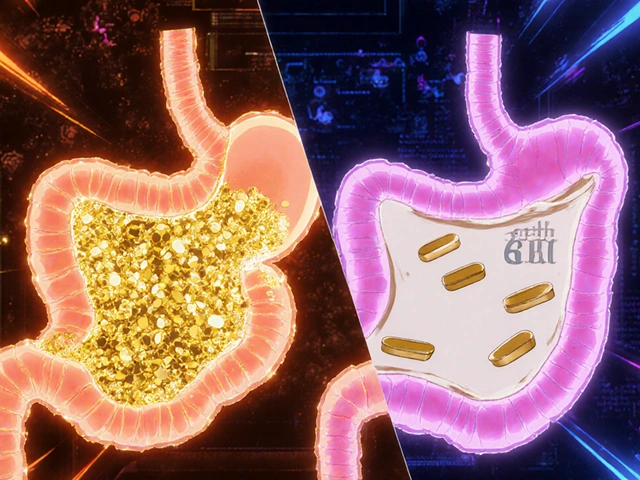
Activated charcoal may be given if the ingestion happened within the last hour. It binds to drugs in the stomach and stops them from being absorbed. But it won’t work for alcohol, acids, metals, or hydrocarbons like gasoline. And it’s not used if the child is unconscious or having seizures.
For diabetes medications, blood sugar is checked every 30 minutes. A child can slip into a coma from low blood sugar without showing obvious signs. That’s why monitoring is non-negotiable.
Step 5: Why Poison Control Works-And Why Most Parents Don’t Use It
Poison Control doesn’t just give advice. They prevent hospitalizations. According to their 2022 data, families who call Poison Control instead of going straight to the ER are 43% less likely to be admitted. That’s because specialists can often manage cases at home with clear instructions: watch for this symptom, give this fluid, check blood sugar every hour.Yet, only 61% of parents can recall the Poison Help number. That’s why the American Association of Poison Control Centers launched the “Know the Number” campaign in January 2023. Save 800-222-1222 in your phone. Program it into your home landline. Put it on the fridge. Tell your babysitter, your grandma, your neighbor. This isn’t just advice-it’s a survival skill.

How to Prevent This From Ever Happening
The best emergency plan is the one you never need. Here’s what works:- Lock it up. Medications stored in locked cabinets reduce accidental ingestions by 85%. Use childproof locks on drawers, not just cabinet knobs.
- Keep it in original containers. No more dumping pills into yogurt cups or pill organizers. The label has vital info in an emergency.
- Use flow restrictors. All new liquid medications come with them-they limit how much can be poured out at once. If yours doesn’t have one, ask your pharmacist for a free one.
- Don’t take meds in front of kids. They imitate. If they see you swallow a pill, they’ll try to copy you.
- Use smart pill bottles. Devices like Hero Health alert you if a dose is missed and lock the bottle if a child tries to open it. They cost $89.99/month, but in high-risk homes, they’ve cut accidental access by 73%.
Starting in 2025, the FDA will require all child-resistant packaging to have two independent safety mechanisms-like a push-and-turn cap plus a child-lock slider. That’s a big step forward. But no packaging is foolproof. Only vigilance is.
Real Stories, Real Consequences
One mother in Ohio delayed calling Poison Control for 45 minutes while searching for her toddler’s pill bottle. He’d swallowed a single 10 mg amlodipine tablet-used for high blood pressure. By the time they got to the hospital, his heart rate had dropped to 42 bpm. He spent 36 hours in cardiac monitoring. Another dad in Texas called Poison Control within three minutes after his child ate three chewable antihistamines. The specialist told him to keep the child awake, give water, and watch for drowsiness. No hospital visit. No IVs. Just a phone call and a calm parent.The difference? One acted on fear. The other acted on knowledge.
What should I do if my child swallows a pill but seems fine?
Call Poison Control at 800-222-1222 immediately. Many dangerous medications have delayed effects. A child may appear normal for hours after swallowing a heart medication or diabetes pill. Never assume they’re okay just because they’re not crying or vomiting. Expert advice is always the safest first step.
Can I use syrup of ipecac to make my child vomit?
No. Syrup of ipecac has not been recommended since 2004. It doesn’t reliably remove toxins and can cause dangerous side effects like prolonged vomiting, dehydration, or aspiration. It delays proper treatment. Poison Control experts will tell you exactly what to do-vomiting is almost never the answer.
How long do I have to act after my child swallows medication?
You have minutes-not hours. The first hour after ingestion is the most critical for treatments like activated charcoal. But even after that, calling Poison Control immediately is essential. Some drugs, like antidepressants or heart medications, can cause sudden, life-threatening changes hours later. Time to expert help matters more than the clock.
Is it safe to wait and see if my child gets sick?
No. Waiting can be deadly. Medications like acetaminophen can cause liver failure 24 to 48 hours after ingestion, with no early symptoms. Beta-blockers can cause heart failure within 30 minutes. You cannot judge the danger by how your child looks. Always call Poison Control first.
What if I don’t know what my child swallowed?
Call Poison Control anyway. They’re trained to help even when you don’t have the bottle. Describe the shape, color, markings, or smell. Tell them how many pills are missing. They can often identify it from your description and give you specific instructions. Don’t wait to find the container-call now.
Can I use the webPOISONCONTROL website instead of calling?
You can use it as a supplement, but never as a replacement for calling. The webPOISONCONTROL tool has 94% accuracy, but it can’t assess breathing, consciousness, or real-time changes. If your child is showing symptoms, call 800-222-1222 immediately. The phone line gives you live, personalized guidance.
What if my child swallowed a medication that’s not theirs?
It doesn’t matter if it’s yours, your partner’s, or a grandparent’s. Any medication not prescribed for that child is a potential poison. The dose, formulation, and active ingredients are designed for adult bodies. A child’s weight and metabolism process drugs differently. Call Poison Control regardless of whose medication it was.
How do I know if a medication is child-resistant?
Look for packaging that requires two separate actions to open-like pushing down while turning the cap, or sliding a tab while pulling. Since 2025, all new child-resistant packaging must have two independent safety mechanisms. But even these aren’t foolproof. Always store medications in a locked cabinet, regardless of the packaging.
What Comes Next
After the emergency, talk to your pediatrician about safety plans. Consider installing smart pill dispensers if you have multiple medications at home. Talk to family members about keeping their meds locked up during visits. Review your home from a child’s eye level: Are pills on the nightstand? Are vitamins in a purse? Is the bathroom cabinet unlocked?This isn’t about blame. It’s about preparation. Accidents happen. But with the right knowledge, you can turn panic into action-and action into safety.

 Atomoxetine and Virtual Reality Therapy: The Future of ADHD Treatment?
Atomoxetine and Virtual Reality Therapy: The Future of ADHD Treatment?
 Proton Pump Inhibitors and Antifungals: How They Interfere With Absorption and Effectiveness
Proton Pump Inhibitors and Antifungals: How They Interfere With Absorption and Effectiveness
 RexMD Sleep Aids and Fast Online Pharmacy Alternatives: Products, Doctor Reviews, and Delivery Insights
RexMD Sleep Aids and Fast Online Pharmacy Alternatives: Products, Doctor Reviews, and Delivery Insights
 How to Keep a Medication List for Safer Care and Fewer Errors
How to Keep a Medication List for Safer Care and Fewer Errors
 Rheumatoid Arthritis: Understanding Autoimmune Joint Damage and Modern Biologic Treatments
Rheumatoid Arthritis: Understanding Autoimmune Joint Damage and Modern Biologic Treatments
Aliza Efraimov
December 30, 2025 AT 06:04I still get chills thinking about when my 2-year-old got into my blood pressure pills. I didn’t even know what to do-just grabbed the phone and called 800-222-1222. The specialist walked me through identifying the pill by its markings while I was on the floor, heart pounding. We didn’t go to the ER. She told me to keep him awake, give sips of water, and check his pulse every 15 minutes. He was fine by midnight. I’ll never not have that number saved in my phone. Ever.
That call saved his life. Not the hospital. Not Google. That one phone call.
Parents-please, just save it. Now.
Nisha Marwaha
January 1, 2026 AT 01:37From a clinical pharmacology standpoint, the critical window for GI decontamination is indeed within the first 60 minutes post-ingestion, particularly for sustained-release formulations or lipophilic agents with delayed absorption kinetics. The utility of activated charcoal is predicated on the absence of contraindications-altered mental status, airway compromise, or ingestion of corrosives. The 2023 AAP guidelines reaffirm that ipecac-induced emesis is not only ineffective but introduces iatrogenic risk via aspiration pneumonia and esophageal mucosal injury. Poison Control’s triage algorithm, which incorporates toxicokinetic modeling based on drug class, dose estimation, and patient weight, reduces unnecessary ED utilization by 43% as cited. Prophylactic use of flow restrictors and smart dispensers like Hero Health demonstrate a 73% reduction in access events in high-risk households. Mandating dual-lock mechanisms per FDA 2025 standards is a necessary, albeit insufficient, step toward systemic prevention.
Paige Shipe
January 2, 2026 AT 13:41I’m sorry but I have to say this: if you can’t keep your meds locked up, you shouldn’t be a parent. I mean, really. You leave your antidepressants on the nightstand like it’s a candy dish? Your child swallows something and you’re surprised? That’s not an accident-that’s negligence. I’ve seen too many parents act like they’re too busy to lock a cabinet but then act like heroes when they call Poison Control. You didn’t save a life-you just avoided the consequences of your own laziness. And don’t even get me started on those ‘smart pill bottles’ that cost $90 a month. Get a lockbox. It’s $12 at Target. Stop making excuses.
And no, I don’t use emoticons. This isn’t a tweet.
Tamar Dunlop
January 3, 2026 AT 08:54As a Canadian parent who has lived through the harrowing experience of a child ingesting a foreign medication during a visit to the United States, I must emphasize the profound difference that immediate access to expert guidance makes. In our case, the Poison Control specialist in Minnesota guided us through identifying a Canadian-brand antihistamine by its distinctive blue-and-white capsule, despite the label being unfamiliar to us. We were able to avoid an ER visit entirely, and the calm, authoritative tone of the professional was the only thing that kept me from spiraling into panic. I have since distributed printed copies of the Poison Help number to every family member who visits our home, regardless of nationality. In times of crisis, clarity is the most powerful antidote. Let us not underestimate the value of preparedness-it is not merely practical, it is profoundly humane.
David Chase
January 4, 2026 AT 21:09THIS IS WHY AMERICA IS STRONGER THAN THE REST OF THE WORLD!!!
Look at this-Poison Control has a 24/7 hotline? IN THE USA?!?!
Other countries? They don’t even have this. In Canada they make you wait 20 minutes on hold. In India? They don’t even have a number. You just pray.
And yet, some of you are still asking if you should call or go to the ER??!!
NO. YOU CALL 800-222-1222. PERIOD. END OF STORY.
SAVE THE NUMBER. TATTOO IT ON YOUR ARM IF YOU HAVE TO. 🇺🇸💪🔥
And yes, I’m mad. Because people still don’t get it. This isn’t a suggestion. It’s a survival protocol. And if you’re not ready, you’re not a parent. You’re a liability.
And if you’re still using syrup of ipecac? You’re a danger to society. 💩
Joe Kwon
January 6, 2026 AT 21:08Just want to add a quiet note: I used to think this was overkill until my niece swallowed a single melatonin gummy. She was fine, but the Poison Control specialist still made me log the time, check her breathing every 10 minutes, and watch for drowsiness for 8 hours. We didn’t go to the hospital. But I learned something: even ‘harmless’ stuff can mess with a kid’s system. I’ve since locked up everything-even my CBD oil and fish oil capsules. Turns out, kids will eat anything that looks like candy. And they’re way more clever than we think. Thanks for the reminder. This stuff matters.
Nicole K.
January 7, 2026 AT 14:43My neighbor’s kid swallowed a whole bottle of Tylenol. She didn’t call Poison Control. She waited until he turned blue. Now he’s in a coma. And she still says she didn’t know it was that serious. I’m not judging-just saying, if you don’t know what to do, you should never be left alone with a child. That’s not mean. That’s fact. You don’t get to wing it with other people’s lives.
Fabian Riewe
January 9, 2026 AT 00:26Biggest thing I learned after my daughter got into my dad’s blood pressure meds? Don’t panic. Just act. I called Poison Control, grabbed the bottle, and started reading the label out loud while they asked me questions. They knew exactly what to do. We didn’t go to the hospital. No IVs. No scary machines. Just a calm voice on the phone telling me what to watch for. I still keep the number on my fridge, next to the fire extinguisher. I don’t care if you think it’s dramatic-it’s the best $0 investment I’ve ever made. Seriously. Save the number. Now. You’ll thank yourself later.
Amy Cannon
January 9, 2026 AT 00:42It is with the utmost gravity and solemn regard for the sanctity of child safety that I feel compelled to underscore the profound imperative of institutionalizing the knowledge of the Poison Control hotline as a non-negotiable component of parental literacy. The statistical efficacy of early intervention-particularly the 43% reduction in hospital admissions-is not merely a figure; it is a moral imperative. The failure to embed this information within the foundational framework of domestic education, whether through pediatric visits, school curricula, or public health campaigns, constitutes a systemic dereliction of duty. Furthermore, the persistence of outdated practices such as the use of syrup of ipecac, despite its unequivocal disavowal by the American Academy of Pediatrics since 2004, reveals a troubling dissonance between medical consensus and public behavior. It is not enough to possess knowledge; one must disseminate it with the urgency of a life hanging in the balance. Let us not wait for tragedy to compel action. Let us act now, with precision, with compassion, and with unwavering resolve.
Himanshu Singh
January 9, 2026 AT 04:45My cousin’s kid ate a whole pack of baby aspirin. He was fine after calling Poison Control, but I didn’t know the number till then. Now I have it saved in my phone, on my watch, even wrote it on my bathroom mirror. I keep forgetting to spell ‘Poison’ right-always write ‘poision’ by mistake. But I remember the number. 800-222-1222. Don’t wait. Just call. Even if you think it’s nothing. Better safe than sorry.