Every year in the U.S., about 7,000 people die because of medication errors. Many of these deaths aren’t caused by bad doctors or faulty drugs-they’re caused by simple mistakes: a pill forgotten, a dose doubled, or a drug interaction missed because no one knew what else the patient was taking. The fix isn’t high-tech. It’s not expensive. It’s just a list. A clear, updated, honest list of every medication you take-prescription, over-the-counter, vitamin, herb, or supplement.
Why Your Medication List Matters More Than You Think
You might think, "I only take a few pills. I know what they are." But here’s the truth: most people forget something. Maybe it’s the ibuprofen you take for your knee. Or the fish oil your cousin swore by. Or the melatonin you only use when you can’t sleep. These aren’t "real" meds to you-but to your body, they interact. To your pharmacist, they matter. To your doctor during an emergency, they could be life-or-death. The Joint Commission, the group that sets hospital safety standards in the U.S., calls accurate medication lists a National Patient Safety Goal. Why? Because when you move from hospital to home, from doctor to ER, from one specialist to another, no one has the full picture unless you bring it. A 2020 study found that if medication lists were kept accurately, up to 80% of errors during care transitions could be prevented. That’s over 1.5 million avoidable adverse drug events each year.What to Include on Your Medication List
A good list isn’t just a scribble on a napkin. It needs details. Here’s what to write down for every medication:- Drug name-both brand (like Lipitor) and generic (atorvastatin)
- Strength and dose-5 mg, 10 mg, 1 tablet
- Frequency-once daily, twice a day, every 6 hours
- Route-by mouth, injection, cream, inhaler
- Purpose-why you take it (e.g., "for high blood pressure," "for joint pain")
- Time of last dose-especially helpful if you’re in the hospital or ER
- Prescribing provider-which doctor gave you this prescription
Choose Your Format: Paper, App, or EHR
There’s no one-size-fits-all. Pick what works for you.Paper Lists
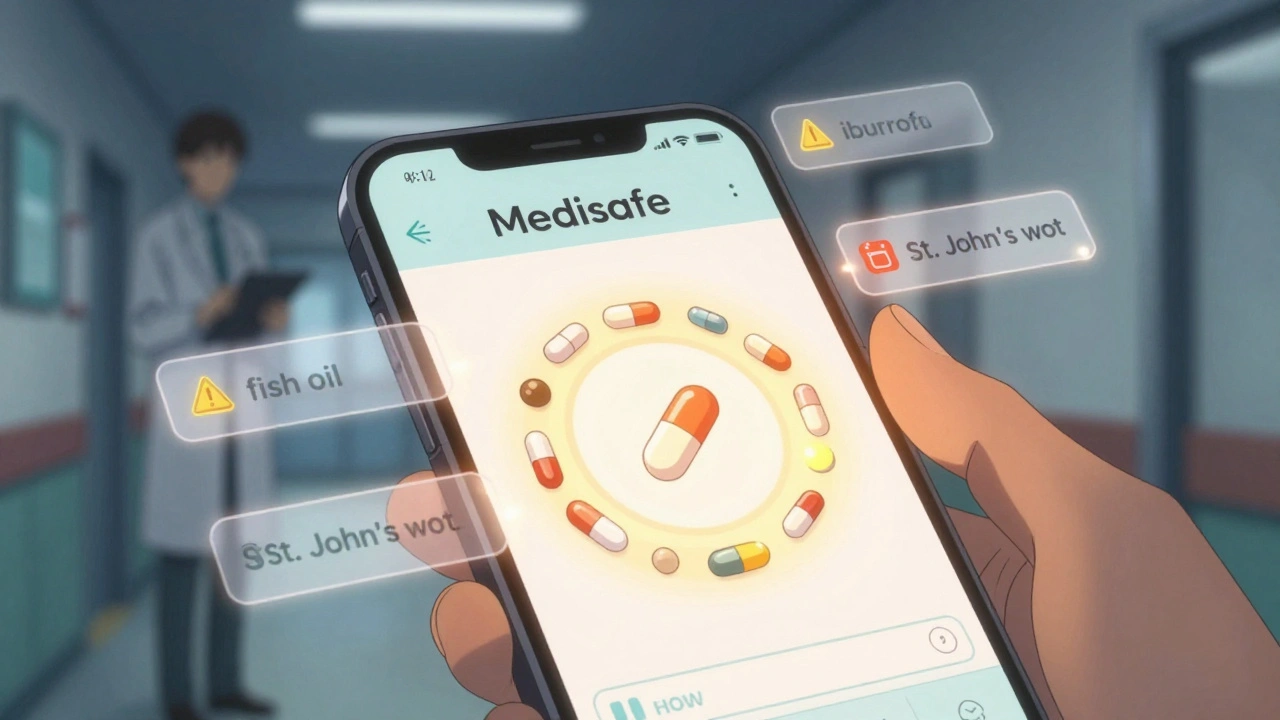
The FDA’s free My Medicines template is simple, printable, and doesn’t need batteries. It has sections for allergies, emergency contacts, and a table for each medication. Many seniors prefer this because it’s tactile and familiar. But here’s the catch: paper doesn’t update itself. If you start a new drug, you have to remember to write it down. And if you lose it? You’re back to square one.Smartphone Apps
Apps like Medisafe, MyTherapy, and CareZone let you scan pill bottles, set reminders, and share your list with family or doctors. Medisafe has over 6 million users. One study in BMJ Open found users missed 28% fewer doses because of the reminders. But adoption among people over 65? Only 35%, according to Pew Research. If you’re not tech-savvy, these can feel overwhelming. Some users complain about cluttered interfaces.Electronic Health Record (EHR) Portals
If you use MyChart (Epic), MyHealtheVet (VA), or another patient portal, check if your provider lets you view or edit your medication list. Kaiser Permanente’s system lets patients update their own lists-and they saw a 22% drop in medication-related readmissions after rolling this out. The problem? Only 58% of primary care practices in the U.S. offer this feature. And even if you update it online, your doctor might not see it unless they pull up your record during a visit.How to Keep It Updated-Without Forgetting
The biggest reason medication lists become useless? They’re not updated. A 2021 University of Michigan study found 68% of patients didn’t update their list after leaving the hospital. That’s dangerous. Here’s how to make updating automatic:- Set a monthly reminder-every first Sunday, open your list and check: any new meds? Any stopped? Any dose changes?
- Use the "brown bag method"-once a year, or after any hospital visit, put all your pills, bottles, and supplements in a brown bag and take them to your doctor. They’ll match what’s on your list with what’s in your bag. This catches hidden meds you forgot about.
- Take a photo-when you get a new prescription, snap a picture of the bottle. Save it in a folder called "Medications." It’s easier than typing everything out.
- Sync refills-ask your doctor if you can get 90-day supplies for chronic meds (like blood pressure or cholesterol drugs). That means fewer refills, fewer chances for confusion, and fewer opportunities for your list to go stale.
When to Review Your List
Don’t wait for an emergency. Review your list at these key moments:- Before every doctor’s appointment
- After a hospital stay or ER visit
- After a new prescription is filled
- After a pharmacist suggests a change
- After you stop a medication-even if you think it didn’t help
- Every six months, even if nothing changed
Common Mistakes (And How to Avoid Them)
People make the same errors over and over:- "I don’t need to list vitamins."-Wrong. St. John’s wort can cancel out antidepressants. High-dose vitamin K can make blood thinners useless.
- "My doctor knows what I take."-Maybe not. Most doctors see 20+ patients a day. They won’t remember your fish oil.
- "I only take it when I need it."-That’s fine, but write it down. "As needed for pain" means nothing if the ER doctor sees you’re on 5 other painkillers.
- "I’ll remember."-You won’t. Stress, illness, or aging can make memory unreliable. A list is your backup brain.
Who Can Help You?
You don’t have to do this alone.- Your pharmacist-They’re medication experts. Many offer free Medication Therapy Management (MTM) under Medicare Part D. They’ll review your list, spot interactions, and help you organize.
- Your primary care doctor-Ask them to review your list at every visit. Bring your list. Don’t assume they’ve seen it.
- A family member-If you’re older or managing multiple conditions, have someone else check your list monthly. Two sets of eyes catch more errors.
Real Stories, Real Risks
A 72-year-old man in Boston was admitted to the hospital for chest pain. He told the nurse he took "a pill for his heart." He didn’t mention the blood thinner he’d been on for years. The hospital gave him aspirin. He had a major bleed. His list was outdated. A woman in Chicago took ibuprofen daily for arthritis. She didn’t think it counted. When she went to the ER for dizziness, the doctor prescribed a new blood pressure drug. The combination caused her kidneys to fail. Her list didn’t include the OTC meds. These aren’t rare. The ECRI Institute recorded over 1,200 medication list-related incidents in 2022 alone. Most were preventable.Your Action Plan
Start today. Here’s what to do:- Grab a piece of paper or open a notes app.
- Write down every medication you’ve taken in the last 30 days-even if you stopped it.
- Include OTC, vitamins, herbs, and supplements.
- For each, write the dose, frequency, and why you take it.
- Print it or save it on your phone. Keep a copy in your wallet.
- Set a calendar reminder: "Update meds" every first Sunday.
- Bring it to your next appointment. Ask: "Is this list complete?"
Final Thought
Your medication list isn’t just paperwork. It’s your safety net. It’s the thing that tells a doctor, "This person is not just taking what’s on my screen. Here’s the full story." It’s the reason you don’t end up in the ER because someone didn’t know you were taking aspirin and a new blood thinner. It’s simple. It’s free. And it could save your life.Do I need to list vitamins and supplements on my medication list?
Yes. Vitamins, herbal remedies, and dietary supplements can interact with prescription drugs. For example, St. John’s wort can reduce the effectiveness of birth control pills and antidepressants. High doses of vitamin K can interfere with blood thinners like warfarin. Even fish oil can increase bleeding risk when taken with aspirin or anticoagulants. If you take it, write it down.
How often should I update my medication list?
Update your list every time you start, stop, or change the dose of any medication-even if it’s temporary. Set a monthly reminder to review it. Also update it after every hospital stay, ER visit, or new prescription. Even if nothing changed, check it every six months. Studies show most lists become outdated within 30 days of a medication change.
Is it better to use a paper list or a smartphone app?
It depends on your comfort level. Paper lists are reliable and don’t need batteries or internet access. They’re great for older adults or those who prefer physical copies. Apps like Medisafe or MyTherapy offer reminders and can share your list with caregivers, but they require tech skills. Many people use both: a printed copy for emergencies and an app for daily tracking.
Can my doctor see my medication list if I use an app?
Only if you share it. Most apps don’t connect directly to your doctor’s electronic health record. You’ll need to email it, print it, or show it on your phone during your visit. Some patient portals (like MyChart) let you view and update your list directly in your provider’s system-if your clinic uses that feature. Always confirm your doctor has seen your updated list.
What should I do if I can’t remember all my medications?
Bring all your pill bottles to your next appointment. This is called the "brown bag method." It’s the most accurate way to rebuild your list. Your pharmacist can also help-they have records of all your filled prescriptions. If you’re unable to do this yourself, ask a family member or caregiver to help you gather the bottles.
Are there free templates I can use?
Yes. The FDA offers a free, printable "My Medicines" template that includes space for allergies, emergency contacts, and all medication details. The American Heart Association also provides downloadable worksheets. You can find these by searching "FDA My Medicines template"-no login or cost required.
Can a pharmacist help me manage my medications?
Yes. Many pharmacies offer free Medication Therapy Management (MTM) services under Medicare Part D. A pharmacist will review your entire list, check for interactions, simplify your regimen, and help you understand why you take each drug. You don’t need to be sick to qualify-just take multiple medications. Ask your pharmacy if they offer this service.

 How Effective Is Calcipotriene for Treating Nail Psoriasis?
How Effective Is Calcipotriene for Treating Nail Psoriasis?
 Pharmacy Counseling: What to Learn When Picking Up Generics
Pharmacy Counseling: What to Learn When Picking Up Generics
 Discover the Benefits of Coca: The Revolutionary Dietary Supplement
Discover the Benefits of Coca: The Revolutionary Dietary Supplement
 Appearance Differences: Why Authorized Generics Look Different from Brand-Name Drugs
Appearance Differences: Why Authorized Generics Look Different from Brand-Name Drugs
sharon soila
December 14, 2025 AT 06:45Every single person should do this. It’s not complicated. It’s not expensive. It’s just common sense. I keep mine in my wallet and update it every Sunday. My mom didn’t, and she ended up in the ER because they didn’t know she was on blood thinners. Don’t be her. Start today.
Rawlson King
December 14, 2025 AT 13:59People still need a guide for this? In 2024? You’re telling me a 72-year-old man can’t remember he’s on warfarin? This isn’t a safety issue-it’s a failure of basic personal responsibility. If you can’t track your own pills, maybe you shouldn’t be managing them alone.
Tommy Watson
December 16, 2025 AT 07:35OMG I JUST REALIZED I FORGOT MY TURMERIC SUPP IN MY LIST 😭 I’VE BEEN TAKING IT FOR 3 YEARS AND MY DOCTOR THOUGHT I WAS JUST A HEALTH NUT. NOW I’M SCARED I’M GONNA BLEED OUT IN MY SLEEP. WHO DO I EVEN TALK TO??
Karen Mccullouch
December 16, 2025 AT 09:09This is why America’s healthcare is broken. We’re not teaching people to be responsible. We’re just handing out apps and templates like candy. Meanwhile, Big Pharma is laughing all the way to the bank. If you’re taking more than 3 pills, you’re already a statistic. This list? It’s not a fix. It’s damage control.
Lauren Scrima
December 16, 2025 AT 20:59Wait-you’re telling me I need to write down my vitamin D? And my melatonin? And my CBD gummies? And my neighbor’s "miracle" turmeric tincture? 😂 I’ve been doing this for years. I keep it in my Notes app. I even color-code by category. Blue = prescription, green = OTC, pink = "I think this might help?"
Jamie Clark
December 17, 2025 AT 13:09Let’s be honest: the system doesn’t want you to have a complete list. Why? Because if you did, you’d question every prescription. You’d notice the overlap. You’d ask why you’re on five painkillers and three antidepressants. The real danger isn’t the missing pill-it’s the fact that no one ever asks you if you still need any of it.
Keasha Trawick
December 18, 2025 AT 00:53This is the most vital health hack since seatbelts. Think of your meds like a symphony-every note matters. Miss one? The whole piece collapses. I use Medisafe + a printed copy in my purse. I also screenshot every Rx bottle. My pharmacist calls me when my lisinopril refills are due. She knows my name, my cats’ names, and the fact that I take fish oil for my anxiety. She’s my MVP.
Webster Bull
December 19, 2025 AT 11:02Just do it. It takes 10 minutes. Use your phone. Take pics. Write it down. No excuses. I’m 68. I don’t use apps. I use a notebook. I keep it next to my coffee mug. Every morning I check it. If I don’t, I don’t take my pills. Simple. Works.
Deborah Andrich
December 20, 2025 AT 12:55I used to think this was overkill. Then my aunt had a stroke and they didn’t know she was on St. John’s wort. It canceled her blood thinner. She didn’t make it. I carry her list now. I update it. I show it to every new doctor. It’s not just a list. It’s a promise. To her. To me. To anyone who might have to make a decision when I can’t speak.
Jennifer Taylor
December 20, 2025 AT 19:18WAIT. SO THEY’RE SAYING WE CAN’T TRUST OUR DOCTORS? WHAT IF THE LIST GETS STOLEN? WHAT IF THE APP IS HACKED? WHAT IF THE GOVERNMENT USES IT TO TRACK OUR MEDS? I HEARD THEY’RE PLANNING TO MAKE EVERYONE UPLOAD THEIR PILLS TO A FEDERAL DATABASE. THIS IS THE FIRST STEP TO MEDICAL CONTROL. WE NEED TO FIGHT THIS.
Shelby Ume
December 21, 2025 AT 21:47My mother is 82 and has 14 medications. I help her update her list every Sunday. We sit with her pill organizer, her prescriptions, and her tea. We talk about how she’s feeling. We laugh. We cry. It’s not just about safety-it’s about connection. She says this is the only time she feels truly heard. That’s worth more than any app.
Jade Hovet
December 23, 2025 AT 13:23OMG I JUST UPDATED MY LIST AND ADDED MY GUMMY VITAMINS 😍 I’M SO PROUD OF MYSELF!! 🎉💖 I even took a pic of my fish oil bottle and labeled it "for brain fog + mood" 🤓📱 #MedListWin #HealthIsWealth #IGotThis
nithin Kuntumadugu
December 25, 2025 AT 01:44USA healthcare is a scam. You think a list will save you? Nah. The real problem? Doctors don’t read your list. Pharmacies don’t cross-check. Apps are just for show. This whole thing is a distraction. They want you to feel safe so you don’t ask why your insulin costs $300. The list won’t fix that. Only revolution will.
John Fred
December 26, 2025 AT 05:45Just did my list. Used MyChart + printed it. My PCP said, "I’ve never seen a patient do this." I told him: "Then you’re not seeing the full picture." He actually smiled. That’s the moment I realized: this isn’t just about safety. It’s about dignity. You deserve to be seen. Full stop.