When you pick up a prescription and see a pill that looks completely different from what you’ve been taking, it’s natural to pause. Generic medications are everywhere now-91% of all prescriptions filled in the U.S. are generics. But many people still wonder: Is this really the same? Will it work? Could it hurt me? The answer isn’t just yes or no-it’s about what you’re told when you walk up to the counter.
Why Your Pill Looks Different
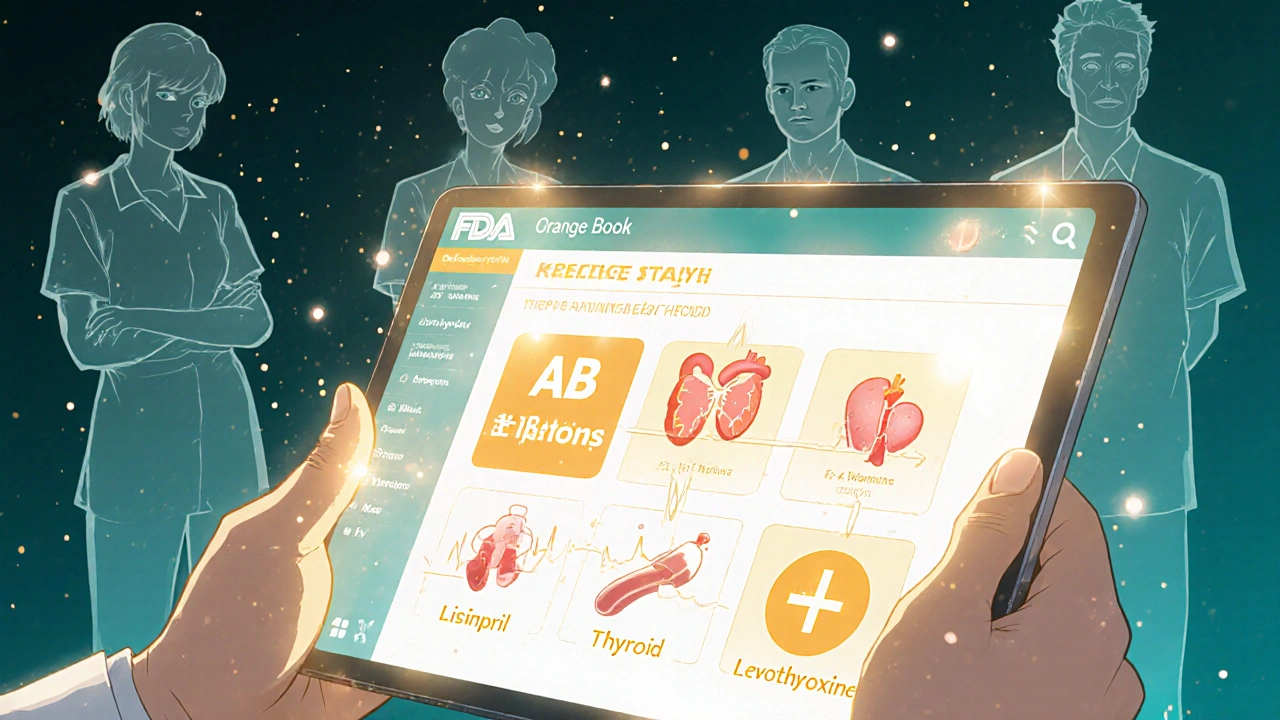
Generic drugs aren’t copies in the way a photocopy is a copy. They’re exact matches in active ingredients, strength, and how they work in your body. The FDA requires that every generic drug deliver the same therapeutic effect as the brand-name version. That means if your brand-name blood pressure pill lowers your systolic pressure by 15 points, the generic must do the same-within a tiny, scientifically accepted range of 80% to 125% effectiveness.So why does it look different? The color, shape, size, and even the imprint on the pill come from inactive ingredients-things like dyes, fillers, and binders. These don’t affect how the drug works, but they can cause confusion. One patient told me they stopped taking their generic thyroid pill because it was white instead of blue. They thought the color change meant it wasn’t working. Their pharmacist later showed them the FDA’s Orange Book entry proving the active ingredient was identical. They restarted the medication and saved $280 a month.
What Pharmacists Are Required to Tell You
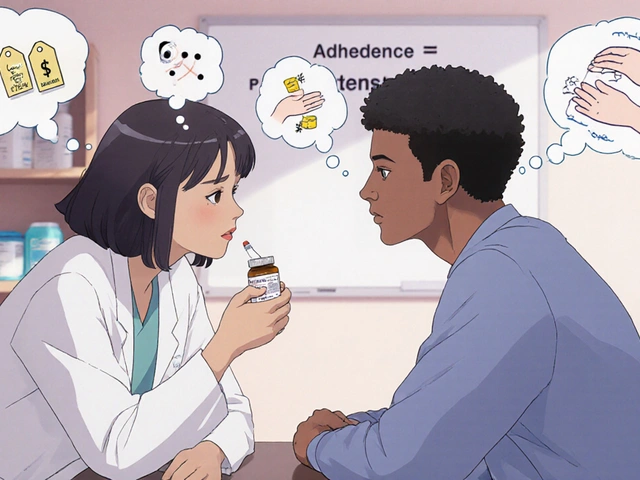
By law, pharmacists must counsel you when you get a generic drug. This isn’t optional-it’s part of Medicaid rules and required in every state. The counseling isn’t just a quick “Here’s your medicine.” It’s a short conversation designed to clear up misunderstandings. Here’s what they should cover:- The difference between the brand name and generic name (e.g., lisinopril instead of Zestril)
- Why the generic is cheaper (no marketing costs, no patent)
- That the active ingredient is identical to the brand
- That the FDA requires the same quality, purity, and stability
- That inactive ingredients might differ-and why that matters if you have allergies
- How to take it, when, and what side effects to watch for
Pharmacists are trained to use the “teach-back” method: they ask you to explain it back in your own words. If you say, “So this is just a cheaper version of my old pill?” they’ll correct you: “It’s not cheaper because it’s weaker. It’s cheaper because the company didn’t pay to invent it.”
What You Need to Ask
Don’t wait for them to bring it up. If you’re handed a new pill, ask these three questions:- “Is this a generic version of my previous medication?” If yes, ask why the change happened. Was it your insurance? Your doctor? The pharmacy?
- “Are there any differences in the inactive ingredients?” This is critical if you’re allergic to lactose, gluten, or certain dyes. Some generics use different fillers, and those can trigger reactions-even if the active drug is perfect.
- “Can I see the FDA’s therapeutic equivalence rating for this?” Most pharmacists can pull up the Orange Book on their computer. Look for the “AB” rating. That means it’s approved as equivalent. Avoid any drug with an “BX” rating-it means there’s not enough data to confirm equivalence.
One patient, John, had a bad reaction to a generic blood pressure pill. He didn’t know he was allergic to lactose, and the generic contained it. His brand didn’t. He didn’t ask. The pharmacist didn’t volunteer it. He ended up in the ER. That’s why asking matters.
When Generics Might Not Be the Best Choice
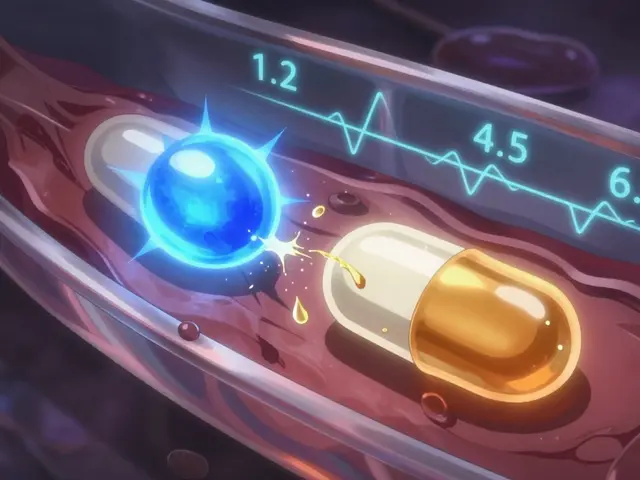
Most of the time, generics are perfect. But there are exceptions. Some drugs have a narrow therapeutic index-meaning the difference between a helpful dose and a dangerous one is very small. For these, even tiny changes in how the body absorbs the drug can matter.Drugs like warfarin (blood thinner), levothyroxine (thyroid), and phenytoin (seizure control) fall into this category. In 23 states, pharmacists can’t automatically switch you to a generic for these without your doctor’s approval. Even then, some doctors prefer to stick with the brand for stability. If you’re on one of these, ask your pharmacist: “Is this substitution safe for my specific condition?”
Studies show that patients on these drugs who switch generics without monitoring have a slightly higher risk of hospitalization. It’s not common-but it’s real enough to warrant caution.
Why Counseling Actually Works
A 2018 study tracked 12.7 million people on chronic medications. Those who got proper counseling when switching to generics had an 8.2% increase in adherence. That means they took their pills more consistently. Why? Because they understood why the change happened. They weren’t afraid.Another study found that patients who received video counseling-short clips explaining how generics work-were 37% more likely to accept the switch. They felt more in control. That’s the power of clear communication.
On the flip side, 31% of patients reported confusion when their pill changed appearance. 18% admitted they skipped doses because the pill looked “wrong.” That’s not a failure of the drug. It’s a failure of the conversation.

What to Do If You’re Still Unsure
If you’re still nervous, here’s what you can do:- Ask your pharmacist to show you the FDA Orange Book entry for your drug. It’s free and public.
- Check the manufacturer’s name on the bottle. Many generics are made by the same companies that make brand-name drugs.
- If you notice a change in how you feel after switching-fatigue, dizziness, mood swings-call your doctor or pharmacist. Don’t assume it’s “all in your head.”
- Keep a simple log: date, pill appearance, how you felt. This helps your provider spot patterns.
One woman, Sarah, kept a notebook. When she switched to a generic for her cholesterol drug, she wrote: “Day 3: no chest tightness. Day 7: energy back to normal.” She showed it to her doctor. He told her: “You’re doing exactly what I want you to do.”
How This Saves You Money-Without Sacrificing Care
Since 2009, generic drugs have saved the U.S. healthcare system over $1.9 trillion. That’s not just corporate profit-it’s lower co-pays, fewer hospital visits, and less financial stress for patients. But that savings only happens if people take their meds.When counseling works, adherence goes up. When adherence goes up, complications go down. When complications go down, costs drop further. It’s a cycle that only works when patients understand what they’re taking.
Generic drugs aren’t second-rate. They’re the result of 40 years of FDA oversight, clinical testing, and real-world data. The only thing missing is the conversation.
Next time you get a generic, don’t just take it. Ask. Listen. Confirm. Your health-and your wallet-will thank you.

 Guide to Affordable Cialis Soft Online: Maximizing Sexual Health
Guide to Affordable Cialis Soft Online: Maximizing Sexual Health
 How to Appeal a Prior Authorization Denial for Your Medication
How to Appeal a Prior Authorization Denial for Your Medication
 What Is Medication Adherence vs. Compliance and Why It Matters
What Is Medication Adherence vs. Compliance and Why It Matters
 Modified-Release Formulations: What You Need to Know About Bioequivalence Standards
Modified-Release Formulations: What You Need to Know About Bioequivalence Standards
 How Azilsartan Affects Blood Pressure in Psoriasis Patients
How Azilsartan Affects Blood Pressure in Psoriasis Patients
Shawn Daughhetee
November 24, 2025 AT 21:29Just got my generic blood pressure pill and thought I got scammed till I read this. Same active stuff, just cheaper. No more panic attacks at the pharmacy counter. Thanks for the clarity.
Miruna Alexandru
November 25, 2025 AT 19:24It's fascinating how societal distrust in pharmaceuticals manifests as visual bias-people equating aesthetic deviation with functional inadequacy. The FDA's AB rating system is a triumph of empirical rigor, yet the public remains tethered to the myth of brand as quality. This isn't pharmacology-it's consumer semiotics. The pill's color is a Rorschach test for anxiety.
Justin Daniel
November 26, 2025 AT 10:41Love how this post doesn't just dump facts but shows you how to talk to your pharmacist like a human. I used to feel dumb asking questions, but now I just say, 'Hey, can you show me the Orange Book?' and they light up. Turns out pharmacists are secret superheroes. Also, my generic metoprolol saved me $150/month. Win.
Melvina Zelee
November 28, 2025 AT 02:17so like i switched to generic levothyroxine last year and at first i was like oh no my energy is gone and my brain feels fuzzy but then i remembered to check the filler and turns out it had lactose and i’m lactose intolerant 😅 so i asked my doc to switch back to the brand or find a lactose-free generic and now im back to normal. point is: dont be shy to ask about the junk inside the pill. its not just the magic stuff that matters. also, keep a journal like sarah did. its weirdly empowering.
ann smith
November 29, 2025 AT 14:40This is such an important message. 💙 So many people skip doses because they're scared-this helps turn fear into understanding. Thank you for sharing practical steps. I'm sharing this with my mom. She’s 72 and still thinks generics are 'cheap knockoffs.' Maybe this will help her see the truth.
Latonya Elarms-Radford
November 30, 2025 AT 03:35Oh, the tragedy of modern medicine-where the soul of pharmaceutical care has been reduced to a transactional exchange between a disengaged pharmacist and a terrified patient, all because we’ve outsourced empathy to corporate cost-cutting. The FDA’s ‘AB’ rating? A bureaucratic euphemism for ‘we’re not going to stop you, even though you might be dying.’ And yet, we’re told to be grateful for the savings. What a grotesque irony: a system that saves billions while eroding trust in the very foundation of healing. I weep for the woman who stopped her thyroid pill because it was white instead of blue. She didn’t just lose a pill-she lost faith in the entire structure meant to protect her.
Mark Williams
November 30, 2025 AT 08:55Therapeutic equivalence is a pharmacokinetic concept, not a marketing one. The 80–125% AUC range is statistically validated across bioequivalence trials, yet public perception remains anchored in perceptual heuristics-color, shape, imprint. The real issue isn’t the drug-it’s the lack of translational education. We need standardized, evidence-based counseling protocols embedded in pharmacy workflows, not left to the discretion of overworked technicians. Also, BX-rated drugs should be flagged at the EHR level-automated alerts could prevent 70% of adverse switches.
Ravi Kumar Gupta
December 2, 2025 AT 05:43In India, we call generics 'sasta dawa'-cheap medicine. But here’s the truth: same pill, same results, same life saved. My uncle took generic warfarin for 8 years, saved enough to send his granddaughter to college. The color changed three times-he didn’t care. He cared that he could breathe. Stop overthinking the pill. Start caring about the person holding it.