INR Elevation Calculator
Expected INR After Trimethoprim-Sulfamethoxazole
When you're on warfarin, even a simple antibiotic can throw your blood thinning off balance - sometimes dangerously so. One of the most dangerous and commonly overlooked interactions happens when trimethoprim-sulfamethoxazole (also known as Bactrim or Septra) is mixed with warfarin. The result? A sudden, unpredictable spike in INR, which can lead to internal bleeding, hospitalization, or even death.
Why This Interaction Is So Dangerous
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. It’s a narrow-margin drug: too little, and you risk clots; too much, and you bleed. Your INR (International Normalized Ratio) tells doctors how long it takes your blood to clot. A normal INR for someone on warfarin is usually between 2.0 and 3.0. If it climbs above 4.0, your bleeding risk starts rising sharply. Above 5.0, the danger becomes serious. Trimethoprim-sulfamethoxazole (TMP-SMX) doesn’t just add to the risk - it multiplies it. Studies show that when this antibiotic is started in someone taking warfarin, INR increases by an average of 1.8 points within just 36 to 72 hours. That’s not a small bump. If your INR was 2.5, it could jump to 4.3 - a level where doctors start panicking. This isn’t just theoretical. Data from the FDA’s adverse event database shows over 1,800 reports of INR spikes linked to TMP-SMX in five years. Nearly half of those cases led to hospitalization. Nearly 70 people died from bleeding complications.How the Interaction Actually Works
It’s not one thing - it’s three things happening at once. First, TMP-SMX blocks the CYP2C9 enzyme. This is the main enzyme your liver uses to break down the most powerful part of warfarin: the S-enantiomer. When this enzyme is slowed down, warfarin builds up in your blood. Clinical studies show clearance drops by 20-30%, meaning you’re getting a stronger dose without increasing the pill. Second, sulfamethoxazole competes with warfarin for binding sites on albumin. Warfarin is 97-99% bound to proteins in your blood. When another drug like sulfamethoxazole comes along, it pushes warfarin off those proteins. Suddenly, more free warfarin is circulating - and it’s active. Third, TMP-SMX kills off gut bacteria that make vitamin K. Your body gets about 30% of its vitamin K from the bacteria in your intestines. When antibiotics wipe out those bugs, your vitamin K levels dip. That means warfarin has even less to fight against. Put all three together, and you’ve got a perfect storm.Not All Antibiotics Are Created Equal
Some antibiotics barely touch your INR. Others? They’re landmines. - Trimethoprim-sulfamethoxazole: INR increases by 1.8 units on average. High risk. - Ciprofloxacin (a fluoroquinolone): INR increases by 0.9 units. Moderate risk. - Amoxicillin: INR increases by just 0.4 units. Low risk. - Metronidazole: INR increases by 1.5 units. Also high risk. That’s why doctors don’t just say “avoid all antibiotics.” They pick carefully. For a urinary tract infection, nitrofurantoin is often preferred over TMP-SMX in patients on warfarin. For pneumonia, azithromycin might be a better bet than ciprofloxacin.
Who’s Most at Risk?
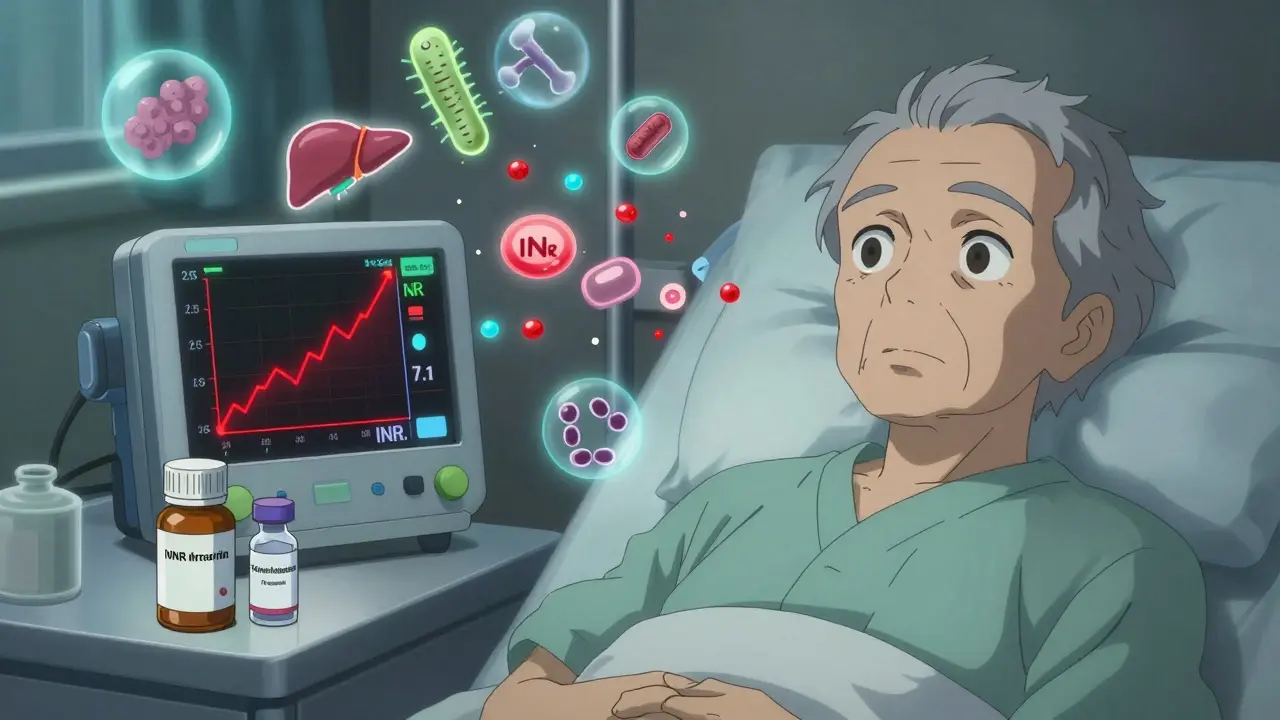
Not everyone reacts the same way. Some people take TMP-SMX and their INR stays stable. Others go from 2.8 to 7.1 in three days. The biggest risk factors:- Age over 75 - metabolism slows down, liver function declines.
- Heart failure - reduced blood flow to the liver means slower drug clearance.
- Liver disease - your liver can’t process warfarin properly.
- Poor nutrition - low vitamin K intake makes you more sensitive.
- Male sex - men are 9% more likely to have a dangerous spike than women, according to a study of over 70,000 patients.
What Doctors Should Do - And What They Often Don’t
The American Heart Association and the American College of Chest Physicians both say: avoid TMP-SMX if you can. But here’s the problem - it’s still prescribed. A 2022 study in JAMA Internal Medicine found that nearly 1 in 5 warfarin patients got a potentially dangerous antibiotic within 30 days. And TMP-SMX made up nearly 30% of those prescriptions. Why? Because it’s cheap, effective, and widely available. A doctor treating a 78-year-old with a UTI might not think twice - especially if they don’t know the patient is on warfarin. Best practice? If TMP-SMX is absolutely necessary:- Check INR before starting the antibiotic.
- Check it again 48 to 72 hours after starting.
- Check it every 3-4 days while on the drug.
- Reduce the warfarin dose by 20-30% preemptively in high-risk patients.
What Happens When INR Goes Too High?
If your INR hits 4.0-5.0 and you’re not bleeding:- Hold 1-2 doses of warfarin.
- Recheck INR in 24-48 hours.
- Restart at a lower dose.
- Give 1-2.5 mg of oral vitamin K.
- Stop warfarin until INR drops.
- Give 5-10 mg of IV vitamin K.
- Infuse 4-factor prothrombin complex concentrate (PCC) - this reverses warfarin fast.
- Admit to hospital.

What Patients Need to Know
You don’t need to understand CYP2C9 enzymes. But you do need to know this:- If you’re on warfarin, tell every doctor, pharmacist, and nurse before they give you any new medicine - even over-the-counter stuff.
- If you’re prescribed Bactrim, Septra, or any sulfa-based antibiotic, ask: “Is this safe with my blood thinner?”
- Know your baseline INR. Keep a log.
- Watch for signs of bleeding: unusual bruising, pink or red urine, bloody stools, severe headaches, dizziness.
- If you start a new antibiotic, get your INR checked within 72 hours - don’t wait for symptoms.
What About Newer Blood Thinners?
Direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, and dabigatran don’t interact with TMP-SMX the same way. That’s why many patients have switched from warfarin. But here’s the catch: 2.6 million Americans are still on warfarin in 2026. Why?- People with mechanical heart valves - DOACs aren’t approved for them.
- People with severe kidney disease - DOACs can build up.
- People on Medicare - warfarin costs $10 a month; DOACs cost $300.
Bottom Line
Trimethoprim-sulfamethoxazole and warfarin don’t mix. Not safely. Not reliably. Not without close monitoring. If you’re on warfarin:- Don’t take TMP-SMX unless there’s no other option.
- If you must take it, get your INR checked within 72 hours.
- Know the signs of bleeding - and act fast.
- Check the patient’s anticoagulant list before prescribing antibiotics.
- Use nitrofurantoin or azithromycin instead of TMP-SMX when possible.
- Don’t assume the patient knows the risk.
Can I take Bactrim if I’m on warfarin?
Bactrim (trimethoprim-sulfamethoxazole) should be avoided if possible when you’re on warfarin. It can cause your INR to spike dangerously high within 2-3 days, increasing your risk of severe bleeding. If no other antibiotic will work for your infection, your doctor may prescribe it - but only after checking your INR before and within 72 hours of starting the drug, and possibly reducing your warfarin dose.
How quickly does INR rise after starting TMP-SMX?
INR typically starts rising within 24-48 hours after starting trimethoprim-sulfamethoxazole, with the peak effect usually seen by day 3. This is why it’s critical to check your INR within 72 hours of beginning the antibiotic - waiting for symptoms like bruising or bleeding means it’s already too late.
What antibiotics are safe with warfarin?
Antibiotics with minimal interaction risk include amoxicillin, ampicillin, and azithromycin. Nitrofurantoin is often preferred for urinary tract infections in patients on warfarin. Always check with your doctor or pharmacist before starting any new antibiotic - even if it’s over-the-counter or for a minor infection.
What should I do if my INR goes above 5.0?
If your INR is above 5.0 and you’re not bleeding, your doctor will likely have you skip 1-2 warfarin doses and give you 1-2.5 mg of oral vitamin K. If you’re bleeding - even mildly - you need medical attention immediately. For INR above 10 with active bleeding, you’ll need IV vitamin K and a clotting factor concentrate called PCC. Never try to adjust your dose on your own.
Why do some people on warfarin take TMP-SMX without problems?
Individual differences in metabolism, liver function, gut bacteria, and genetics (like CYP2C9 and VKORC1 variants) affect how your body handles the interaction. Some people naturally clear warfarin faster or have more vitamin K from their diet. But you can’t predict who’s safe - so no one should assume they’re an exception. Always assume risk until proven otherwise with testing.
 Serum Sickness-Like Reactions to Antibiotics: What Parents and Doctors Need to Know
Serum Sickness-Like Reactions to Antibiotics: What Parents and Doctors Need to Know
 How to Use Travel Health Clinics for Pre-Trip Medication Planning
How to Use Travel Health Clinics for Pre-Trip Medication Planning
 Organ Donation Awareness: How It Lowers Transplant Rejection Rates
Organ Donation Awareness: How It Lowers Transplant Rejection Rates
 Wholesale Economics: How Generic Drug Distribution and Pricing Really Work
Wholesale Economics: How Generic Drug Distribution and Pricing Really Work
 Compare Rhinocort (Budesonide) with Alternatives: What Works Best for Nasal Allergies?
Compare Rhinocort (Budesonide) with Alternatives: What Works Best for Nasal Allergies?
Sazzy De
January 31, 2026 AT 20:45Been on warfarin for 8 years and never knew Bactrim could do this. My doc just prescribed it last month for a UTI. I got my INR checked a week later and it was 4.1. Scared the hell out of me. Glad I didn't ignore the bruising.
Now I always ask about antibiotics before they write anything. Simple question, maybe saves your life.
KATHRYN JOHNSON
February 2, 2026 AT 02:46It is imperative that healthcare providers be held accountable for failing to screen for clinically significant drug interactions. The data presented is unequivocal. Prescribing trimethoprim-sulfamethoxazole to patients on warfarin constitutes a breach of the standard of care.
Amy Insalaco
February 3, 2026 AT 15:52Frankly, the entire pharmacokinetic model here is oversimplified. The CYP2C9 inhibition is well-documented, but the albumin displacement hypothesis is largely theoretical and contradicted by plasma protein binding studies from the 90s. The real culprit is the gut microbiome disruption-specifically, the depletion of Bacteroides fragilis and its vitamin K2 synthesis pathways, which is a far more nuanced and underappreciated mechanism.
Also, the 2022 JAMA study cited doesn’t control for INR monitoring frequency, so the causality is confounded. We need longitudinal cohort analyses with genotyped CYP2C9/VKORC1 variants to truly quantify risk.
And let’s not forget the confounding effect of dietary vitamin K intake variability-kale consumption alone can swing INR by 0.7 points in sensitive patients.
Marc Bains
February 4, 2026 AT 22:38As a nurse practitioner in rural Ohio, I see this every month. Elderly patients come in with bloody stools, and we find out they got Bactrim from the urgent care down the road. No one asked about their blood thinner.
That’s why I started handing out laminated cards to every warfarin patient: ‘ASK BEFORE YOU TAKE ANY NEW MED.’
It’s not fancy, but it works. We’ve cut our emergency visits by almost half in two years.
Knowledge isn’t power-it’s survival.
owori patrick
February 5, 2026 AT 00:54This is so important. In Nigeria, many people use antibiotics like Bactrim for everything-cold, fever, even headaches. No one checks INR. My uncle died from internal bleeding after taking it for a tooth infection. He didn’t even know he was on warfarin.
We need to educate communities. Not just doctors. Everyone.
Claire Wiltshire
February 6, 2026 AT 22:29For patients on warfarin: keep a printed log of your INR values and the dates you took any new medications. Bring it to every appointment. It’s a simple habit that gives your provider critical context.
Also, if you’re on Medicare and worried about cost, ask about generic warfarin-it’s under $5 a month. DOACs aren’t always the answer, and that’s okay.
Diksha Srivastava
February 7, 2026 AT 15:50You guys are doing amazing work spreading this info. I used to think blood thinners were just for old people, but my grandma almost died from this. Now I’m sharing this post with every person I know on meds. You never know who needs to hear it.
Keep going!
Shubham Dixit
February 9, 2026 AT 09:29Let me tell you something-this whole thing is a Western medical obsession. In India, we’ve been using Bactrim with warfarin for decades. My father, 82, has a mechanical valve and takes both without issue. He eats lots of spinach, drinks buttermilk, and his INR stays stable. You people overcomplicate everything with your enzymes and protein binding and jargon. Real medicine is about outcomes, not lab numbers.
And yes, I know the FDA says it’s dangerous-but we’ve had 30 years of real-world experience here. Maybe your data is biased because you only study people who are already sick or on too many pills.
Don’t scare people into avoiding life-saving antibiotics because of some statistical outlier. Use common sense. Monitor. Don’t panic.
Carolyn Whitehead
February 10, 2026 AT 22:05My dad had a scary INR spike last year after a course of Bactrim. He’s fine now but we’re extra careful. Just wanted to say thank you for writing this. I showed it to his doctor and now they always check before prescribing anything. Small changes matter.
Sidhanth SY
February 11, 2026 AT 07:37My cousin’s cardiologist switched him from warfarin to apixaban just because he got a UTI. Cost went from $12 to $450/month. He’s not rich. I get why DOACs are great, but we can’t just abandon warfarin users. This post? It’s a lifeline for people who can’t afford the upgrade.
Thanks for not making it about ‘better drugs’-but about safety for everyone.