After a colonoscopy finds and removes polyps, many patients assume the job is done. But that’s not true. The real work begins now: knowing when to come back for your next colonoscopy. Get it wrong, and you could miss a growing cancer. Get it right, and you avoid unnecessary procedures, save money, and reduce anxiety. The question isn’t just when to repeat the colonoscopy-it’s why that timing matters, and how your specific polyps change everything.
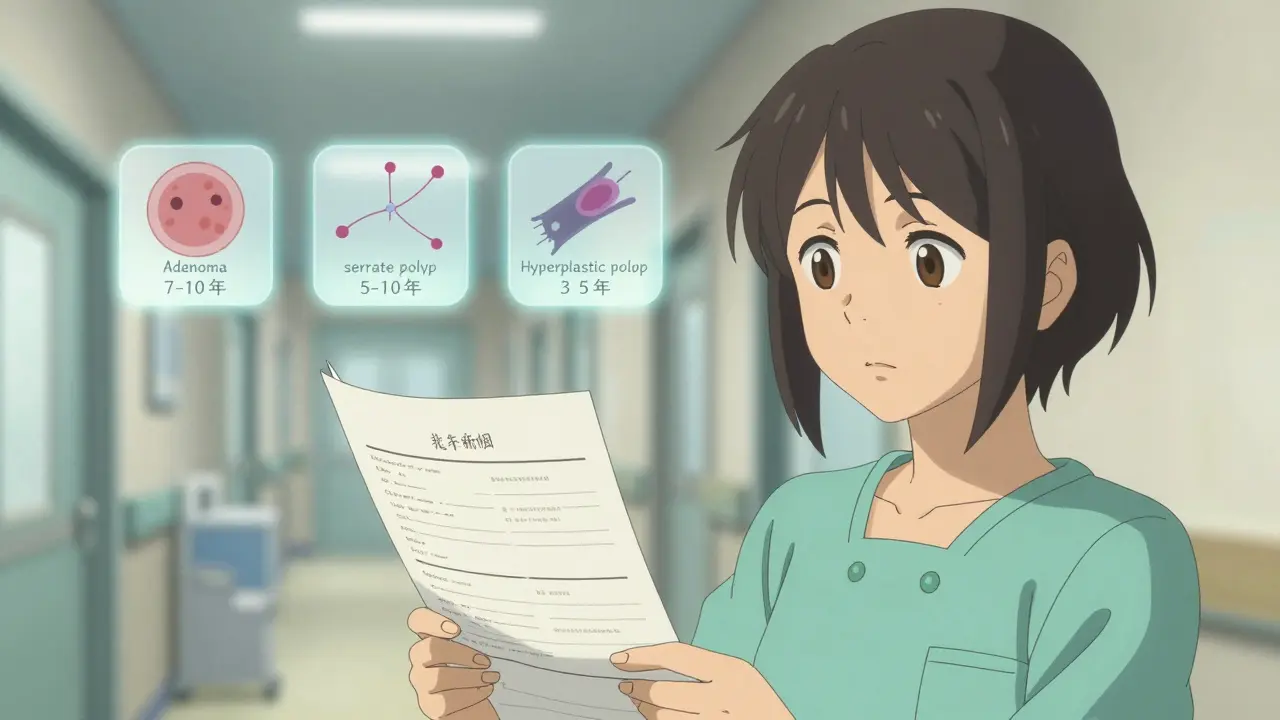
Not All Polyps Are the Same
Polyps aren’t just growths. They’re clues. Some are harmless. Others are warning signs. The key to your next colonoscopy isn’t your age or family history-it’s what the doctor found during your procedure. Three main types matter most: adenomas, serrated polyps, and hyperplastic polyps.Adenomas are the most common precancerous polyps. If you have one or two that are smaller than 10 mm, your risk of developing colon cancer in the next decade is almost the same as someone with a clean colon. That’s why the 2020 guidelines from the US Multi-Society Task Force now recommend waiting 7 to 10 years before your next colonoscopy. This was a big shift from the old 5-year rule. Studies show that 98.7% of people with these small adenomas stay cancer-free after 10 years.
If you have three or four adenomas, all under 10 mm, the clock resets to 3 to 5 years. Why? More polyps mean more chances for something to go wrong. It’s not about size anymore-it’s about quantity. Five or more adenomas, no matter the size, means you need a repeat colonoscopy in 3 years.
Now, if any polyp is 10 mm or larger, has villous features (finger-like projections), or shows high-grade dysplasia (abnormal cells), you’re in the high-risk group. That triggers a 3-year interval, no exceptions. These polyps grow faster and turn cancerous more often.
Serrated Polyps: The Silent Threat
Serrated polyps, especially sessile serrated lesions (SSLs), are sneaky. They look flat and harmless under the scope, but they’re responsible for up to 30% of colon cancers that develop between screenings. That’s why they’re treated differently.If you have one or two SSLs smaller than 10 mm, the current recommendation is 5 to 10 years. But if you have three or four, drop that to 3 to 5 years. Five or more? Back in 3 years. The tricky part? SSLs are often missed during colonoscopy because they blend into the colon lining. If your bowel prep wasn’t perfect, or if the polyp was hard to see, your doctor might shorten the interval just to be safe.
Hyperplastic polyps are usually harmless-but only if they’re small and in the lower colon. If you have a hyperplastic polyp that’s 10 mm or larger, or if it’s in the right side of the colon, treat it like an SSL. That means a 3 to 5 year follow-up. Why? Because it’s hard to tell them apart without a biopsy, and misclassifying one could cost you years of safety.
What Happens When Polyps Are Removed in Pieces?
Sometimes, a polyp is too big to remove in one piece. That’s called piecemeal resection. It’s common with polyps over 20 mm. When this happens, the risk of leftover tissue increases. That’s why follow-up timing changes dramatically.The US guidelines say: come back in 6 months. That’s not a suggestion-it’s a rule. At that six-month check, the doctor looks for any remaining tissue or early signs of regrowth. If everything looks clean, you can go back to the standard schedule. But if there’s even a hint of leftover polyp, you might need another scope in another 3 to 6 months.
Some European guidelines suggest a range of 3 to 6 months, giving doctors flexibility. But in the U.S., sticking to the 6-month mark is the standard. Skipping it or waiting longer increases your risk of cancer developing undetected.

What About Serrated Polyposis Syndrome?
This is rare, but serious. If you have more than 20 serrated polyps total, with at least five being 10 mm or larger, you likely have serrated polyposis syndrome. This condition can lead to colon cancer before age 50.Guidelines vary. The Japanese recommend yearly colonoscopies. In the UK, doctors suggest every 1 to 2 years until age 75. But if you’ve had two clean scopes with no polyps over 10 mm, some doctors will stretch it to 2 years. The key? You can’t relax. This isn’t a routine check. It’s ongoing surveillance.
Why So Many Doctors Get It Wrong
Even though the guidelines are clear, most doctors still recommend the old 5-year rule. A 2020 study at a Veterans Affairs hospital found only 18.6% of gastroenterologists followed the updated 7-10 year interval for low-risk adenomas. Most stuck with 5 years out of habit-or fear.Why? Two reasons. First, many doctors don’t know the new rules. A 2022 survey found only 28.5% of U.S. gastroenterologists correctly identified the right interval for small serrated polyps. Second, there’s legal pressure. Doctors worry if they wait 10 years and a patient gets cancer, they’ll be blamed-even if the guidelines say it’s safe.
Patients get caught in the middle. Your primary care doctor might tell you to come back in 5 years. Your gastroenterologist says 10. Who do you believe? The answer is: check your pathology report. It tells you exactly what was found. Use that to ask the right questions.

Tools That Help You Stay on Track
You don’t have to remember all this. There are tools built into electronic health records now. Epic and Cerner systems can automatically flag your next colonoscopy date based on what was found. But not every clinic uses them.There’s also Polyp.app, a free tool developed by gastroenterologists at Massachusetts General Hospital. You input your polyp details-number, size, type-and it tells you your exact interval. It’s used by over 12,000 clinicians in the U.S. and is accurate for all guideline types.
Even better? Ask for a written summary after your procedure. It should say: “Recommended surveillance: X years.” If it doesn’t, ask for it. Don’t assume they’ll remember.
What If You’re Not Sure What You Had?
It’s common to get lost in the medical jargon. “Adenoma,” “SSL,” “hyperplastic”-it’s confusing. If you don’t know what you had, call your doctor’s office and ask for your pathology report. The report will list the exact type and size. You can also ask: “Was this a low-risk or high-risk polyp?”Here’s a simple cheat sheet:
- Low-risk: 1-2 adenomas ≤10 mm → 7-10 years
- Medium-risk: 3-4 adenomas <10 mm OR 1-2 SSLs <10 mm → 3-5 years
- High-risk: ≥10 mm adenoma, villous features, high-grade dysplasia, ≥5 polyps, or any SSL ≥10 mm → 3 years
- Piecemeal resection >20 mm: 6 months
- Serrated polyposis: 1-2 years
Keep this list. Put it in your phone. Show it to your doctor if they say something different.
What’s Next? Personalized Surveillance
The future isn’t about counting polyps anymore. Researchers are testing blood and stool tests that look for DNA changes linked to cancer risk. These molecular markers could one day tell you if you need a colonoscopy in 3 years-or if you can safely wait 10.Trials are already underway. One, NCT04567821, is testing a blood test that detects abnormal DNA methylation patterns. If it works, we might soon replace polyp counts with personalized risk scores.
Until then, stick to the rules. Your next colonoscopy isn’t a routine check-up. It’s a cancer prevention tool. Get the timing right, and you’re giving yourself the best shot at staying healthy.
How often do I need a colonoscopy after having one small adenoma removed?
If you had one or two adenomas smaller than 10 mm and no other high-risk features, you should wait 7 to 10 years for your next colonoscopy. This is based on the 2020 US Multi-Society Task Force guidelines, which show cancer risk is nearly the same as someone with a normal colon. Many doctors still recommend 5 years due to habit or fear, but the evidence supports waiting longer.
What if I had a serrated polyp instead of an adenoma?
For one or two sessile serrated lesions (SSLs) under 10 mm, the recommended interval is 5 to 10 years. If you had three or four, come back in 3 to 5 years. Five or more? Return in 3 years. SSLs are harder to detect and can turn cancerous without warning, so timing matters more than with adenomas. If your bowel prep was poor or the polyp was hard to remove, your doctor might shorten the interval.
Do I need a colonoscopy in 6 months if my polyp was removed in pieces?
Yes-if any polyp larger than 20 mm was removed in pieces, you need a follow-up colonoscopy in exactly 6 months. This is to check for leftover tissue that could grow into cancer. Waiting longer increases your risk. This rule applies regardless of polyp type. Don’t delay this appointment-it’s not optional.
Why do some doctors say 5 years when the guidelines say 7-10 years?
Many doctors still follow the old guidelines out of habit, fear of lawsuits, or lack of awareness. A 2022 survey found only 37% of U.S. gastroenterologists could correctly identify all risk categories. Even those who know the rules often over-call screenings to avoid missing something. Always ask for your pathology report and confirm your interval based on what was found-not what your doctor remembers.
Can I skip my next colonoscopy if I feel fine?
No. Colon cancer often grows without symptoms until it’s advanced. Polyps that become cancerous usually don’t cause pain, bleeding, or changes in bowel habits until it’s too late. Skipping your scheduled colonoscopy-even if you feel perfectly healthy-puts you at risk. The goal of surveillance is to catch problems before they become dangerous.
Are there alternatives to colonoscopy for follow-up?
For surveillance after polyp removal, colonoscopy is still the gold standard. Stool tests like FIT or Cologuard are for initial screening, not follow-up. If you’ve had polyps, those tests can’t confirm if new ones have grown. Only a colonoscopy lets your doctor see the entire colon and remove any new growths during the same visit. Don’t rely on stool tests for surveillance.
 Future Hepatitis C Treatments After Sofosbuvir: What's Next?
Future Hepatitis C Treatments After Sofosbuvir: What's Next?
 Effective Ways to Prevent Gonorrhea and Keep Your Partner Safe
Effective Ways to Prevent Gonorrhea and Keep Your Partner Safe
 What Is a Mentat? The Real‑World Meaning Behind Dune’s Human Computers
What Is a Mentat? The Real‑World Meaning Behind Dune’s Human Computers
 Coronary Calcium Score: What CT Scans Reveal About Plaque Buildup in Your Arteries
Coronary Calcium Score: What CT Scans Reveal About Plaque Buildup in Your Arteries
 Healthcare System Communication: How Institutional Education Programs Improve Patient Outcomes
Healthcare System Communication: How Institutional Education Programs Improve Patient Outcomes