When patients leave the doctor’s office confused, anxious, or unsure what to do next, it’s rarely because the diagnosis was wrong. More often, it’s because the communication broke down. Studies show that poor communication contributes to 80% of medical errors and is linked to 15-20% of adverse patient outcomes. That’s why hospitals and health systems are no longer treating communication as a soft skill - they’re building formal, structured education programs to fix it.
Why Communication Training Isn’t Optional Anymore
In 2010, the Affordable Care Act shifted healthcare’s focus from volume to value. Suddenly, hospitals weren’t just paid for how many procedures they did - they were paid based on how satisfied patients were. One of the biggest drivers of patient satisfaction? How well staff communicated. Data from Press Ganey in 2022 found a strong correlation (r=0.78) between communication quality and patient satisfaction scores. Hospitals with better-trained staff saw fewer malpractice claims - Johns Hopkins found a 30% drop among physicians who completed communication training. And it’s not just about being nice. Clear communication reduces readmissions, prevents medication errors, and helps patients follow treatment plans. The Joint Commission, which accredits U.S. hospitals, now requires formal communication processes under Standard RI.01.01.01. Medicare even ties 30% of hospital reimbursements to HCAHPS scores, which include questions like, “Did your doctors listen to you?” and “Did they explain things clearly?”What These Programs Actually Teach
These aren’t just lectures on “being polite.” Modern institutional programs are built on evidence, not guesswork. They focus on specific, measurable behaviors that make a difference. At the University of Maryland’s Program for Excellence in Patient-Centered Communication (PEP), clinicians learn to:- Elicit the patient’s story without interrupting
- Respond with empathy, not just facts
- Check for understanding using the “teach-back” method
- Setting boundaries with difficult patients
- Reading non-verbal cues
- Managing emotionally charged conversations
Specialized Programs for Different Roles
Not every clinician needs the same training. Programs are now tailored to specific roles. The Society for Healthcare Epidemiology of America (SHEA) offers a $75-$125 course for infection preventionists. It teaches them how to communicate about outbreaks, handle media inquiries, and correct misinformation on social media. One reviewer from Cleveland Clinic said Module 4 helped her reach 50,000 people with accurate vaccine info - turning a public health crisis into a teachable moment. Meanwhile, the University of Texas at Austin’s Health Communication Training Series (HCTS) focuses on public health emergencies. Their 2022 “Pandemic Preparedness” module was built after CDC reports showed 40% of early pandemic delays were due to poor internal communication. It teaches teams how to coordinate messaging during crises, something most hospitals had never practiced before.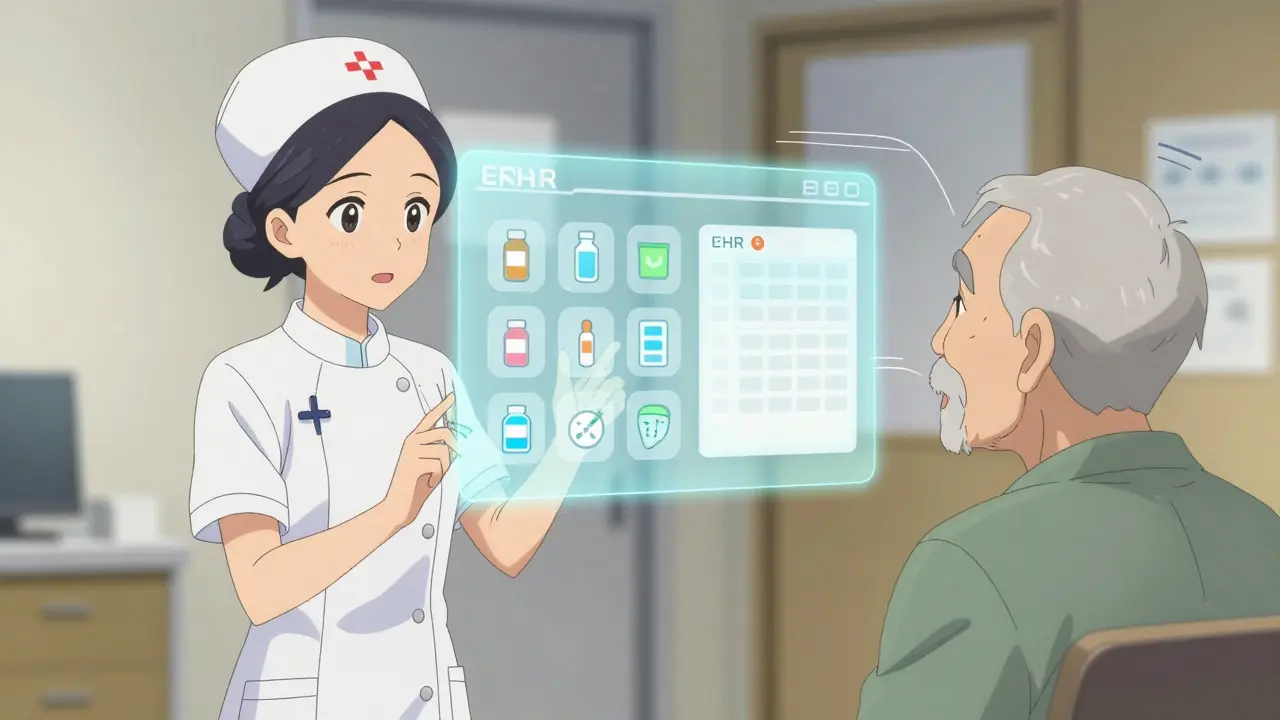
The Most Effective Method: Mastery Learning
Northwestern University’s simulation program uses a technique called mastery learning. Trainees don’t move on until they hit an 85% proficiency score on communication skills. They repeat simulations - 4 to 6 sessions over their clinical rotations - until they get it right. The results? A 37% higher skill retention rate after six months compared to traditional lecture-based training. Residents who completed the program also had 28% fewer patient complaints. But there’s a catch. It takes time, staff, and simulation labs. Only 22% of rural hospitals have the resources to do this. That’s why many institutions start small - training one unit at a time, using peer champions to lead the way.What’s Missing: Equity and Long-Term Tracking
Despite progress, major gaps remain. A 2023 AHRQ report found a 28% gap in communication satisfaction between white patients and minority patients. Yet only 40% of programs address cultural humility or health equity. And while most programs track satisfaction right after training, only 12% follow up beyond six months. Skills fade without reinforcement. Tulane’s 2022 study showed communication proficiency plateaued at 70% without ongoing practice. New tools are emerging. ACH is testing AI-powered feedback systems that analyze real clinician-patient conversations and give instant coaching. Early pilots show 22% faster skill acquisition. Some hospitals are embedding communication prompts directly into their EHR systems - reminding doctors to ask, “What’s your biggest concern today?” before they even open the chart.
How These Programs Are Changing Hospitals
Successful programs follow a four-phase model:- Needs assessment: Use patient surveys to find specific gaps - not “communication is bad,” but “staff don’t explain test results clearly.”
- Skills prioritization: Focus on 3-5 behaviors that will have the biggest impact.
- Contextualized training: Use real cases from your own hospital, not generic examples.
- Workflow integration: Add reminders to your EHR. Make communication part of the routine, not an extra task.
The Real Barrier Isn’t Training - It’s Time
Most clinicians agree: these skills matter. But 58% of healthcare workers surveyed in 2023 said they lack time to use them. Doctors interrupt patients after just 13.3 seconds - even after training. The solution isn’t more hours. It’s smarter design. One hospital reduced patient wait times by 20% simply by training staff to ask, “What’s your main concern?” at check-in - cutting down on later confusion and repeat questions.What’s Next?
The market for healthcare communication training hit $2.8 billion in 2023 and is growing at over 11% per year. Forty-seven universities now offer master’s degrees in health communication - up from 29 in 2019. The next wave will focus on:- Integrating communication tools into telehealth platforms
- Measuring skill retention using EHR data
- Building interprofessional training - where nurses, pharmacists, and doctors learn to communicate as a team
 Boost Your Health with Cat's Foot: The Ultimate Dietary Supplement You Need!
Boost Your Health with Cat's Foot: The Ultimate Dietary Supplement You Need!
 Exploring the Best Alternatives to Valtrex for Herpes Treatment
Exploring the Best Alternatives to Valtrex for Herpes Treatment
 How to Safely Buy Cheap Generic Azithromycin Online
How to Safely Buy Cheap Generic Azithromycin Online
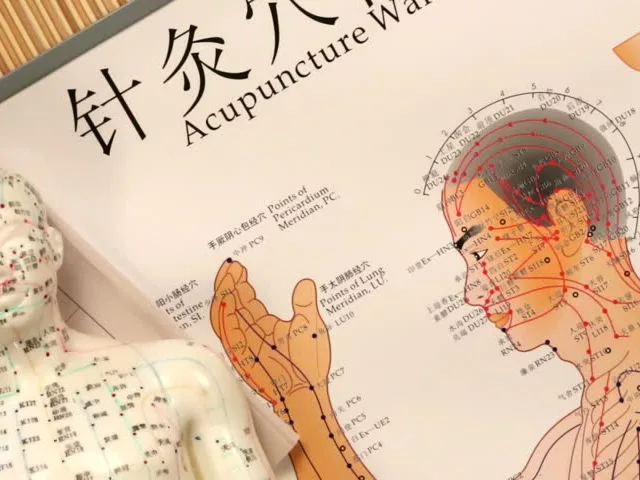 Inflammation of the Skin: The Benefits of Acupuncture and Traditional Chinese Medicine
Inflammation of the Skin: The Benefits of Acupuncture and Traditional Chinese Medicine
Roshan Gudhe
February 3, 2026 AT 13:55Communication in healthcare isn't just about talking-it's about listening with your whole being. I've seen doctors recite textbook answers while patients cried silently. Training that teaches empathy, not just scripts, is the only thing that can heal the real wound: disconnection.
Wendy Lamb
February 4, 2026 AT 07:39Teach-back works. My mom didn’t understand her diabetes meds until her nurse asked her to explain it back. Simple. No jargon. Just clarity.
caroline hernandez
February 5, 2026 AT 15:22There's a critical gap in longitudinal competency tracking. Without sustained reinforcement via EHR-integrated nudges and periodic OSCE-style re-assessments, even the most robust training regimens devolve into performative compliance. Skill decay is inevitable without deliberate practice cycles embedded into workflow architecture.
Prajwal Manjunath Shanthappa
February 7, 2026 AT 02:44Let’s be honest: this is just corporate fluff dressed up as ‘evidence-based.’ Real medicine is about efficiency, not emotional labor. If your patient can’t understand ‘take two pills daily,’ maybe they shouldn’t be trusted with their own health.
Janice Williams
February 7, 2026 AT 04:35How convenient that after decades of underfunding hospitals, we suddenly care about communication. This is a PR move to deflect from the real crisis: staffing shortages, 12-minute visits, and insurance denials. Training doctors to smile more doesn’t fix a system built to extract profit, not care.
And don’t get me started on ‘cultural humility’-it’s a buzzword for guilt-tripping white clinicians while ignoring systemic racism in diagnostics and access.
Also, 28% gap in satisfaction? That’s not communication-it’s structural neglect. You can’t train empathy into a machine that’s designed to grind people down.
And who funds this? Hospitals? Medicare? The same entities that cut nursing staff by 20% last year? Please.
I’ve seen the ‘champions’-they’re the ones working 80-hour weeks while training others. They’re not heroes. They’re exhausted.
And AI feedback systems? That’s just surveillance with a smiley face. Who’s auditing the algorithm? Is it trained on biased datasets? Of course it is.
Stop pretending this is about patients. It’s about HCAHPS scores and avoiding fines.
And the $2.8 billion market? That’s a gold rush. Consultants, universities, and tech startups are cashing in while nurses quit by the thousands.
Let’s fund more beds. More nurses. More time. Not another PowerPoint on ‘active listening.’
And if you think this solves equity, you haven’t met a single Black patient who’s been dismissed for ‘being emotional’ while their heart attack went untreated.
Training doesn’t fix oppression. It masks it.
Alex LaVey
February 8, 2026 AT 22:28I’ve worked in rural clinics for 15 years. We don’t have simulation labs. We don’t have budgets. But we do have trust. I sit with my patients. I learn their names. I ask about their grandkids. That’s the communication training that matters.
Not the fancy courses. Not the AI. Just presence.
And yes-I interrupt sometimes. But I also listen longer than most. Because I know if I don’t, no one else will.
Jhoantan Moreira
February 10, 2026 AT 16:54Love how this highlights interprofessional training. My pharmacist and I now do weekly huddles before rounds. We catch med errors before they happen. It’s not about hierarchy-it’s about teamwork. 🙌
Caleb Sutton
February 12, 2026 AT 12:19They’re using AI to monitor doctors? Who’s watching the AI? This is Big Pharma’s new control system. They’re not training communication-they’re training obedience. You think they care about patients? They care about liability. Every word you say is being recorded, analyzed, and weaponized. Next thing you know, you’re flagged for ‘negative sentiment’ because you said ‘I’m sorry this is taking so long.’
Antwonette Robinson
February 13, 2026 AT 08:09Wow. So after 30 years of ignoring patient feedback, we’re suddenly shocked that people are confused? Maybe if you’d listened before, we wouldn’t need a $2.8 billion industry to teach you how to speak English.
Kunal Kaushik
February 15, 2026 AT 04:53My aunt had a stroke. The nurse didn’t explain the meds. She just handed her a paper. She took the wrong dose. Ended up back in ER. Simple stuff. But nobody had time. Training won’t fix that unless you fix the schedule.
Also, emoji for empathy? 🤔
Daz Leonheart
February 15, 2026 AT 18:51my brother is a nurse and he said the teach-back thing actually works but only if the doc stops rushing. the system is broken. training is just bandaids. we need less patients per shift. not more slides.
Rachel Kipps
February 17, 2026 AT 05:38I’m a patient advocate. I’ve sat in on dozens of discharge meetings. The most common mistake? Assuming understanding. Not asking. Not checking. Not pausing. It’s not about being nice. It’s about being responsible.
And I’ve seen families cry because they didn’t know what to do next. No one told them. No one asked.
Simple. Human. Necessary.
Ed Mackey
February 18, 2026 AT 11:33One thing no one talks about: burnout. Nurses aren’t robots. If you’re exhausted, you’re not going to remember the teach-back script. You’re going to say ‘just follow the paper.’ Training has to include mental health support, not just communication modules.
And typo: I meant ‘you’re’ not ‘your’-but you get the point.