Drug Interaction Checker
Check Your Medications
Enter all medications you're currently taking. Include prescriptions, OTC drugs, supplements, and vitamins.
No medications added yet. Start by adding your current medications above.
Every year in the U.S., thousands of people end up in the hospital-not because of a fall, infection, or accident-but because they took two medications together that shouldn’t have been mixed. It’s not rare. It’s not exotic. It’s drug interactions, and they’re often completely preventable. You might be taking a blood pressure pill, a painkiller, a vitamin, and a sleep aid, all prescribed by different doctors. None of them are dangerous alone. But together? They could cause a dangerous drop in blood pressure, liver damage, or even a heart rhythm problem. The good news? You don’t need to be a doctor to protect yourself. You just need to know what to check and how to ask the right questions.
Know Exactly What You’re Taking
Before you even think about a new medication, make a complete list of everything you’re already taking. Not just prescriptions. Not just the big-name drugs. Everything. That includes:- Prescription medications (name, dose, how often)
- Over-the-counter pills (ibuprofen, antacids, allergy meds)
- Vitamins and minerals (especially iron, calcium, vitamin K)
- Herbal supplements (St. John’s wort, garlic, ginkgo, echinacea)
- Probiotics, amino acids, and energy drinks with hidden stimulants
Many people forget supplements. But St. John’s wort can make birth control fail. Garlic can thin your blood too much if you’re on warfarin. Even a simple vitamin D pill can interfere with some thyroid medications. Write down the exact brand and dosage. Don’t rely on memory. Bring the actual bottles to your next appointment. A 2018 study found that patients who brought their physical meds to their doctor cut medication errors by 37%.
Ask These Four Questions Before Accepting a New Prescription
Don’t assume your doctor knows your full list. Even if you filled out a form, they might not have seen it. Don’t wait for them to ask. Ask them yourself. Here are the exact questions to say:- Can I take this with my other medications?
- Should I avoid any foods, drinks, or alcohol while taking this?
- What signs of a bad reaction should I watch for?
- How will this drug work in my body, and could it affect anything else I’m taking?
These aren’t just polite questions-they’re safety checks. For example, if you’re on simvastatin (Zocor) for cholesterol and your doctor prescribes amiodarone for heart rhythm, combining them at high doses can raise your risk of muscle breakdown by 15 times. That’s not theoretical. It’s been documented in multiple studies. But if you ask, your doctor might switch you to a safer statin like pravastatin.
Use a Reliable Drug Interaction Checker-But Don’t Trust It Fully
There are free tools online that can help you scan your meds. The best ones include:- Drugs.com Drug Interactions Checker-covers over 24,000 prescription drugs, 7,000 supplements, and 4,000 foods. It’s updated daily and used by over a million people monthly.
- University of Liverpool HIV Drug Interaction Checker-originally built for HIV meds, but now covers dozens of common drugs. It uses a color-coded system (red = avoid, yellow = caution, green = safe) and rates evidence strength from 1 (strong) to 5 (theoretical).
- WebMD Drug Interaction Checker-easy to use, but less accurate than Drugs.com in clinical studies.
A 2021 study in the Journal of Medical Internet Research found Drugs.com caught 92.4% of serious interactions. WebMD caught 87.1%. That might sound good-but here’s the catch: no tool knows your body. It doesn’t know if you have kidney disease, are over 65, or have a genetic variation that slows how you process drugs. The FDA says these tools are helpful, but they’re not a substitute for professional advice. Use them to spot red flags, then bring those flags to your doctor or pharmacist.
Know the Most Dangerous Combinations
Some drug pairs are so risky they show up in hospital data over and over. Here are the top seven combinations linked to serious hospitalizations, according to the American Academy of Family Physicians:- Warfarin + NSAIDs (like ibuprofen or naproxen): Increases bleeding risk. Even a minor cut can become life-threatening.
- SSRIs + MAOIs (certain antidepressants): Can cause serotonin syndrome-a dangerous spike in body temperature, confusion, and muscle rigidity.
- Digoxin + Clarithromycin (an antibiotic): Can cause digoxin to build up to toxic levels, leading to irregular heartbeat.
- Statins + Fibrates (cholesterol drugs): Raises risk of rhabdomyolysis-muscle tissue breaking down and damaging kidneys.
- Calcium channel blockers + Protease inhibitors (HIV meds): Can cause dangerously low blood pressure.
- Sildenafil (Viagra) + Nitrates (heart meds): Can crash blood pressure to fatal levels.
- Theophylline + Fluvoxamine (asthma + antidepressant): Can cause seizures or heart rhythm problems.
If you’re on any of these drugs, make sure your new prescription doesn’t clash. Even if your doctor says it’s fine, double-check. One Reddit user reported that their pharmacist caught a major interaction between sertraline and linezolid that their doctor had missed-saving them from a life-threatening serotonin surge.
Use One Pharmacy for Everything
If you fill prescriptions at CVS, Walgreens, and a local pharmacy, each one only sees part of your picture. That’s how dangerous combinations slip through. A 2021 study of 22,000 Medicare patients found that using just one pharmacy reduced serious drug interactions by 31%. Why? Because one pharmacy has one full record. They can scan every new prescription against every old one, every supplement, every OTC pill.Some people switch pharmacies to save money. But if you’re taking five or more meds, the cost of a bad interaction-hospital stay, ER visit, long-term damage-is far higher than a few dollars on a prescription. The BeMedWise Program calls this the “One Pharmacy Rule.” It’s simple. Stick with one. Let them become your safety net.
Update Your Medication List After Every Visit
Your meds change. A lot. A new antibiotic. A steroid for inflammation. A new painkiller after surgery. Don’t wait until your annual checkup. After every doctor’s visit, update your list. Keep it in your wallet, phone notes, or a printed copy you carry. The Cleveland Clinic calls this a “medication passport.” In their program, patients who kept updated lists saw a 52% drop in medication errors.Even small changes matter. If your doctor says, “Take one pill a day instead of two,” write it down. If you stop a supplement because you felt weird, note that too. You might forget later. But your pharmacist won’t-if they have the full picture.
Watch for Warning Signs
Not every interaction causes immediate symptoms. But some do. If you start a new drug and notice any of these, call your doctor or go to urgent care:- Unexplained bruising or bleeding
- Severe dizziness, fainting, or fast heartbeat
- Unusual muscle pain, weakness, or dark urine
- Extreme fatigue, confusion, or memory loss
- Severe stomach pain, nausea, or yellowing skin/eyes
- Rash, swelling, or trouble breathing
These aren’t “maybe it’s nothing” symptoms. They’re red flags. A study from 1995 showed that half of all adverse drug reactions are preventable-if you catch them early. Don’t wait. Don’t assume it’s just a side effect. Ask: “Could this be from a drug interaction?”

Don’t Assume Supplements Are Safe
Many people think “natural” means “safe.” It doesn’t. St. John’s wort can make birth control, antidepressants, and even some cancer drugs stop working. Garlic and ginkgo can thin your blood. Kava can damage your liver. Turmeric can interfere with blood thinners. A 2023 survey found that 58% of patients never tell their doctor about supplements they take. That’s a gap in your safety net. Always disclose them. Even if you think they’re “just vitamins.”Technology Is Helping-But You’re Still the Last Line of Defense
Hospitals and pharmacies are using smarter systems. The FDA is testing AI tools that predict your personal risk based on your age, kidney function, and genetics. The NIH has shown that adding your CYP450 gene data (which tells how you metabolize drugs) improves accuracy by 37%. But these tools aren’t everywhere yet. And even when they are, they can’t replace your awareness.Here’s the hard truth: 8.3% of prescriptions in U.S. pharmacies are still filled for known dangerous combinations. Why? Because patients use multiple pharmacies. Because doctors are rushed. Because patients don’t speak up. You can’t control the system. But you can control your own checklist. Your list. Your questions. Your pharmacy. Your vigilance.
Drug interactions aren’t scary because they’re common. They’re scary because they’re preventable. And you’re the one who holds the key.
Can I use a drug interaction checker app instead of talking to my doctor?
No. Apps like Drugs.com or WebMD are useful tools to spot potential problems, but they don’t know your full health picture-like your kidney function, age, genetics, or other conditions. They also can’t interpret subtle risks or adjust for your unique situation. Always confirm any warning with your doctor or pharmacist. The FDA warns that patient-facing tools should never replace professional advice.
What should I do if I accidentally took two drugs that interact?
Don’t panic, but don’t wait. Call your pharmacist or doctor right away. If you’re having symptoms like dizziness, chest pain, confusion, muscle weakness, or trouble breathing, go to the nearest emergency room. Even if you feel fine, it’s important to get checked. Some interactions take hours or days to show effects. Your provider may advise you to stop one drug, adjust the dose, or monitor you closely.
Why do I get so many interaction alerts when I use a pharmacy app?
Pharmacy systems often flag every possible interaction-even ones with very low risk or no real-world evidence. This is called “alert fatigue.” Too many warnings mean people start ignoring them, even the important ones. A Reddit user reported 12 false alerts for just five common meds. That’s why the American Medical Informatics Association recommends systems use only high-evidence alerts (Level A or B). If you’re overwhelmed, ask your pharmacist to explain which alerts matter and which don’t.
Are herbal supplements really dangerous with prescription drugs?
Yes. Many people assume supplements are harmless because they’re “natural.” But St. John’s wort can make birth control, antidepressants, and transplant drugs stop working. Garlic and ginkgo can thin your blood dangerously if you’re on warfarin. Kava can cause liver damage, especially with alcohol or acetaminophen. A 2023 survey found 58% of patients never tell their doctor about supplements. That’s a huge risk. Always list them-exactly what you take and how often.
Is it safe to take my meds with grapefruit juice?
No-not if you’re taking certain drugs. Grapefruit juice blocks an enzyme in your gut that breaks down some medications, causing them to build up to toxic levels. This affects statins (like simvastatin and atorvastatin), some blood pressure meds (like felodipine), and certain anti-anxiety drugs. Even one glass can cause problems that last over 24 hours. The American Heart Association specifically warns against it with statins. If you’re unsure, ask your pharmacist whether your meds interact with grapefruit.
How often should I review my medication list?
At least once a year-but ideally after every doctor’s visit, hospital stay, or new prescription. Medications change often. A new painkiller, a short-term antibiotic, or a seasonal allergy med can all create new risks. The BeMedWise Program recommends bringing all your pill bottles to one annual review. But if you’re on five or more drugs, or have multiple chronic conditions, review your list every 3-6 months. Keep it updated. It’s your best defense.
Next Steps: Your Action Plan
1. Make your list. Write down every medication, supplement, and OTC pill you take. Include doses and frequency.2. Use Drugs.com. Enter your full list and see what pops up. Note any red flags.
3. Go to one pharmacy. If you use multiple, switch to one. Ask them to run a full interaction scan.
4. Ask the four questions. Before accepting any new prescription, ask your doctor: Can I take this with my other meds? Should I avoid food or drinks? What signs should I watch for? How will this affect my body?
5. Update after every visit. Add or remove meds immediately. Keep the list in your wallet or phone.
6. Speak up. If something feels off after starting a new drug-don’t wait. Call your provider. You know your body best.
Drug interactions don’t care how smart you are. They don’t care if you’re healthy or old. They only care if you’re unaware. Stay informed. Stay vigilant. Your life depends on it.

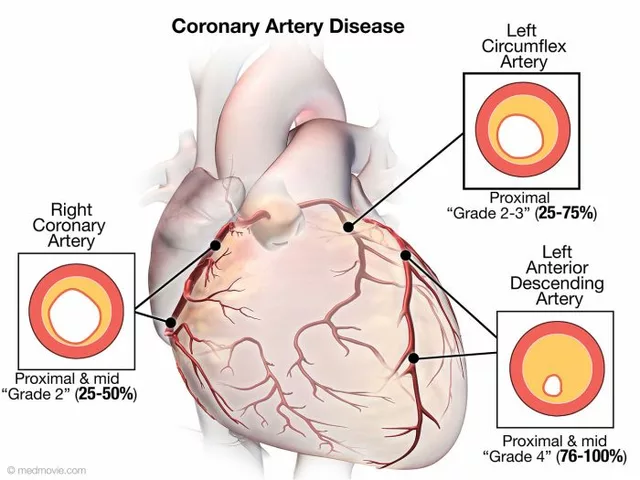 Coronary Artery Disease and Mental Health: The Impact on Emotional Well-being
Coronary Artery Disease and Mental Health: The Impact on Emotional Well-being
 Feverfew and Anticoagulants: What You Need to Know About Bleeding Risk
Feverfew and Anticoagulants: What You Need to Know About Bleeding Risk
 Epivir (Lamivudine) vs Other HIV Drugs: Detailed Comparison
Epivir (Lamivudine) vs Other HIV Drugs: Detailed Comparison
 How Medicines Work and When They’re Safe to Use
How Medicines Work and When They’re Safe to Use
 Hemophilia Self‑Care Guide: How to Take Time for Yourself
Hemophilia Self‑Care Guide: How to Take Time for Yourself
Jamie Watts
November 15, 2025 AT 08:11Yo I've seen this so many times in the ER - people think 'natural' means 'safe' and then show up with liver failure from St. John's wort and warfarin. No one tells their doctor about supplements. I had a guy last week who took turmeric for 'inflammation' and bled out from a nosebleed. You're not a wizard. You're not a chef. You're a patient. Listen to the science.
John Mwalwala
November 16, 2025 AT 10:48They don't want you to know this but the FDA and Big Pharma are actively suppressing the truth about drug interactions because they make more money off you getting sick. The real danger? The CYP450 enzyme system is being manipulated by glyphosate in your food and EMF radiation from your phone. That's why the interaction checkers are useless. They don't account for the 5G-induced metabolic chaos. Your pharmacist? Probably on the payroll. I've been tracking this since 2017. The data is buried in PubMed but you need to know how to dig. Trust no one. Check your bloodwork. Always.
Deepak Mishra
November 17, 2025 AT 17:09OMG I JUST HAD THIS HAPPEN TO ME!!! 😱 I took ibuprofen with my blood thinner and my hand started swelling and I thought I was gonna DIE!!! 💔 I called my pharmacist at 2am and she was like 'oh honey you're lucky you didn't stroke out' 😭😭😭 I'm switching to one pharmacy now and I'm writing EVERYTHING down!! 📝💖 I even made a color coded chart!!! 🎨🌈 #MedSafety #DontBeLikeMe
Diane Tomaszewski
November 19, 2025 AT 05:49It's funny how we treat our bodies like machines you just plug stuff into. We don't ask how the parts talk to each other. We just assume it'll work. But we're not robots. We're messy, biological, weird things. Maybe the real solution isn't more apps or checklists. Maybe it's just slowing down. Listening. Not rushing to the next pill.
Dan Angles
November 20, 2025 AT 11:11While the article presents a commendable framework for mitigating medication-related risks, it is imperative to underscore the non-negotiable role of clinical pharmacists in the medication reconciliation process. The 'One Pharmacy Rule' is not merely a suggestion-it is a standard of care endorsed by the American Society of Health-System Pharmacists. Furthermore, the integration of electronic health records with clinical decision support systems remains underutilized in outpatient settings. I urge all patients to request a formal medication therapy management session with a certified pharmacist at least biannually.
David Rooksby
November 20, 2025 AT 16:49Look I get it, you're all about the checklist and the apps and the one pharmacy thing, but let's be real here - doctors are overworked, pharmacists are underpaid, and the system is rigged. I had a guy at my local CVS give me a 12-page printout of 'possible interactions' for my 5 meds - half of them were for things that only happen if you're on 17 drugs and have a liver transplant. That's alert fatigue, man. It's not helping, it's making people tune out. I once had a pharmacist yell at me because I took melatonin with my antidepressant - turns out it was fine, just a dumb algorithm flagging it because someone in Sweden once reported a headache. We need smarter systems, not more noise. And stop acting like everyone's just lazy for not writing everything down - I work two jobs and sleep 4 hours a night. You want me to be perfect? Then fix the damn system first.
Melanie Taylor
November 22, 2025 AT 10:36As a South Asian immigrant, I can’t tell you how many times my parents took 'herbal teas' from the market and didn’t tell anyone - 'it’s just for digestion!' 🙈 But then they ended up in the hospital because it mixed with their blood pressure meds. I started translating all their pill bottles into Hindi and making them show me every bottle before they take anything. Now they laugh about it - but they do it. 🌿❤️ If you’re from a culture where 'natural' = 'no doctor needed' - please, please, please talk to someone. We’re not alone in this.
Teresa Smith
November 23, 2025 AT 08:13Let me be clear - this isn't about being careful. It's about being responsible. You don't get to be a passive participant in your own health. If you're on five or more medications, you owe it to yourself - and your family - to be the CEO of your pharmacology. This isn't a suggestion. It's a survival protocol. And if you're too tired, too busy, or too overwhelmed to make a list, then you're not too busy - you're just in denial. Your life isn't a suggestion box. It's your only one. Update your list. Call your pharmacist. Say the four questions. Do it now. Not tomorrow. Today.
ZAK SCHADER
November 23, 2025 AT 09:24Why are we even doing this? In America we got the best doctors, the best tech, and we're still getting screwed by our own laziness? We got apps for everything but we still forget to tell our doctor we took a gummy vitamin? This ain't rocket science. It's basic. We got free apps, free pharmacies, free info - and people still get hospitalized because they didn't write down a pill name? We're not sick from drugs. We're sick from stupidity. Fix your brain first.
Danish dan iwan Adventure
November 24, 2025 AT 02:17Drug interaction risk stratification requires CYP450 genotyping + polypharmacy index + renal clearance metrics. Apps are heuristic. Clinically insufficient. Your pharmacist's system is rule-based. Still inadequate. Only AI-driven pharmacokinetic modeling with real-time EHR integration can reduce iatrogenic harm at scale. Prioritize genomic testing if on >3 meds. Otherwise, you're gambling with your cytochrome P450 isoforms.