When you pick up a prescription at the pharmacy and see a generic version of your brand-name drug, you’re seeing the result of a highly structured, science-driven process managed by the FDA. It’s not just about copying a pill. The FDA’s approval of generic drugs follows a strict, legally defined pathway called the Abbreviated New Drug Application (ANDA). This system was created by the Hatch-Waxman Act of 1984 to make safe, effective, and affordable medicines available to millions - without forcing companies to repeat every clinical trial ever done on the original drug.
What Is an ANDA, and Why Does It Exist?
An ANDA is a regulatory submission to the FDA that proves a generic drug is the same as its brand-name counterpart in every way that matters: active ingredient, strength, dosage form, route of administration, and, most critically, how your body absorbs it. The word “abbreviated” isn’t a shortcut - it’s a smart reuse of existing data. The brand-name drug already went through years of safety and efficacy testing. The generic doesn’t need to redo that. Instead, it must prove it performs the same way in your body. The FDA’s Center for Drug Evaluation and Research (CDER), through its Office of Generic Drugs (OGD), handles every ANDA. Since 2015, the FDA has approved over 450 first-time generic drugs. In 2023 alone, 90 new generics hit the market. That’s not random - it’s the result of a system designed to scale competition.The Five Core Requirements for Generic Approval
For a generic drug to get approved, it must meet five non-negotiable standards:- Pharmaceutical equivalence: The generic must have the exact same active ingredient, strength, dosage form (pill, injection, cream), and route of administration (oral, topical, etc.) as the brand-name drug, known as the Reference Listed Drug (RLD).
- Bioequivalence: This is the heart of the process. The generic must deliver the same amount of active ingredient into your bloodstream at the same rate as the brand. The FDA requires studies with 24 to 36 healthy volunteers, measuring blood levels over time. The results must fall within 80% to 125% of the brand’s values - a tight window that ensures no clinically meaningful difference.
- Manufacturing quality: The facility making the generic must follow Current Good Manufacturing Practices (cGMP). This means clean rooms, validated equipment, strict quality control, and documented processes. The FDA inspects these sites - sometimes unannounced - and will reject an ANDA if the facility fails.
- Labeling accuracy: The generic’s label must match the brand’s in content and format, except for minor differences in inactive ingredients (like dyes or fillers). Even those must be safe and properly listed.
- Electronic submission format: All ANDAs must be submitted in the eCTD (electronic Common Technical Document) format. This isn’t just a preference - it’s a rule. The dossier is split into five modules covering administrative info, summaries, quality data, nonclinical studies, and clinical data (labeling).
The ANDA Submission Process: What Happens After You File
Once a company submits an ANDA, the clock starts. Under the Generic Drug User Fee Amendments (GDUFA), the FDA has a target of reviewing complete applications within 10 months. But the journey doesn’t begin with a review - it begins with a filing decision. Within 60 days of submission, the FDA decides whether the ANDA is filed or refused. If it’s refused, it’s usually because of missing documents, formatting errors, or incomplete data. Companies get one chance to fix it. If they don’t, the application is abandoned. If filed, the application enters the review queue. The review team - made up of chemists, pharmacologists, microbiologists, and regulatory specialists - digs into every page. They check:- Is the bioequivalence study statistically sound?
- Does the manufacturing process consistently produce the same product batch after batch?
- Are the inactive ingredients safe and properly documented?
- Is the labeling clear, accurate, and identical to the RLD?
Why Some Generic Drugs Take Longer Than Others
Not all generics are created equal. Simple oral tablets - like metformin or lisinopril - are straightforward. Their ANDAs often clear review in 10 to 11 months. But complex products? That’s a different story. Inhalers, nasal sprays, injectable suspensions, and topical ointments are harder to copy. Why? Because their effectiveness depends not just on the drug, but on how it’s delivered. The particle size in an inhaler, the viscosity of a cream, the stability of a suspension - these are harder to replicate. The FDA calls these “complex generic drugs.” About 15% of ANDAs fall into this category. One company submitted an ANDA for a nasal spray in 2022. It received three CRLs over 28 months. Each time, the FDA questioned the bioequivalence methodology. The company spent over $2.3 million in extra testing. That’s not rare. For complex products, the review timeline can stretch to 3 years or more.
Patents, Exclusivity, and Legal Hurdles
Even if your ANDA is perfect, you might not be able to sell your drug right away. The brand-name drug might still be under patent protection. Or it might have data exclusivity - a period during which the FDA can’t approve a generic, even if the patent has expired. The Hatch-Waxman Act lets generic companies challenge patents by filing a Paragraph IV certification. This means they claim the patent is invalid or won’t be infringed. If they win in court, they get 180 days of market exclusivity - the first generic on the market gets to be the only one selling for half a year. That’s why companies like Teva and Mylan spend millions on legal teams. In 2023, the first generic version of Humira made over $1.2 billion during its exclusivity window. But if multiple companies file Paragraph IV certifications at the same time, they share the 180-day window. That’s why you sometimes see several generics launch on the same day.Who’s Winning the Generic Game?
The U.S. generic drug market is crowded. Over 100 companies compete, but a few dominate:- Teva Pharmaceutical: 15.2% market share
- Viatris (formerly Mylan): 12.7% share
- Sandoz: 10.3% share
How Long Does It Really Take to Get a Generic Approved?
The timeline isn’t just about FDA review. The whole process takes years:- 6-9 months: Design and run the bioequivalence study
- 3-6 months: Develop the formulation and manufacturing process
- 2-4 months: Compile the eCTD dossier
- 10 months: FDA review (target under GDUFA)
What Happens After Approval?
Approval doesn’t mean the job is done. The FDA continues to monitor:- Post-market adverse event reports
- Manufacturing inspections (every 2-3 years)
- Batch testing for consistency
Are Generic Drugs Really the Same?
The short answer: yes - for 99% of patients. The FDA requires generics to meet the same standards as brand-name drugs. Studies show that generic drugs perform just as well in clinical practice. For most conditions - diabetes, high blood pressure, cholesterol - switching to a generic makes no difference. But there are exceptions. For drugs with a narrow therapeutic index (NTI), like warfarin, levothyroxine, or phenytoin, even small differences in absorption can matter. Some patients report feeling different after switching. The FDA acknowledges this and recommends close monitoring in these cases. But that doesn’t mean the generic is unsafe - it means the system requires extra caution. As Dr. Janet Woodcock, former head of CDER, said: “Generic drugs account for 90% of prescriptions filled in the U.S. but only 23% of total drug spending.” That’s the power of the ANDA system.What’s Next for Generic Drug Approval?
The FDA is making changes to keep up with demand and complexity:- GDUFA IV (2023-2027): Aims to review 90% of ANDAs within 10 months and reduce median review time to 8 months.
- Complex Generic Drug Initiative: New guidance for 27 types of complex products - from inhalers to topical gels.
- AI in review: The FDA is testing AI tools to sort through documents faster, cutting administrative time by 25% by 2025.
- Biosimilars: The same logic is being applied to biologic drugs. The FDA expects to approve 10-15 biosimilars a year by 2026.
How long does the FDA take to approve a generic drug?
Under the current GDUFA guidelines, the FDA targets a 10-month review timeline for complete ANDA submissions. However, the entire process - from formulation development to final approval - typically takes 3 to 4 years. This includes time for bioequivalence studies, manufacturing setup, and regulatory preparation before the application is even filed. If the FDA issues a Complete Response Letter (CRL), the timeline can extend further depending on how quickly the company addresses the issues.
Can a generic drug be different from the brand-name version?
Legally and scientifically, a generic drug must be identical to the brand-name drug in active ingredient, strength, dosage form, and route of administration. It must also be bioequivalent - meaning it delivers the same amount of drug into your bloodstream at the same rate. Differences are only allowed in inactive ingredients (like colorants or fillers), and those must still be safe. While most generics work the same, a small number of patients may notice differences with narrow therapeutic index drugs like warfarin or levothyroxine, where even minor absorption changes can matter.
Why do some generic drugs get rejected by the FDA?
The most common reasons for rejection include incomplete or flawed chemistry, manufacturing, and controls (CMC) data (32% of cases), inadequate bioequivalence study design (28%), manufacturing facility issues (22%), and labeling discrepancies (18%). Many rejections happen because companies underestimate the level of detail required in the eCTD submission. Even small formatting errors or missing stability data can trigger a Complete Response Letter.
Are generic drugs made in the same facilities as brand-name drugs?
Yes - and no. Many generic drugs are made in the same factories as brand-name drugs, especially when the original manufacturer also produces the generic. But most generics are made in separate facilities, often overseas. The FDA inspects all manufacturing sites - whether in the U.S., India, China, or elsewhere - using the same cGMP standards. A facility that makes a brand-name drug must meet the same quality rules as one making a generic. The FDA doesn’t distinguish between them in its inspections.
How does the FDA ensure generic drugs are safe after they’re on the market?
The FDA continues to monitor generics after approval through post-market surveillance. This includes tracking adverse event reports, conducting random facility inspections every 2-3 years, and testing drug batches for consistency and purity. If a generic drug is linked to safety issues - such as contamination or inconsistent absorption - the FDA can issue recalls or require changes to the manufacturing process. For example, in 2021, the FDA recalled several generic blood pressure medications due to impurities, showing that oversight doesn’t end at approval.
 Diarex vs Alternatives: Which Hair Loss Treatment Performs Best?
Diarex vs Alternatives: Which Hair Loss Treatment Performs Best?
 Medicare Drug Coverage and Cost Assistance Options in 2025-2026
Medicare Drug Coverage and Cost Assistance Options in 2025-2026
 Buy Cheap Generic Abilify Online: A Practical Guide
Buy Cheap Generic Abilify Online: A Practical Guide
 Rheumatoid Arthritis: Understanding Autoimmune Joint Damage and Modern Biologic Treatments
Rheumatoid Arthritis: Understanding Autoimmune Joint Damage and Modern Biologic Treatments
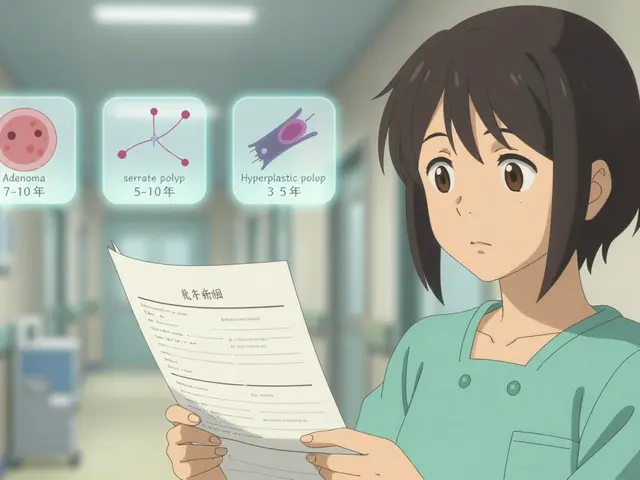 Repeat Colonoscopy: What Your Surveillance Interval Should Be After Polyp Removal
Repeat Colonoscopy: What Your Surveillance Interval Should Be After Polyp Removal
Steve World Shopping
December 3, 2025 AT 07:59The ANDA framework is a masterclass in regulatory efficiency-pharmaceutical equivalence, bioequivalence thresholds (80-125%), cGMP compliance, eCTD formatting-all meticulously engineered to eliminate redundant clinical trials while preserving therapeutic integrity. The real genius lies in the FDA’s refusal to compromise on bioequivalence metrics, even as global manufacturing complexity skyrockets. This isn’t bureaucracy-it’s pharmacokinetic precision.
Alicia Marks
December 3, 2025 AT 19:46This is why generics save lives. 💙
Paul Keller
December 4, 2025 AT 18:34It is imperative to recognize that the Abbreviated New Drug Application process, while ostensibly streamlined, remains an extraordinarily rigorous and methodologically stringent regulatory pathway. The FDA’s Office of Generic Drugs operates under a framework that prioritizes patient safety above commercial expediency, which is why even minor deviations in dissolution profiles or excipient composition can trigger a Complete Response Letter. The 10-month review window is not a target-it is a benchmark of scientific discipline. To suggest otherwise is to misunderstand the foundational principles of pharmacovigilance and evidence-based medicine.
Jay Everett
December 5, 2025 AT 08:01Bro. The ANDA system is basically the superhero of healthcare economics. 🦸♂️💊
Brand drug costs $400? Generic hits $4. Same active ingredient. Same blood levels. Same results. Just without the fancy packaging and $300M marketing budget.
And the FDA? They’re the no-nonsense bouncer checking IDs at the club-bioequivalence? Check. cGMP? Check. Labeling? Double-check.
Complex generics like inhalers? Yeah, those are like trying to copy a jet engine with a 3D printer-takes forever, costs a fortune, and someone’s always crying about particle size.
But when it works? It’s pure magic. Millions of diabetics on $3 metformin. Grandmas on $2 lisinopril. That’s the ANDA dream. No hype. Just science that works.
मनोज कुमार
December 5, 2025 AT 23:42Joel Deang
December 6, 2025 AT 02:28so like… the FDA checks if the generic pill dissolves the same way as the brand one? like… literally just watches it melt in a beaker? 🤯
also why do all the generic factories seem to be in india? is that why my blood pressure med tastes weird now?? 😅
Arun kumar
December 6, 2025 AT 16:07it’s funny how people think generics are ‘inferior’ but the same exact science that makes the brand work is used for the generic. the body doesn’t care if the pill says ‘Pfizer’ or ‘teva’-it only cares about the molecule. the real issue is marketing, not medicine. we’ve been conditioned to trust logos over labs.
Zed theMartian
December 8, 2025 AT 00:47Let me be the first to say this: the entire ANDA system is a corporate illusion. The FDA isn’t protecting patients-they’re protecting Big Pharma’s monopoly by delaying generics through bureaucratic red tape. That ‘10-month review’? A joke. Look at the 28-month nightmare for that nasal spray. That’s not science-that’s a pay-to-play system where only giants like Teva and Sandoz can afford the legal and regulatory war chest. And don’t get me started on Paragraph IV certifications-this isn’t innovation, it’s litigation theater dressed up as public health.
ATUL BHARDWAJ
December 9, 2025 AT 07:45Rebecca M.
December 10, 2025 AT 20:50Oh wow, so the FDA just says ‘sure, this pill is fine’ and then we all live happily ever after? 🤡
Let’s not forget the 2021 blood pressure recall. Or the 2018 valsartan NDMA scandal. Or the 2020 metformin contamination. Oh wait-you didn’t mention those because you’re too busy high-fiving the FDA for being ‘efficient.’
Maybe the real question is: why are we okay with our life-saving meds being made in factories with zero transparency?
And why does the ‘affordable’ generic cost more than my rent?
Lynn Steiner
December 12, 2025 AT 07:02Every time I see a generic, I think about how my grandpa couldn’t afford his insulin in 2008. Now my cousin gets it for $4. That’s not just science-that’s justice. 🇺🇸
So yeah, the FDA’s slow. So what? At least they don’t let poison into the system. You want cheap? Go to a shady website. I’ll take the 10-month wait over a dead kid any day.