When your asthma gets worse every spring, or after you vacuum the living room, or when your cat jumps onto the bed - it’s not just bad luck. It’s likely your allergies are fueling your asthma. This isn’t rare. About 60% of adults with asthma have allergic asthma, where everyday allergens like pollen, dust mites, or pet dander trigger inflammation in the airways. The result? Wheezing, coughing, chest tightness - and more frequent rescue inhaler use. But here’s the good news: if you can identify and manage the allergic trigger, you can take back control.
Why Allergies Make Asthma Worse
Allergic asthma doesn’t just mean you’re sneezing and itchy-eyed while your lungs are also acting up. It’s a deeper connection. When you breathe in an allergen - say, cat dander - your immune system overreacts. It releases IgE antibodies, which then activate mast cells. These cells dump histamine and other inflammatory chemicals directly into your airways. That’s when the swelling, mucus production, and muscle tightening happen - the same process that causes asthma symptoms. This isn’t just a coincidence. It’s a pattern. Most people with allergic asthma developed allergies first - often as kids. Eczema, then hay fever, then asthma. That’s called the “allergic march.” By age 12, about 70% of kids with asthma already have confirmed allergies. In adults, it’s still common: 50% of asthma patients test positive for one or more allergens. The more allergens you’re sensitive to, the worse your asthma tends to be.How Doctors Diagnose the Overlap
If you’ve got asthma and your symptoms flare with certain exposures, your doctor should check for allergies. The gold standard? Skin prick testing. A tiny drop of allergen is placed on your skin, then lightly pricked. If you’re sensitive, a small red bump appears within 15 minutes. It’s quick, accurate, and 95% sensitive for common triggers like pollen, dust mites, and pet dander. Blood tests that measure specific IgE levels are also used, especially if skin testing isn’t possible. But neither test alone is enough. You need both: positive allergy tests and asthma symptoms that match exposure. Spirometry - the breathing test that measures airflow - confirms asthma. If your lung function improves after using a rescue inhaler, that’s another clue. Many people never get tested. A 2022 survey found that only 35% of primary care doctors routinely screen asthma patients for allergies. That’s a problem. The European Academy of Allergy and Clinical Immunology says 30% of people with poorly controlled asthma have undiagnosed allergies. If you’re using your inhaler more than twice a week, it’s time to ask.Managing the Trigger: Avoidance That Actually Works
Avoiding allergens sounds simple - until you try it. Dust mites live in bedding, carpets, and stuffed animals. Pet dander clings to clothes, furniture, and air vents. Pollen floats in on the breeze. You can’t eliminate them completely, but you can cut exposure significantly. For dust mites: Use allergen-proof mattress and pillow covers. Wash bedding weekly in hot water (130°F or higher). Keep indoor humidity below 50%. Vacuum weekly with a HEPA-filter vacuum - Consumer Reports found these reduce dust mite allergens by 85% when used regularly. For pets: Keep them out of the bedroom. Wash them every two weeks. Use an air purifier with a HEPA filter in the main living area. One patient on the Asthma and Allergy Foundation forum said removing her cat from the bedroom cut her rescue inhaler use from four times a week to once a month. For pollen: Check daily pollen forecasts. Apps like Allergy Alert give hyperlocal data. Stay indoors on high-pollen days, especially in the morning. Change clothes and shower after being outside. Keep windows closed during peak season. It takes time - 2 to 4 weeks - for these changes to make a real difference. But for many, it’s the first step toward breathing easier without more meds.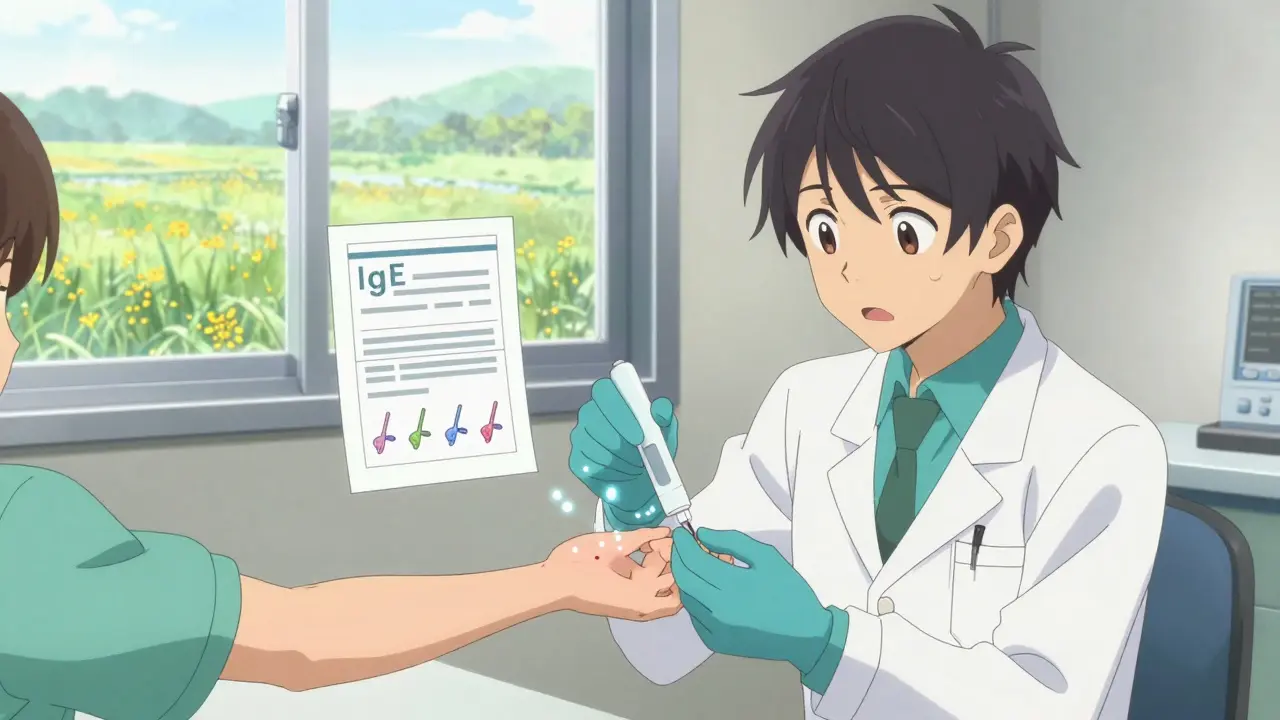
Immunotherapy: Rewiring Your Immune System
If avoidance isn’t enough, allergen immunotherapy - commonly called allergy shots - can change the game. It’s not a quick fix. You get regular injections over 3 to 5 years. But it’s the only treatment that can actually modify the disease, not just mask symptoms. How it works: Small, increasing doses of your trigger allergens are injected under the skin. Over time, your immune system learns not to overreact. Studies show it reduces asthma symptoms by 40-60% and cuts medication use by nearly half. One 2020 study found it saved patients about $1,200 a year in asthma meds. There’s also sublingual immunotherapy - tablets you dissolve under your tongue. These are FDA-approved for grass and ragweed allergies and are becoming more popular. They’re less invasive than shots but still require daily use for years. The catch? It takes months to start working. The first 3-6 months involve weekly or monthly visits. Some people get temporary worsening of symptoms during dose increases. That’s why 31% quit within the first year. But those who stick with it? 78% report moderate to significant improvement. One patient on the COPD Foundation forum cut his steroid inhaler dose in half after two years and hasn’t needed oral steroids in 18 months.Biologics: Targeted Drugs for Severe Cases
For people with severe allergic asthma that doesn’t respond to standard treatments, biologics are a breakthrough. These are injectable or IV drugs that block specific parts of the immune response. Omalizumab (Xolair) targets IgE - the antibody that kicks off allergic reactions. The INNOVATE trial showed it cuts asthma exacerbations by 50%. Dupilumab (Dupixent) blocks IL-4 and IL-13, two key inflammation drivers. It’s approved for both asthma and eczema. And tezepelumab (Tezspire), approved in 2021, works even in people without high eosinophil levels - making it one of the first biologics effective for both allergic and non-allergic severe asthma. These drugs aren’t cheap. Annual costs range from $25,000 to $35,000. But for someone who’s in the ER every few months, the cost of hospital visits and missed work often outweighs the drug price. They’re also highly targeted: blood tests for eosinophils (a type of white blood cell) and FeNO (fractional exhaled nitric oxide) help doctors decide who will respond best.What Doesn’t Work - and Why
Not every asthma patient with allergies will benefit equally from allergy-focused treatments. Dr. Sally Wenzel from the University of Pittsburgh points out that asthma isn’t one disease. It’s many. Some people have mostly eosinophilic inflammation. Others have neutrophilic or mixed patterns. Allergies might be the trigger for one person, but for another, it’s cold air, stress, or pollution. That’s why some patients don’t improve even after immunotherapy or biologics. Their inflammation is driven by something else. That’s why GINA’s 2023 guidelines now recommend testing for biomarkers like eosinophils and FeNO to guide treatment. It’s precision medicine - matching the right drug to the right inflammation pattern. Also, don’t rely on “natural” remedies like essential oils or herbal supplements. There’s no solid evidence they reduce airway inflammation. In fact, some essential oils can irritate the airways and trigger attacks.
What You Can Do Today
If you have asthma and suspect allergies are making it worse:- Track your symptoms. When do they flare? After being outside? After cleaning? Around pets?
- Ask your doctor for allergy testing - skin prick or blood test.
- Start simple environmental changes: allergen-proof bedding, HEPA vacuum, keep pets out of the bedroom.
- If you’re using your rescue inhaler more than twice a week, talk to your doctor about stepping up treatment.
- Consider seeing an allergist if your asthma isn’t under control. They’re trained to connect the dots between allergies and breathing problems.
Real People, Real Results
On the AAFA forum, 68% of 1,247 people with allergic asthma said identifying and avoiding triggers improved their lives. On Reddit, 52% of users complained about insurance denying coverage for allergy testing - out-of-pocket costs can hit $250-$400. But those who got tested and acted on results saw dramatic changes. One man in Ohio stopped needing oral steroids after two years of allergy shots for dust mites. A woman in Seattle cut her inhaler use by 80% after switching to a HEPA air purifier and removing carpet from her bedroom. These aren’t outliers. They’re the rule when allergy and asthma are treated together.The Bigger Picture
The global allergy diagnostics market is growing fast - projected to hit $4.1 billion by 2027. Health systems like Kaiser Permanente now require allergy testing for asthma patients with uncontrolled symptoms. Their results? A 22% drop in hospitalizations. The future is personalized. Multi-allergen immunotherapy tablets are in phase 3 trials. New biologics are being tested to block different inflammatory pathways. The goal? To stop asthma before it flares - not just treat it after. But access remains a problem. In low-resource areas, 75% of asthma patients can’t get basic allergy testing. That’s a global health gap. Here in the U.S., we have tools - we just need to use them.Is allergic asthma the same as regular asthma?
No. Allergic asthma is triggered by allergens like pollen, dust mites, or pet dander, while non-allergic asthma is caused by factors like cold air, exercise, stress, or pollution. The symptoms are similar, but the triggers and treatments differ. Allergic asthma often starts in childhood and responds better to inhaled steroids and allergy-focused treatments like immunotherapy.
Can allergy shots cure asthma?
No, but they can significantly reduce how often and how badly your asthma flares. Allergen immunotherapy doesn’t cure asthma - it changes how your immune system reacts to allergens. Over 3-5 years, many patients see a 40-60% drop in symptoms and need less medication. Some even stop using daily inhalers. It’s disease modification, not a cure.
How do I know if I have allergic asthma?
Look for patterns: Do your asthma symptoms get worse during pollen season? After being around pets? After cleaning? If yes, get tested. Skin prick tests or blood tests for specific IgE can confirm allergies. If those are positive and you have asthma symptoms that match exposure, you likely have allergic asthma. Your doctor may also check your blood eosinophil count or FeNO levels to support the diagnosis.
Are biologic therapies worth the cost?
For people with severe allergic asthma who keep ending up in the ER or needing oral steroids, yes. Biologics like omalizumab or dupilumab can cut exacerbations by 50% or more. While they cost $25,000-$35,000 a year, the savings from avoided hospital visits, missed work, and emergency care often make them cost-effective. Insurance usually requires proof of poor control with standard treatments before approving them.
Can I stop my asthma inhaler if I start allergy shots?
Not right away. Allergy shots take months to start working. You should continue your prescribed inhaler unless your doctor says otherwise. Over time, as your symptoms improve, your doctor may gradually reduce your medication. Many patients end up on lower doses or stop daily controllers after 2-3 years of successful immunotherapy. Never stop medication without medical supervision.

 Vitamin E and Warfarin: What You Need to Know About the Bleeding Risk
Vitamin E and Warfarin: What You Need to Know About the Bleeding Risk
 Guide to Affordable Cialis Soft Online: Maximizing Sexual Health
Guide to Affordable Cialis Soft Online: Maximizing Sexual Health
 A Comprehensive Guide to Calcium Acetate Safety and Toxicity
A Comprehensive Guide to Calcium Acetate Safety and Toxicity
 Litigation in Generic Markets: How Patent Disputes Delay Affordable Medicines
Litigation in Generic Markets: How Patent Disputes Delay Affordable Medicines
 How Azilsartan Affects Blood Pressure in Psoriasis Patients
How Azilsartan Affects Blood Pressure in Psoriasis Patients
Christine Détraz
December 22, 2025 AT 21:19Been dealing with this since I was 8. Got diagnosed with eczema, then hay fever, then asthma by 14. No one ever connected the dots until I was 28. Skin test showed I’m allergic to dust mites, cat dander, and ragweed. Started using mattress covers, HEPA filter, and kept my cat out of the bedroom. My rescue inhaler use dropped from daily to once a week. It’s not magic, it’s just science you ignore until you’re gasping for air at 3 a.m.
Also, stop listening to people who say ‘just breathe through it.’ It’s not a mindset thing. It’s biology.
Katie Taylor
December 23, 2025 AT 17:11Y’all need to stop being lazy. If your asthma sucks, get tested. Don’t wait for your doctor to bring it up. Go to an allergist. Pay out of pocket if you have to. I spent $350 on a skin test and saved $2,000 a year on ER visits. This isn’t optional. Your lungs are not a suggestion box.
Blow Job
December 25, 2025 AT 16:54My mom had allergic asthma. She did allergy shots for 5 years. She stopped needing prednisone. She stopped waking up wheezing. She lived to 82. I’m doing the same thing now. It’s not glamorous. It’s not quick. But it works if you don’t quit after the first shot.
Don’t let the cost scare you. Ask about payment plans. Ask about clinical trials. Don’t just accept ‘this is just how it is.’
Jillian Angus
December 27, 2025 AT 05:46my cat sleeps on my chest and i breathe fine
maybe its all in my head
but then again i dont have asthma so idk lol
Isaac Bonillo Alcaina
December 27, 2025 AT 20:16Let me guess - you’re one of those people who think biologics are ‘miracle cures’ while ignoring the fact that 30% of patients still flare. The pharmaceutical industry loves to sell hope, not results. You think immunotherapy is the answer? Look at the dropout rate. 31% quit in the first year because it’s exhausting, expensive, and doesn’t guarantee anything.
Meanwhile, your inhaler costs $30. The shots cost $15,000 a year. Who’s really profiting here? Not you. And don’t tell me ‘it’s worth it’ - I’ve seen people bankrupt themselves chasing ‘perfect control.’ It’s a scam dressed in white coats.
Payson Mattes
December 28, 2025 AT 22:38Did you know the CDC is hiding the truth about allergens? They’re not just in your house - they’re in the water supply, the vaccines, the 5G towers. That’s why your symptoms get worse when you vacuum - it’s not dust mites, it’s nano-particles from government spray programs. I’ve been tracking my symptoms since 2018 and the spikes always line up with EPA announcements.
Also, HEPA filters don’t work because they can’t block electromagnetic allergens. You need a Faraday cage around your bed. I built mine out of aluminum foil and it cut my attacks by 70%.
Ps. Don’t trust your doctor. They’re paid by Big Pharma to keep you hooked on inhalers.
Joe Jeter
December 30, 2025 AT 09:45Everyone’s so obsessed with ‘allergies causing asthma’ like it’s some new revelation. Newsflash - asthma has always been about inflammation. Allergies are just one trigger among dozens. You think removing your cat is going to fix your airway remodeling? Nah. You’re just distracting yourself from the real issue: your lungs are damaged and you’re trying to blame your pet.
Also, why do we treat asthma like a lifestyle product? ‘Buy this pillow. Use this vacuum. Avoid this pollen.’ What about fixing the actual disease? We’re treating symptoms like a menu item instead of a medical condition. Pathetic.
Bhargav Patel
December 31, 2025 AT 18:23There is a profound metaphysical truth here: the body does not mistake allergens for threats - it responds to the dissonance between internal harmony and external disruption. The immune system, like the mind, seeks equilibrium. When we live in environments saturated with synthetic materials, chemical cleaners, and chronic stress, our biology interprets these as violations of natural order.
Thus, dust mites are not the enemy - they are mirrors. The true allergen is our disconnection from rhythm - of breath, of season, of silence. Immunotherapy may quiet the signal, but it does not restore the song.
Consider this: in cultures where indoor air is naturally ventilated, where homes are built of earth and wood, allergic asthma is rare. Not because they are immune - but because they have not severed their relationship with the living world.
Perhaps the cure is not in more injections, but in fewer walls.
John Pearce CP
January 1, 2026 AT 00:40It's appalling that this article treats allergic asthma as if it's a uniquely American problem. In Europe, they've had this figured out since the 1970s. We have the science, the diagnostics, the treatments - yet we still have people living in mold-infested housing, refusing to remove pets, and blaming their condition on ‘stress.’
This isn’t a medical issue - it’s a cultural failure. We prioritize convenience over health. We’d rather buy a $500 air purifier than fix the leaky window letting in mold. We’d rather take a pill than clean our carpets.
And now we’re spending $30,000 on biologics while ignoring basic public health infrastructure? Shameful. If you can’t afford to live in a clean environment, then your asthma isn’t medical - it’s a consequence of systemic neglect. And that’s not a diagnosis. That’s a verdict.