When your liver gets scarred, it doesn’t heal the way your skin does. Instead of repairing itself, it builds hard, fibrous tissue that blocks blood flow and stops it from working right. This is cirrhosis-the end stage of long-term liver damage. It’s not a single disease. It’s the result of years of injury from alcohol, hepatitis, fatty liver, or other causes. And once it’s advanced, no pill can undo it. But catching it early? That changes everything.
What Happens Inside the Liver During Cirrhosis?
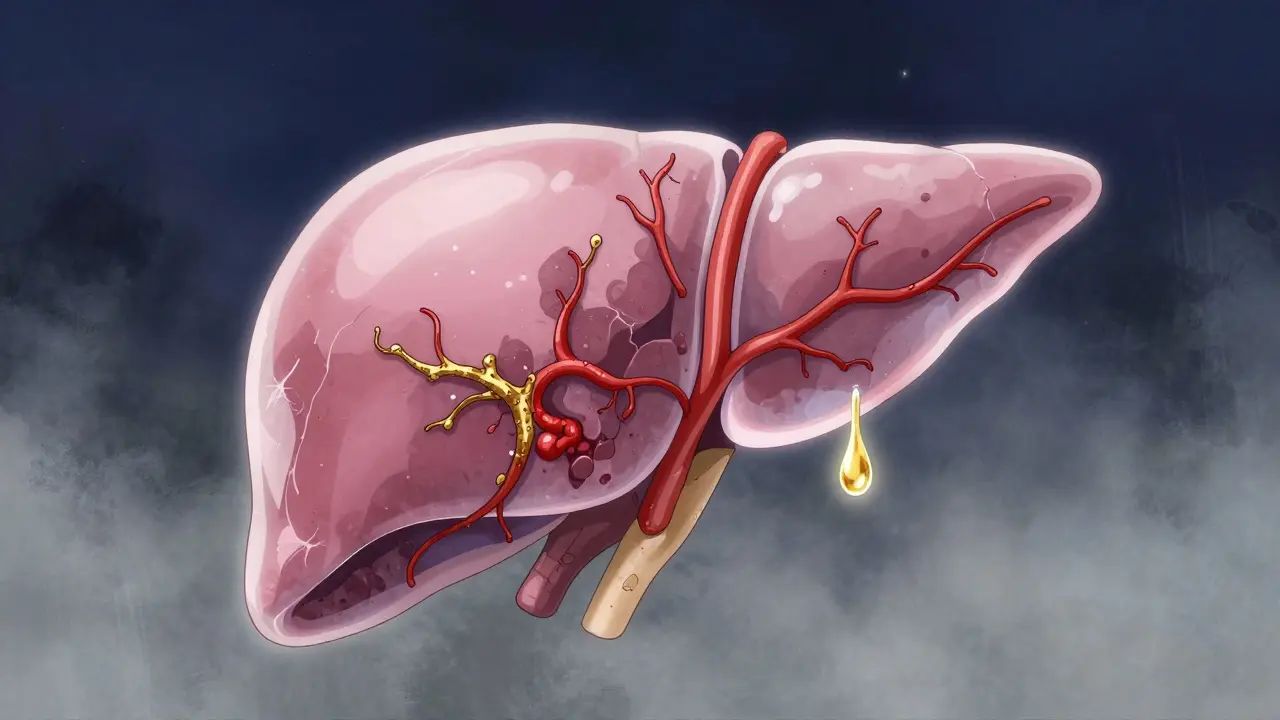
Your liver is tough. It can handle a lot-alcohol, toxins, medications-until it can’t. Every time liver cells get damaged, the body tries to fix them. But if the damage keeps coming, the repair process goes wrong. Instead of healthy cells, it lays down scar tissue. Over time, this scar builds up in thick bands, cutting off blood vessels and crushing the remaining healthy tissue into nodules. This isn’t just about structure. It breaks function. The liver can’t clean your blood properly. It stops making proteins like albumin that keep fluid in your veins. It can’t process nutrients, make bile for digestion, or produce clotting factors. Blood backs up, pressure rises in the portal vein, and fluid leaks into your belly-that’s ascites. Toxins build up in your brain, causing confusion or forgetfulness-this is hepatic encephalopathy. Doctors measure this damage with tests. A MELD score (Model for End-Stage Liver Disease) uses bilirubin, creatinine, and INR to predict survival. A score above 15 means you’re at serious risk. Ultrasound elastography can now measure liver stiffness without a biopsy. Values over 12.5 kPa strongly suggest cirrhosis. Blood tests show low albumin, high bilirubin, and low platelets-all signs the liver is failing.Compensated vs. Decompensated: The Critical Divide
Not all cirrhosis is the same. There are two stages, and the difference between them is life-or-death. In compensated cirrhosis, the liver is scarred but still doing enough to keep you alive. You might feel fine. No swelling. No confusion. No vomiting blood. Many people don’t even know they have it until a routine blood test shows abnormal liver enzymes. About 80-90% of people in this stage survive five years. Then comes decompensated cirrhosis. That’s when the liver can’t keep up anymore. Fluid fills your belly. You get confused or drowsy. You start bleeding from swollen veins in your esophagus. Your kidneys start to shut down. At this point, survival drops to 20-50% over five years. And there’s no turning back. No drug can reverse the scarring. The only real fix is a transplant. This is why early detection matters. If you have hepatitis C, heavy drinking, or obesity with fatty liver, get checked. A simple ultrasound and blood panel can catch cirrhosis before it becomes life-threatening.What Causes Cirrhosis Today?
The causes have shifted. Ten years ago, alcohol and hepatitis C were the big ones. Now, non-alcoholic fatty liver disease (NAFLD) is the fastest-growing cause in the U.S. It’s linked to obesity, diabetes, and metabolic syndrome. About 24% of all cirrhosis cases now come from NAFLD-more than alcohol. Alcohol still plays a major role. Chronic heavy drinking over 10+ years damages liver cells directly. Hepatitis B and C can silently scar the liver for decades before symptoms appear. Autoimmune hepatitis, genetic conditions like hemochromatosis, and long-term bile duct blockages also lead to cirrhosis. The key point: all these causes lead to the same end result. The liver doesn’t care if the damage came from a beer, a virus, or excess sugar. It responds the same way-with scar tissue.
Can You Reverse Cirrhosis?
Here’s the hard truth: once cirrhosis is established, the scarring is permanent. No pill, supplement, or diet can erase it. But here’s the hopeful part: if you catch it early-while it’s still compensated-you can stop it from getting worse. And in some cases, the liver can improve enough to function better. If you have alcohol-related cirrhosis and quit drinking, your risk of death drops by 50% in five years. If you have hepatitis C and get cured with antivirals, fibrosis can regress in up to 70% of cases. If you lose weight and control diabetes with NAFLD, liver inflammation can improve. This isn’t a cure. It’s damage control. The scar tissue stays. But the liver can still do its job-if you stop the attack.When Is a Liver Transplant the Only Option?
A liver transplant isn’t a last resort. It’s the only cure for decompensated cirrhosis. In the U.S., about 40% of all liver transplants are done for cirrhosis. The system uses the MELD-Na score to decide who gets priority. Higher scores mean higher risk of death without a transplant. A score above 15 puts you on the urgent list. Over 14,000 people are waiting right now. Only about 8,800 livers become available each year. That means 12% of people on the list die before they get one. Transplant isn’t simple. You need to be healthy enough to survive surgery. No active cancer. No uncontrolled infection. No recent substance use (usually 6 months sober). You’ll need lifelong immunosuppressants to prevent rejection. But the results are powerful: 80-90% of patients survive five years after transplant, and most return to normal life. New techniques are helping. Machines that keep donor livers alive and beating outside the body (normothermic perfusion) are increasing the number of usable organs by 22%. Researchers are also testing lab-grown liver cells and bioartificial livers-tools that might one day bridge the gap until a transplant is available.What Does Daily Life Look Like With Cirrhosis?
Living with cirrhosis means constant management. Diet is critical. Sodium must be under 2,000 mg a day to fight fluid buildup. Protein needs to be balanced-too little causes muscle loss, too much can trigger brain fog. Alcohol? Absolutely off-limits. Even one drink can push you into decompensation. Medications change. Your liver can’t process drugs the way it used to. Painkillers like ibuprofen or Tylenol in high doses can be deadly. Antibiotics, sedatives, and even some herbal supplements need careful review. Always check with your hepatologist before taking anything new. Symptoms you can’t ignore: confusion, yellow eyes, sudden belly swelling, vomiting blood, or extreme fatigue. These aren’t normal aging. They’re red flags. Support matters. A 2022 Cleveland Clinic study found that patients with access to multidisciplinary teams-doctors, dietitians, social workers, addiction counselors-had 40% fewer hospital visits. The American Liver Foundation offers nurse navigation (1-800-GO-LIVER) to help people find specialists, understand insurance, and connect with peer groups.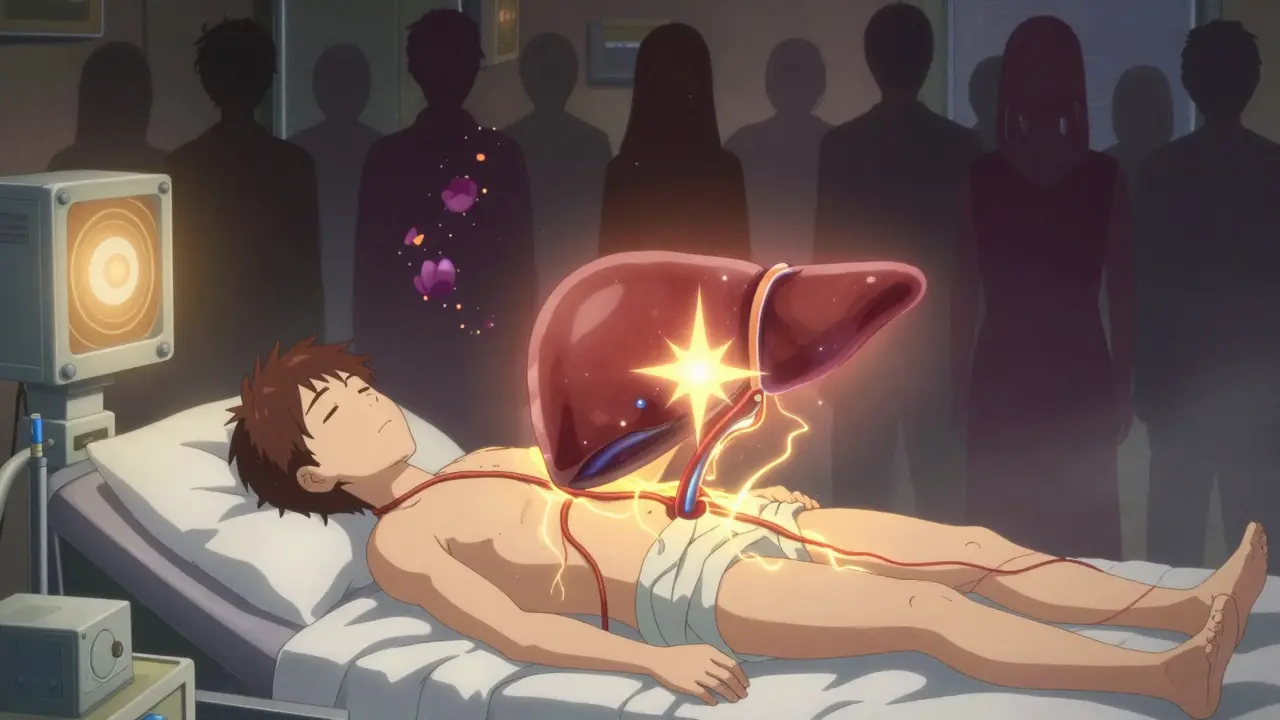
What’s Next for Cirrhosis Treatment?
The future is moving fast. New drugs are in trials. One, called simtuzumab, targets the fibrosis process itself and slowed scarring by 30% in early NASH-related cirrhosis. Another, obeticholic acid, is already approved for a rare form of cirrhosis and may help others soon. Non-invasive testing is getting better. MRI elastography now detects cirrhosis with 90% accuracy-better than ultrasound. Blood tests that measure specific fibrosis markers are being developed to replace biopsies entirely. The big shift? From staging by symptoms to staging by molecular signals. Researchers are learning to read the liver’s genetic fingerprint. Soon, treatment may be tailored not just to whether you have cirrhosis, but to what kind-alcohol-driven, fat-driven, virus-driven-and how fast it’s progressing. But the biggest challenge remains: organ shortage. Until we solve that, prevention and early intervention are the most powerful tools we have.Frequently Asked Questions
Can cirrhosis be cured without a transplant?
No, cirrhosis itself cannot be cured once scar tissue has formed. But if caught early in the compensated stage, removing the cause-like quitting alcohol, curing hepatitis C, or losing weight-can stop further damage and allow the liver to function better. The scarring doesn’t disappear, but the liver can adapt and avoid progression to life-threatening complications.
How do I know if I have cirrhosis if I feel fine?
Many people with early cirrhosis have no symptoms. Routine blood tests showing elevated liver enzymes, low platelets, or abnormal protein levels can raise the red flag. An ultrasound with elastography or a FibroScan can measure liver stiffness. If you have risk factors-like heavy drinking, obesity, hepatitis B or C, or diabetes-ask your doctor for screening even if you feel okay.
Is a liver transplant the only option for advanced cirrhosis?
Yes, for decompensated cirrhosis with complications like ascites, bleeding, or hepatic encephalopathy, a transplant is the only treatment that restores long-term survival. Other treatments manage symptoms but don’t fix the underlying liver failure. Without a transplant, most people with advanced cirrhosis die within a few years.
How long is the wait for a liver transplant?
It varies widely. In the U.S., the average wait is 3 to 5 years, but it depends on your MELD-Na score, blood type, and location. People with higher scores (above 20) get priority and may wait only weeks or months. Those with lower scores can wait years. About 12% of people on the waiting list die before a liver becomes available.
Can I drink alcohol after a liver transplant for cirrhosis?
Absolutely not. Even a small amount of alcohol can damage the new liver and trigger rejection or new scarring. Transplant centers require lifelong abstinence from alcohol, especially if cirrhosis was caused by drinking. Violating this rule can lead to loss of the transplant and removal from the waiting list.
 How Azilsartan Affects Blood Pressure in Psoriasis Patients
How Azilsartan Affects Blood Pressure in Psoriasis Patients
 Peru Balsam: The Life-Changing Dietary Supplement You Need to Experience
Peru Balsam: The Life-Changing Dietary Supplement You Need to Experience
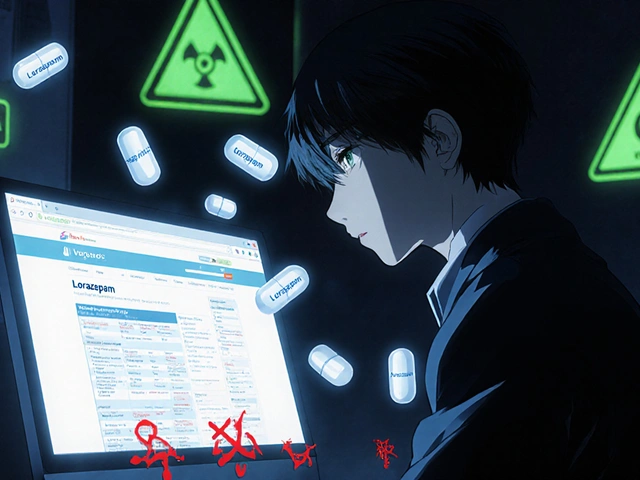 Buy Online Cheap Generic Ativan: What You Need to Know Before You Order
Buy Online Cheap Generic Ativan: What You Need to Know Before You Order
 IBS-Mixed: How to Manage Alternating Constipation and Diarrhea
IBS-Mixed: How to Manage Alternating Constipation and Diarrhea
 How Clinician Communication Shapes Patient Trust in Generic Medications
How Clinician Communication Shapes Patient Trust in Generic Medications
Sarthak Jain
December 16, 2025 AT 10:55bro i had a fibroscan last year after my doc saw my alt was skyhigh. 14.2 kpa. they said early cirrhosis. i quit beer cold turkey and lost 35 lbs. my last scan was 9.8. liver's still scarred but it's chillin now. no more jager bombs.
Daniel Wevik
December 18, 2025 AT 01:15the MELD-Na score is the real gatekeeper. if you're above 15, you're in the urgent pool. below 10, you're basically invisible to the system. it's not about who's sicker-it's about who's gonna die fastest without a transplant. brutal math, but it's what we've got.
Rulich Pretorius
December 18, 2025 AT 05:09it's fascinating how the liver doesn't care about the origin of the damage. whether it's ethanol, hepatitis, or fructose syrup-the hepatocyte just sees stress and responds with fibrosis. evolution didn't prepare us for 2000 calories of high-fructose corn syrup a day. our livers are ancient organs in a modern world.
Thomas Anderson
December 18, 2025 AT 16:31if you're overweight and drink soda daily, get a fibroscan. no excuses. it's a 10-minute scan. cheaper than your monthly energy drinks. save your liver before it's too late.
Natalie Koeber
December 19, 2025 AT 21:37they say NAFLD is the new big cause... but i bet big pharma pushed this to sell more meds. they don't want you to know the real cause: glyphosate in our food. liver damage from Roundup. they hide it behind 'metabolic syndrome' to sell statins and insulin. check the studies-they're all funded by Big Ag.
Rich Robertson
December 20, 2025 AT 13:31my uncle got a transplant in '19. 7 years sober. now he's hiking in the Rockies. the immunosuppressants are a pain-constant blood tests, infections, the whole deal-but he's alive. he says the real miracle isn't the new liver, it's the fact that he finally stopped pretending he could drink and be fine.
Dwayne hiers
December 21, 2025 AT 08:38normothermic perfusion is a game-changer. it keeps donor livers metabolically active outside the body, allowing for functional assessment and even repair. we're moving from static organ storage to dynamic organ maintenance. this could increase the donor pool by 30%+ in the next 5 years. the future of transplant logistics is alive and beating.
Tim Bartik
December 22, 2025 AT 01:34they say you gotta be sober 6 months before transplant? bullcrap. my cousin got one after 3 weeks. they don't care about your past if you got the right insurance and the right last name. the system's rigged for the rich. poor folks die waiting while billionaires get liver #22.
Wade Mercer
December 23, 2025 AT 10:54people don't realize alcohol-related cirrhosis is 100% preventable. if you're drinking enough to scar your liver, you're not just hurting yourself-you're being selfish. you're wasting a scarce organ that could go to someone who didn't choose to destroy theirs.
Jonny Moran
December 24, 2025 AT 20:19if you're reading this and you're scared-good. that means you care. reach out to the American Liver Foundation. talk to a nurse navigator. you don't have to figure this out alone. thousands of people have walked this path. you can still have a full life-even with cirrhosis. just don't wait until you're vomiting blood to act.
Daniel Thompson
December 25, 2025 AT 07:49your post is medically accurate, well-researched, and clinically relevant. however, I must note that the omission of any discussion regarding the role of gut microbiota in portal hypertension and hepatic encephalopathy represents a significant gap in the current understanding of cirrhosis pathophysiology. Recent studies in Nature Gastroenterology (2023) indicate that fecal microbiota transplantation may modulate ammonia metabolism and reduce encephalopathy episodes by up to 40% in compensated patients. This should be considered in future iterations of clinical guidelines.