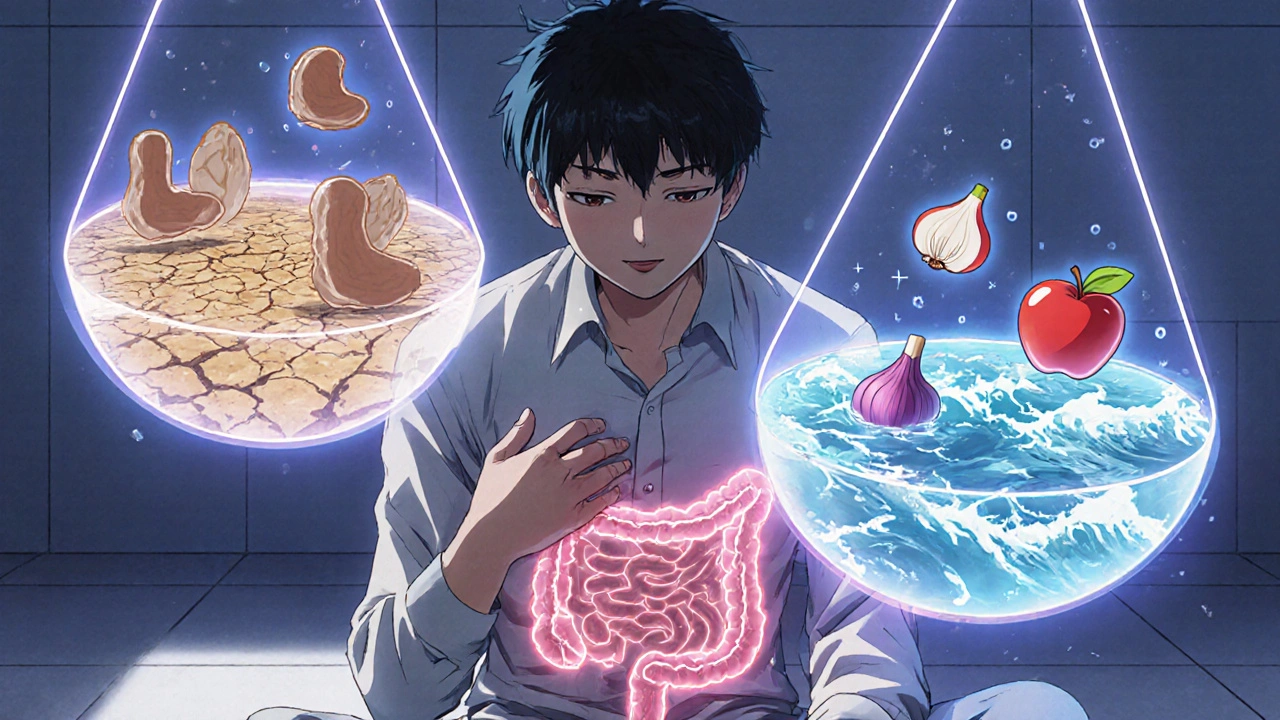
Living with IBS-Mixed means your gut feels like a pendulum-sometimes stuck in constipation, other times racing toward diarrhea. One day you’re struggling to go, the next you’re stuck near a bathroom. It’s exhausting. And frustrating. You’re not alone. About 1 in 5 people with IBS experience this back-and-forth pattern, known as IBS-Mixed or IBS-M. Unlike Crohn’s or colitis, there’s no inflammation to see on a scan. No tumors. No bleeding. Just pain, bloating, and unpredictable bowel habits that make planning a trip, a date, or even a workday feel risky.
What Exactly Is IBS-Mixed?
IBS-Mixed isn’t just "IBS that acts up." It’s a specific diagnosis defined by the Rome IV criteria: recurrent abdominal pain at least once a week for three months, with bowel movements that alternate between hard/lumpy (Bristol Stool Scale 1-2) and loose/watery (Bristol Stool Scale 6-7) in at least 25% of episodes. That means if you have 20 bowel movements in a month, at least 5 need to be constipated and 5 diarrhea. The rest can be normal, but the pattern has to be consistent over time.
Doctors rule out other things first-celiac disease, thyroid issues, colon cancer-before labeling it IBS-M. Blood tests, stool tests, and sometimes a colonoscopy are used to check for red flags. If those come back clean and your symptoms match the criteria, you’ve got IBS-M. It’s not "all in your head." It’s real biology: your gut nerves are oversensitive, your muscles move too fast or too slow, and the bacteria in your intestines are out of balance.
Why Is IBS-Mixed So Hard to Treat?
Here’s the catch: what helps one symptom often makes the other worse. Take loperamide (Imodium). It slows down diarrhea-great, right? But if you take it during a constipation phase, you’re stuck. Same with laxatives. Polyethylene glycol (Miralax) can help you go, but if you’re already having loose stools, it turns things into a mess.
Even medications made for IBS have mixed results in IBS-M. Linaclotide, approved for constipation-predominant IBS, only helped about 22% of IBS-M patients in clinical trials. Eluxadoline, for diarrhea-predominant IBS, worked for just 19%. That’s because IBS-M isn’t one problem-it’s two, happening in the same body, sometimes on the same day.
That’s why most successful plans don’t rely on a single pill. They combine diet, stress control, and smart, flexible medication use.
Diet: The Low FODMAP Diet Works-But It’s Not Easy
The most researched and effective dietary approach for IBS-M is the low FODMAP diet. FODMAPs are short-chain carbs that ferment in the gut and pull water in, triggering bloating, gas, and changes in bowel speed. High-FODMAP foods include onions, garlic, wheat, dairy (lactose), apples, honey, and artificial sweeteners like sorbitol.
Studies show 50-60% of IBS-M patients see improvement on this diet. That’s lower than the 70-75% seen in IBS-D, but still significant. The trick? It’s not about cutting out forever. It’s a three-step process:
- Elimination (2-6 weeks): Remove all high-FODMAP foods. Stick to low-FODMAP options like bananas, oats, eggs, chicken, spinach, and lactose-free dairy.
- Reintroduction (8-12 weeks): Add one FODMAP group back at a time-like onions, then apples, then milk-and track symptoms. This tells you exactly what triggers you.
- Personalization: Keep the foods you tolerate and avoid only what causes trouble.
Doing this alone is tough. Most people mess up the reintroduction phase and give up. Working with a registered dietitian who specializes in IBS cuts your chances of failure in half. Apps like Monash University’s FODMAP app help you scan food labels and track triggers.
Real talk: 52% of people burn out on strict diets after six months. That’s normal. You don’t have to be perfect. Aim for 80% adherence. If you eat garlic at a friend’s dinner, don’t panic. Just go back to your plan the next day.
Medications: Have a Plan for Both Sides
Since you can’t predict which bowel habit will show up, the best strategy is to keep two medications on hand-one for constipation, one for diarrhea-and use them only when needed.
- For constipation: Polyethylene glycol (Miralax) 17g daily is gentle and doesn’t cause cramping. Magnesium citrate works fast but can be too strong-use only during flare-ups.
- For diarrhea: Loperamide (Imodium) 2-4mg as needed. Don’t take it daily. It can cause constipation if overused.
For pain and bloating, antispasmodics like dicyclomine (Bentyl) 10-20mg before meals can help. They relax gut muscles and reduce cramping. About 40-50% of IBS-M patients report relief.
Antidepressants might sound surprising, but they’re one of the most effective tools for IBS-M. Low-dose tricyclics like amitriptyline (10-25mg at night) don’t treat depression here-they calm nerve signals in the gut. Studies show 55-60% of IBS-M patients get better pain control and fewer bowel fluctuations. SSRIs like sertraline help too, but tricyclics are better for pain.
Peppermint oil capsules (IBgard) are another option. They’re enteric-coated so they release in the small intestine, not the stomach. In user surveys, 68% report less pain and 57% say bloating drops. Side effects? A small number get heartburn.

Stress and the Gut-Brain Connection
Stress doesn’t cause IBS-M, but it lights the fuse. In one study, 68% of IBS-M patients said anxiety or emotional stress made their symptoms worse. That’s because your gut and brain are wired together. When you’re stressed, your nervous system sends signals that speed up or slow down digestion-exactly what triggers alternating symptoms.
That’s why cognitive behavioral therapy (CBT) is a first-line recommendation from the American Gastroenterological Association. CBT doesn’t mean you’re "crazy." It means you’re learning how to change how your brain responds to gut signals. In trials, CBT reduced symptom severity by 40-50%. Online programs like the Nerva app or Face-to-Face CBT with a therapist trained in IBS are proven to work.
Other stress tools: daily breathing exercises (5 minutes, 4-7-8 technique), yoga, or even regular walks. Movement calms the nervous system. You don’t need to meditate for an hour. Start with 5 minutes a day.
What Doesn’t Work-and What to Avoid
Many people try quick fixes that backfire:
- Overusing laxatives: Leads to dependency and worsens diarrhea when you stop.
- Going gluten-free without celiac: Unless you have celiac disease, gluten isn’t the culprit. You’re probably just cutting out wheat, which is high in FODMAPs. That’s why it seems to help-but it’s not gluten.
- Drinking too much coffee: Caffeine speeds up your gut. 24% of IBS-M patients say it triggers diarrhea.
- Skipping meals or eating too fast: Both mess with gut motility. Eat slowly. Don’t skip breakfast.
Also, avoid fiber supplements that are insoluble-like wheat bran. They can irritate the gut. Stick to soluble fiber: psyllium husk (Metamucil) 5g daily. It softens stool without causing gas spikes.
Tracking Your Progress
You can’t manage what you don’t measure. Keep a daily log for at least 4 weeks. Track:
- Bowel movement (use the Bristol Stool Scale-pictures are easy to find online)
- Pain level (0-10)
- Food eaten
- Stress level
- Medications taken
Apps like Cara Care or GI Monitor make this easier than paper journals. Patients who use apps improve 35% more than those who write things down.
After a month, look for patterns. Do symptoms spike after dairy? After Friday nights out? After skipping sleep? That’s your roadmap.

What’s New in IBS-M Treatment?
There’s hope on the horizon. In 2023, a new drug called ibodutant showed 45% symptom improvement in IBS-M patients-nearly double the placebo rate. It’s not approved yet, but phase 3 trials are promising.
Microbiome testing is also evolving. Companies like Viome use AI to analyze your gut bacteria and suggest personalized diets. In a small 2023 study, users saw 58% symptom reduction. It’s expensive-around $300-but may become more accessible soon.
The Rome Foundation is updating its criteria for 2024. The new definition will require alternating symptoms in 30% of bowel movements instead of 25%. That might make diagnosis stricter, but it’ll also help researchers design better treatments.
Real-Life Success Stories
One user on Reddit, u/SarahIBS2022, went from 25 symptom days a month to 8 after 3 months on low FODMAP and daily peppermint oil. Another on HealthUnlocked found that combining dicyclomine with psyllium husk gave her steady relief. A third switched from trying one pill at a time to having Miralax and Imodium on standby-and learned to use them only when needed. Her quality of life improved in weeks.
There’s no magic cure. But there is control. And that’s what matters.
Final Thoughts
IBS-Mixed is complicated, but it’s manageable. You don’t need to be perfect. You don’t need to eliminate every trigger forever. You need a system: track your symptoms, eat what works, manage stress, and use meds smartly-not constantly.
The goal isn’t to never have a bad day. It’s to have more good ones. To plan a weekend trip without fear. To laugh without worrying about where the bathroom is. That’s possible. And it starts with understanding your body-not fighting it.
Can IBS-Mixed turn into Crohn’s disease or colitis?
No. IBS-Mixed is a functional disorder, meaning there’s no structural damage or inflammation in the gut. Crohn’s and ulcerative colitis are inflammatory diseases with visible damage on scans and blood tests. IBS-M doesn’t progress into these conditions. But if you develop new symptoms like weight loss, blood in stool, or fever, see a doctor-those aren’t typical IBS signs.
How long does it take to see improvement with the low FODMAP diet?
Most people notice changes within 2-6 weeks of starting the elimination phase. Some feel better in days, especially if they cut out caffeine or artificial sweeteners. But full results take time. The reintroduction phase is where you learn your triggers-and that can take another 8-12 weeks. Patience is key.
Is it safe to take laxatives and anti-diarrheals together?
Not at the same time. But using them separately based on your current symptoms is safe and recommended. For example, take Miralax if you’re constipated, and Imodium if you’re having diarrhea. Never take both on the same day unless directed by a doctor. Keep a symptom log so you know which one to use when.
Why do I feel fine in the morning but awful after lunch?
This is common. Your gut is most active after eating, especially after meals high in fat, sugar, or FODMAPs. The gastrocolic reflex triggers bowel movements after eating. If your gut is sensitive, this reflex becomes exaggerated. Try smaller, low-FODMAP meals. Avoid large lunches with fried foods or dairy. Eat slowly. Your gut will thank you.
Can IBS-Mixed go away on its own?
Rarely. IBS-Mixed is a chronic condition, but symptoms can improve significantly with the right management. Many people reach a point where flare-ups are mild, infrequent, and predictable. You might not be "cured," but you can live well. The goal isn’t elimination-it’s control.
What should I do if my doctor doesn’t take my symptoms seriously?
Keep a detailed symptom and food diary for at least 4 weeks. Print it out. Bring it to your next appointment. Mention the Rome IV criteria and ask if they’ve ruled out celiac disease and other red flags. If they dismiss you, ask for a referral to a gastroenterologist who specializes in functional GI disorders. Many clinics now have IBS programs. You deserve care that matches your experience.
 IP-6: The Dietary Supplement That's Taking the Health World by Storm
IP-6: The Dietary Supplement That's Taking the Health World by Storm
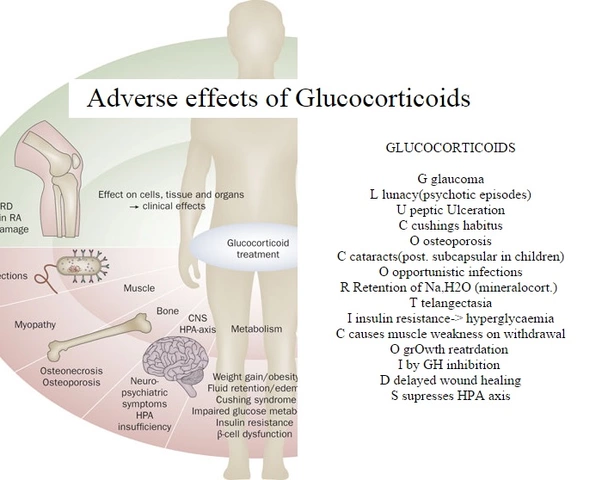
 Polypharmacy and Side Effects: How Taking Too Many Medications Increases Health Risks
Polypharmacy and Side Effects: How Taking Too Many Medications Increases Health Risks
 Wild Yam: The Unsung Hero of Natural Dietary Supplements
Wild Yam: The Unsung Hero of Natural Dietary Supplements
 The Link Between Bimatoprost and Dry Eye Syndrome
The Link Between Bimatoprost and Dry Eye Syndrome
 Feverfew and Anticoagulants: What You Need to Know About Bleeding Risk
Feverfew and Anticoagulants: What You Need to Know About Bleeding Risk
Deepa Lakshminarasimhan
November 12, 2025 AT 17:58okay but what if the real issue is glyphosate in our food supply? i’ve read studies-hidden in paywalls-that show it messes with gut bacteria way worse than FODMAPs. they don’t want you to know this because Big Ag owns the FDA. i went low-FODMAP for 6 months, still felt like garbage. switched to organic, no processed stuff, and boom-6 weeks later, my gut stopped playing roulette. they’re hiding the truth. i’m not crazy, i’m just the only one who read the papers.
Erica Cruz
November 13, 2025 AT 08:51lol at the low FODMAP diet. it’s just a fancy way to say ‘eat boring food and cry.’ 50-60% improvement? that’s not a cure, that’s a consolation prize. and peppermint oil? that’s what you give toddlers with gas. if you’re not on a $1200 microbiome test and a personalized IV drip of probiotics, you’re not even playing the game. also, why is everyone still using Miralax? it’s literally just sugar water with a fancy name.
Johnson Abraham
November 14, 2025 AT 12:08bruh i tried all this stuff. low fodmap? too hard. peppermint oil? made me heartburn. imodium? made me stuck for 3 days. miralax? same. i just drink coffee and pray. also why is everyone so serious? i’m just trying to get to the bathroom without crying. 🤡
Shante Ajadeen
November 16, 2025 AT 01:49i just want to say-this post helped me so much. i’ve had ibs-m for 8 years and felt so alone. the part about ‘aim for 80% adherence’ hit me in the chest. i thought i had to be perfect. i’ve been using miralax and imodium on an as-needed basis and keeping a simple log in my notes app. last week i ate garlic at a friend’s birthday and didn’t panic. i just went back to my plan the next day. it’s not about being flawless-it’s about being kind to yourself. you’re doing better than you think.
dace yates
November 16, 2025 AT 22:38so if ibs-m doesn’t turn into crohn’s, why do some people develop new symptoms like weight loss or blood in stool? is that just coincidence, or could it be misdiagnosed? i’ve seen people get labeled ‘ibs’ for years, then suddenly diagnosed with colitis. how do you know the difference for sure? any red flags i should watch for beyond what’s listed?
Danae Miley
November 18, 2025 AT 06:58The claim that ‘IBS-M doesn’t progress into Crohn’s or colitis’ is misleading. While IBS is a functional disorder, emerging longitudinal studies (e.g., Gut, 2022) show a statistically significant correlation between chronic IBS and subsequent development of microscopic colitis in patients with persistent low-grade inflammation undetectable via standard colonoscopy. The Rome IV criteria are outdated. If your doctor isn’t ordering calprotectin stool tests, they’re not doing their job. You deserve better than ‘it’s all in your head.’
Charles Lewis
November 19, 2025 AT 03:56It is worth noting that the gut-brain axis is not merely a metaphor but a neurophysiological pathway mediated by the vagus nerve, the enteric nervous system, and a complex interplay of cytokines, serotonin, and microbial metabolites. The efficacy of low-dose tricyclic antidepressants in IBS-M is not due to their antidepressant properties per se, but rather their antagonism of 5-HT3 and 5-HT4 receptors in the intestinal mucosa, which modulates visceral hypersensitivity and motility. Cognitive behavioral therapy, when delivered by trained clinicians using protocols validated by the American College of Gastroenterology, demonstrates neuroplastic changes in the anterior cingulate cortex and insula-regions implicated in pain processing and interoceptive awareness. Therefore, the integration of pharmacological, dietary, and psychological interventions is not merely a ‘plan’-it is a systems-based approach grounded in contemporary neurogastroenterology. One must not underestimate the power of consistent, evidence-informed self-management.
Renee Ruth
November 20, 2025 AT 12:00they’re all lying. i’ve been on every diet, every pill, every ‘therapy.’ i’ve cried in public bathrooms so many times i’ve lost count. i’ve lost jobs, relationships, friends. they say ‘you’re not alone’-but no one gets it. no one. they just throw FODMAPs and peppermint oil at you like it’s a magic spell. i’ve been told i’m ‘too emotional.’ guess what? my gut is screaming, and no one’s listening. i’m not just ‘managing’-i’m surviving. and the fact that they’re still selling this as ‘manageable’? it’s cruel. someone needs to expose this system.