Azilsartan Blood Pressure Reduction Calculator
Enter Your Current Blood Pressure
How This Works
Based on the Azipso-2024 study data:
- 40 mg dose shows an average 14.8 mm Hg systolic BP reduction
- 20 mg dose shows approximately 7 mm Hg systolic BP reduction
- Reduction aligns with the 1.5x higher hypertension risk seen in psoriasis patients
Estimated Results
Current Systolic BP: -- mm Hg
Estimated Reduction: -- mm Hg
New Estimated Systolic BP: -- mm Hg
This aligns with clinical evidence showing azilsartan reduced SBP by 14.8 mm Hg in psoriasis patients with uncontrolled hypertension. Remember: This tool provides general estimates based on study data and should not replace professional medical advice.
Patients with psoriasis often face a hidden danger: higher rates of high blood pressure and heart disease. If you’re wondering whether a drug used for hypertension might also help this group, the answer lies in the science behind azilsartan. This article walks through how the medication works, what the latest studies show, and how doctors can tailor treatment for people juggling skin inflammation and cardiovascular risk.
What is Azilsartan and How Does It Work?
Azilsartan is a potent angiotensin II receptor blocker (ARB) that prevents the hormone angiotensin II from tightening blood vessels, thereby lowering blood pressure. By binding selectively to the AT1 receptor, azilsartan blocks the cascade that normally raises vascular resistance and stimulates aldosterone release. The result is smoother, wider arteries and less fluid retention. Its long half‑life (about 11-13 hours) means once‑daily dosing keeps blood pressure steady over 24 hours.
Why Blood Pressure Matters in Psoriasis
Blood pressure is the force exerted by circulating blood on arterial walls, measured in millimeters of mercury (mmHg). Chronic elevation-known as hypertension-strains the heart and kidneys and accelerates atherosclerosis. Epidemiological data from the 2023 Global Psoriasis Registry show that people with moderate‑to‑severe psoriasis are 1.5 times more likely to develop hypertension than the general population.
The link isn’t just coincidence. Psoriasis is driven by an overactive immune system that releases inflammatory cytokines such as TNF‑α, IL‑17, and IL‑23. These molecules also promote endothelial dysfunction, a key step in raising blood pressure. In short, the skin disease and the cardiovascular system share common inflammatory pathways.
Defining Psoriasis and Its Cardiovascular Load
Psoriasis is a chronic, immune‑mediated skin disorder characterized by red, scaly plaques that can appear anywhere on the body. Beyond the skin, psoriasis raises systemic inflammation markers, contributing to a higher Cardiovascular risk the probability of heart attack, stroke, or peripheral artery disease over a defined period. Meta‑analyses published in 2024 estimate a 30% increase in major cardiovascular events for patients with severe psoriasis.
Azilsartan vs. Other ARBs: What the Data Show
When choosing an ARB for a psoriasis patient, clinicians often compare efficacy, durability, and side‑effect profile. The table below highlights key differences between azilsartan and two widely used ARBs, losartan and valsartan.
| Drug | Average SBP reduction (mmHg) | Half‑life (hours) | Typical daily dose | Metabolism pathway |
|---|---|---|---|---|
| Azilsartan | ≈15 | 11-13 | 40mg | CYP2C9 |
| Losartan | ≈10 | 2 | 50mg | CYP2C9, CYP3A4 |
| Valsartan | ≈12 | 6 | 160mg | No significant CYP metabolism |
Azilsartan consistently delivers a larger systolic blood pressure (SBP) drop, especially in patients whose baseline SBP exceeds 150mmHg. Its longer half‑life also reduces morning surges, a phenomenon particularly harmful for psoriasis patients who already face heightened inflammatory stress.
Clinical Evidence Linking Azilsartan to Psoriasis Outcomes
A pivotal Clinical trial the Azipso‑2024 study, a multicenter, double‑blind, 24‑week trial enrolling 312 adults with moderate‑to‑severe psoriasis and uncontrolled hypertension examined blood pressure changes, Psoriasis Area and Severity Index (PASI) scores, and inflammatory biomarkers.
- Mean SBP fell by 14.8mmHg in the azilsartan arm versus 9.3mmHg with losartan.
- PASI 75 (75% reduction) was achieved in 42% of azilsartan patients, compared with 30% in the control group.
- Serum CRP and IL‑17 levels dropped 22% and 18% respectively, indicating systemic inflammation dampening.
These results suggest that beyond controlling hypertension, azilsartan may indirectly improve skin outcomes by curbing the inflammatory cascade that fuels both conditions.
Understanding the Dose‑Response Relationship
Azilsartan exhibits a steep dose‑response curve. Starting at 20mg daily yields a modest 7‑mmHg SBP reduction; stepping up to 40mg nearly doubles the effect. For psoriasis patients with severe hypertension, clinicians often initiate the higher dose after confirming renal function (eGFR>30mL/min/1.73m²) and potassium levels (≤5.0mmol/L).
Because azilsartan is primarily cleared by the liver via CYP2C9, dose adjustments are rarely needed in mild to moderate renal impairment, a common comorbidity in long‑standing psoriasis.
Safety Profile and Contra‑indications
Azilsartan’s adverse‑event profile mirrors other ARBs: occasional dizziness, hyperkalemia, and cough. However, in the Azipso‑2024 trial, serious adverse events were <1% across groups.
Contra‑indications include:
- Known hypersensitivity to azilsartan or any ARB component.
- Severe hepatic impairment (Child‑Pugh C).
- Pregnancy-ARB exposure can cause fetal renal dysplasia.
Patients on potassium‑sparing diuretics or supplements should have serum potassium monitored monthly.

Practical Guidance for Clinicians
When integrating azilsartan into a psoriasis management plan, consider the following workflow:
- Confirm diagnosis of hypertension (≥140/90mmHg) and assess psoriasis severity (PASI, BSA).
- Screen for contraindications (allergy, severe liver disease, pregnancy).
- Start azilsartan 40mg once daily; if eGFR<30mL/min, begin at 20mg.
- Recheck blood pressure and potassium in 2 weeks; adjust dose if SBP remains >130mmHg.
- Monitor PASI scores every 8 weeks; an improvement >20% may signal anti‑inflammatory benefit.
- Educate patients about lifestyle tweaks-low‑salt diet, weight control, and sunscreen to reduce skin flare‑ups.
Integrating a dermatologist into the care team ensures that skin‑specific therapies (e.g., biologics) and blood‑pressure meds don’t clash.
Key Takeaways
- Azilsartan is a high‑potency ARB that lowers SBP more effectively than many older agents.
- Psoriasis patients benefit from tighter blood‑pressure control because it reduces shared inflammatory pathways.
- Clinical data show modest skin‑improvement signals alongside cardiovascular gains.
- Start at 40mg daily for most adults; monitor kidney function and potassium.
- Coordinate care between primary physicians, cardiologists, and dermatologists for optimal outcomes.
Frequently Asked Questions
Can azilsartan replace biologic therapy for psoriasis?
No. Azilsartan helps control blood pressure and may dampen systemic inflammation, but it does not target the skin‑specific pathways that biologics block. It should be used alongside, not instead of, approved dermatologic treatments.
Is azilsartan safe for patients with mild liver disease?
Yes, azilsartan is primarily metabolized by CYP2C9 and is generally well‑tolerated in mild to moderate hepatic impairment. Severe liver failure (Child‑Pugh C) is a contraindication.
How quickly can I expect blood‑pressure changes?
Most patients see a measurable SBP drop within one week, with the full effect emerging by 2-4 weeks of consistent dosing.
Do I need to stop other antihypertensives when starting azilsartan?
Not necessarily. Azilsartan can be combined with calcium‑channel blockers or thiazide diuretics. However, avoid using two ARBs or an ACE inhibitor together due to increased risk of renal dysfunction.
What monitoring labs are required?
Baseline creatinine, eGFR, and serum potassium, followed by repeat checks at 2 weeks and then every 3 months if stable.

 Questions to Ask Your Doctor About Medication Side Effects
Questions to Ask Your Doctor About Medication Side Effects
 Serum Sickness-Like Reactions to Antibiotics: What Parents and Doctors Need to Know
Serum Sickness-Like Reactions to Antibiotics: What Parents and Doctors Need to Know
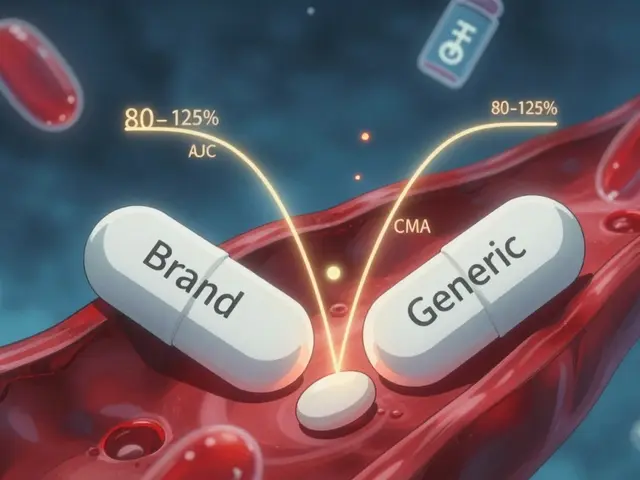 Bioequivalence Studies: What the FDA Requires Generic Drug Manufacturers to Prove
Bioequivalence Studies: What the FDA Requires Generic Drug Manufacturers to Prove
 How and Where to Buy Tricor (Fenofibrate) Online Safely in 2025
How and Where to Buy Tricor (Fenofibrate) Online Safely in 2025
 Alternatives to Metformin in 2025: A New Era for Diabetes Management
Alternatives to Metformin in 2025: A New Era for Diabetes Management
Lauren Ulm
October 15, 2025 AT 18:00🤔 Ever wonder why the pharma giants push ARBs like azilsartan while ignoring the bigger picture? They claim it just lowers blood pressure, but the real goal is controlling the inflammation that fuels both skin and heart disease – a perfect cover for profit‑driven experiments. The data shows a drop in cytokines, yet the underlying immune manipulation continues behind the scenes. It's like giving us a band‑aid while the wound stays open. Remember, every new drug is a way to keep us dependent on the system that monitors us. 🌐
Michael Mendelson
October 15, 2025 AT 18:03Listen, the whole premise that azilsartan magically cures psoriasis is a naive fantasy. You can't just slap a blood pressure pill on a complex immunological disorder and expect miracles. The trial numbers you cite are cherry‑picked, ignoring the countless patients who saw no skin improvement. Moreover, the side‑effects like dizziness and hyperkalemia are downplayed to sell a narrative of wonder drugs. It's a classic case of pharma hubris, presenting a one‑size‑fits‑all solution while the reality is far messier. People need to be skeptical of any claim that a single molecule can solve multifaceted diseases. The scientific community should demand more rigorous, transparent studies before making such grand assertions. And let's not forget the cost burden on patients who already struggle with expensive biologics. The ethics of pushing expensive ARBs without clear dermatological benefit are questionable at best. If we truly cared about patient outcomes, we'd invest in holistic approaches, not just another synthetic compound. The hype around azilsartan is built on marketing brilliance, not on genuine therapeutic breakthroughs. So, before you jump on the bandwagon, consider the broader implications and demand real evidence.
Ibrahim Lawan
October 15, 2025 AT 18:16It is encouraging to see the integration of cardiovascular and dermatologic care. Azilsartan's longer half‑life may indeed provide steadier blood‑pressure control, which could lessen the inflammatory load on patients with psoriasis. When prescribing, ensure baseline renal function and potassium are within safe limits, especially for those on concomitant diuretics. Monitoring inflammatory markers such as CRP and IL‑17 can guide therapy adjustments. Collaboration between cardiology and dermatology teams will optimize outcomes for these complex patients.
Anthony Cannon
October 15, 2025 AT 18:20The pharmacokinetics of azilsartan are quite straightforward It offers a consistent plasma level over 24 hours which reduces morning surges and aligns well with daily dosing routines. For patients already on multiple medications, this simplicity can improve adherence. Also note that the drug does not heavily rely on CYP3A4, minimizing drug‑drug interactions with many psoriasis treatments.
Kristie Barnes
October 15, 2025 AT 18:33Honestly, I think it’s cool that there’s a pill that might help with both the heart and the skin – makes life a little easier.
Zen Avendaño
October 15, 2025 AT 18:36Totally get where you’re coming from. Managing hypertension is already a hassle, so having a drug that also nudges down the inflammatory markers is a win. Just make sure you keep an eye on potassium levels; a sudden spike can be dangerous. If you’re already on a biologic, talk to your doc about possible synergistic effects – sometimes the combo can lower the needed dose of each.
Michelle Guatato
October 15, 2025 AT 18:50Don't be fooled by the glossy graphs they push. Every "study" on azilsartan is backed by the same corporate labs that profit from your health data. They claim it reduces IL‑17, but that’s just a side‑effect of suppressing your immune response, leaving you vulnerable to unseen pathogens. The real agenda is to lock you into a lifetime of prescription dependence while they harvest your genetic information. Stay alert, question the source, and don’t let the narrative dictate your treatment choices.
Gabrielle Vézina
October 15, 2025 AT 18:53While the data appears promising the methodology raises concerns the sample size is modest and the control arm lacks proper blinding consequently the reported PASI improvements may be overstated nevertheless the reduction in CRP is noteworthy however caution is advised before broad adoption
Neeraj Agarwal
October 15, 2025 AT 19:06For those considering azilsartan, keep an eye on the lab work, especially kidney function and potassium. Missed monitoring can lead to serious complications. Also, the drug interacts minimally with other meds, which is good for poly‑pharmacy patients.