The Science Behind Ovulation: How Your Hormones Set the Stage
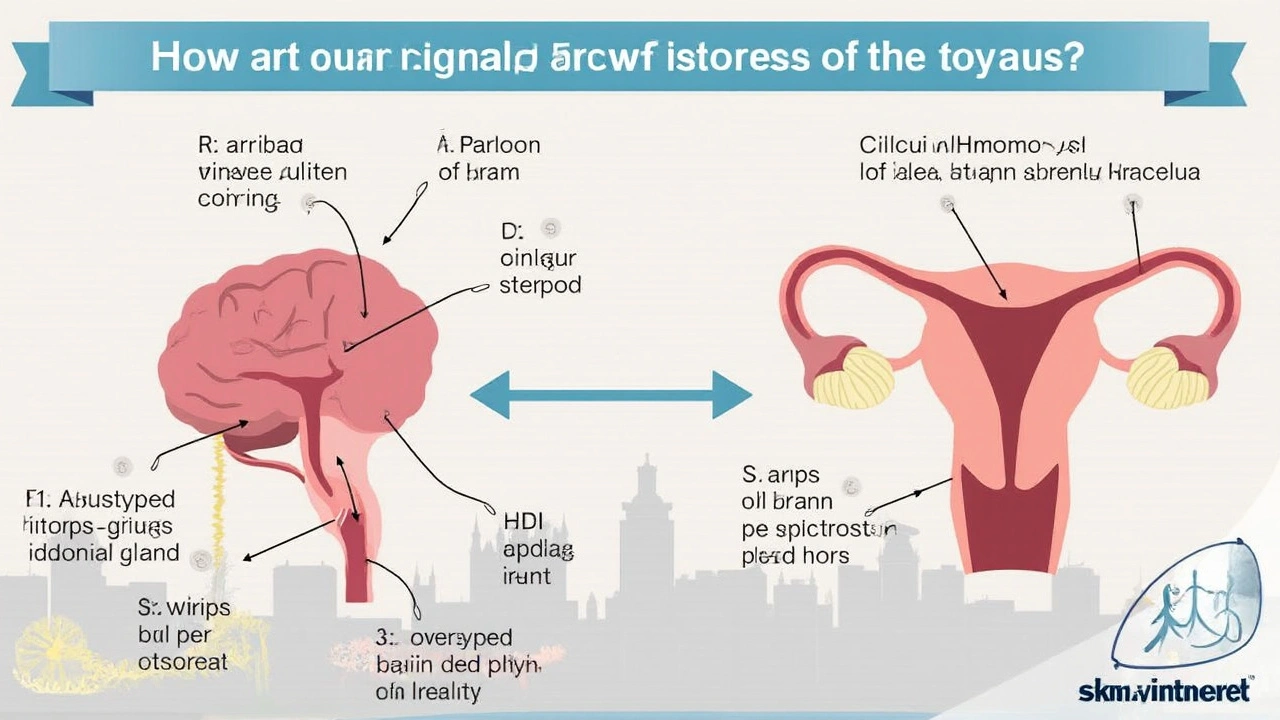
It’s hard to appreciate just how much choreography goes into ovulation until you start untangling the messy tangle of hormones behind it. Picture the brain and ovaries like friends sharing secrets over a text chain—except instead of emojis, they’re using chemical messengers. For ovulation to even have a shot at happening, your hypothalamus (located in your brain) kicks things off by releasing pulses of gonadotropin-releasing hormone (GnRH). This might sound straight out of a textbook, but if those pulses glitch—too fast, too slow, too erratic—? The rest of the chain falls apart, and so does your shot at pregnancy.
Once GnRH gets things moving, your pituitary gland (another important player in the brain) steps up and shoots out two hormones: follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH nudges the ovaries to mature a group of follicles, and inside one lucky follicle, there’s an egg primed for release. The LH surge is like a last call—within 24-36 hours, the ripest egg makes its escape from the ovary, hoping to meet a sperm cell with excellent navigation skills. Of course, if these hormone signals get lost, muted, or just come at the wrong time, ovulation never happens or goes awry. If you’re reading this after months (or years) of frustration, you’ve probably realized how finicky this system is.
Now, what can throw these pathways off? Sometimes, high stress, being underweight or overweight, polycystic ovary syndrome (PCOS), premature ovarian failure, or thyroid imbalances jam the signal at different points. In fact, PCOS alone is behind around three out of every four cases of anovulation in people seeing fertility doctors. So, if your cycles are unpredictable, ovulation induction doctors will make it a game of detective work—blood tests, ultrasounds, even charting your symptoms. The beauty (and curse) of modern medicine is just how precisely these hormones can be measured and tinkered with, which brings us to why ovulation induction is both an art and a science.
Even if you’re tracking ovulation at home with test strips, remember these only pick up the LH surge—not the whole story. Sometimes you’ll see that surge, but the follicle doesn’t release an egg. Other times, the ovary’s response to all the hormonal cues is too weak or too chaotic. This is why doctors take a deeper look at the hormone ballet behind the scenes. Sometimes, a single pill or injection can push things back into rhythm, but it takes trial and error and regular monitoring. Don’t be surprised if you need a cycle or two (or three) before you hit a sweet spot, because even textbook hormone levels don’t guarantee perfect ovulation every time.
Popular Drug Classes for Ovulation Induction
When you first walk into a fertility clinic and start talking about ovulation induction, you’ll hear a parade of medication names that sound more like a chemistry midterm than a road to parenthood. But each drug, believe it or not, has its own personality and trick for helping you ovulate. Let’s break down the biggest hitters:
Clomiphene Citrate (Clomid) gets top billing for a reason—it’s cheap, easy to take, and has decades of proof behind it. It acts by blocking estrogen receptors in your brain, tricking it into sending out more FSH and LH. Think of it as a gentle nudge to the system, often prescribed for people with PCOS or unexplained infertility. Side effects? Hot flashes, mood swings, and sometimes the lining of your uterus doesn’t build up as nicely as you’d want. Success rates hover around 25-30% per cycle, but most doctors only want you taking it for about 6 cycles, max.
When Clomid isn’t working or if you get too many side effects, there’s Letrozole (Femara). Originally made for breast cancer, doctors noticed it’s actually even better at making some women ovulate—especially with PCOS. The upsides? Fewer hot flashes, a more natural endometrial lining, and a slightly higher success rate for live births in some studies. You still need to watch out for multiple pregnancies—twins happen more often on any ovulation induction drug.
If oral medications flop, next up are the injectable gonadotropins (FSH and sometimes LH directly). These are the big guns: you inject yourself daily, your ovaries get flooded with hormones, and you need ultrasounds every few days to avoid overstimulation or dangerous side effects like ovarian hyperstimulation syndrome (OHSS). Is it powerful? Absolutely. But it’s more expensive, riskier, and usually reserved for when simpler options fail or you’re prepping for IVF.
For people with rare hormonal issues or irregular brain-to-ovary signaling (like hypogonadotropic hypogonadism), pulsed GnRH therapy mimics what your brain should do naturally, solved with a little pump device. And in special cases related to high prolactin levels (which shut down ovulation), your doctor might reach for a drug like cabergoline to bring things back to normal.
If you’re curious about choices beyond the go-to prescriptions, check out this helpful roundup of alternative to Clomid options. You’ll find some surprising strategies for those looking to optimize chances or who don’t mesh with first-line drugs.
Something that tends to worry every couple: does this mean I’ll have quadruplets? Not really. The risk of higher order multiples with pills like Clomid or letrozole is about 1%. With injectables, the risk jumps (which is why monitoring is non-negotiable). Your doctor’s goal is always one healthy baby—but sometimes, the ovaries miss the memo and mature too many eggs!
How Success Rates Stack Up: What the Numbers Really Mean
There’s a lot of myth-making around fertility treatment numbers. The truth? Nothing guarantees a positive pregnancy test, but well-chosen ovulation induction therapy can make a huge difference. After all, if you’re not releasing an egg each month, chances of conception drop to basically zero—so even a single month of reliable ovulation is a huge win.
For couples dealing with anovulatory infertility (meaning you’re not ovulating at all), the odds improve nicely once treatment starts. For example, people with PCOS have around a 15-25% chance of pregnancy per cycle using letrozole or Clomid. Over the course of six cycles, about 80% will see ovulation, and around half may get pregnant. Of course, those numbers drop if there are extra fertility hurdles—like low sperm count, tubal problems, or older age. No two cases are the same, but ovulation induction can at least double or triple a couple’s monthly chance compared to going unmedicated.
If you need to move up to injectable gonadotropins, the per-cycle pregnancy rates rise to about 20-25% (again, highly dependent on your underlying health). But these drugs are pricier, require more intensive monitoring, and come with a higher chance of twins or triplets. It’s always a balancing act—a little too much stimulation, and suddenly you’re facing tough decisions about selective reduction or pregnancy risks.
Curious if success rates change based on diagnosis? Here’s a handy table summarizing rough numbers based on condition and drug class:
| Diagnosis | Drug | Ovulation Rate | Pregnancy Rate per Cycle |
|---|---|---|---|
| PCOS | Letrozole | 80-90% | 15-25% |
| PCOS | Clomid | 70-85% | 10-20% |
| Unexplained | Clomid | 60-80% | 8-15% |
| Hypogonadotropic Hypogonadism | GnRH therapy | 90%+ | 20-25% |
| Any | Injectables | 90%+ | 15-25% |
If none of this is working, don’t get discouraged. Sometimes adding treatments (like metformin in women with PCOS, or insemination for mild male factor infertility) boosts the odds again. Even then, about 10-15% of couples need to move on to IVF for best results. The journey isn’t linear—but the science shows that persistence and adjusting treatment can open up new opportunities.
One thing that rarely gets mentioned: success doesn’t always look like a baby on the first try. Sometimes it’s about confirming ovulation is happening, giving your body a fighting chance, or even just restoring more regular cycles. And yes, stress is a factor—a 2022 U.S. survey found about 80% of couples find the unpredictability of fertility meds the most emotionally draining part of treatment. If you need to take breaks, talk with your doctor honestly. The right pace matters as much as the right medication.
Tips, Troubleshooting, and What to Expect Going Forward
If you’re thinking about starting ovulation induction, you probably want concrete tips and a clear sense of what actually happens month to month. It’s not a walk in the park, but you can stack the deck in your favor by knowing what to expect—and how to handle the curveballs.
- Timing your medication: Most oral drugs (like Clomid, letrozole) are taken early in your cycle—usually days 3-7 or 5-9 after your period starts. Make sure you mark your calendar and stick to it. Forgetting or skipping a dose can throw off your whole ovulation window.
- Monitoring is your friend: Don’t get annoyed by all the ultrasounds and bloodwork. These track your follicle growth, hormone surge, and lower the risk of multiples or OHSS. If you’re using injectables, monitoring isn’t optional—it’s standard practice for safety.
- Track your symptoms: Your body often sends signals too. Ovulation predictor kits, basal body temperature charts, and even changes in cervical mucus all help confirm ovulation is actually happening.
- Mood swings are common: A lot of the meds tinker with your estrogen, and that can mess with your mood, sleep, and even your appetite. Don’t be too hard on yourself—and let your partner in on the ride. My spouse, Margot, once joked that tracking cycles is basically a cross between detective work and a reality TV challenge.
- Know when to mix it up: If nothing’s happening after 3-6 cycles (or you’re getting frustrating side effects), talk to your doctor about changing drugs, adding adjuvant therapies, or switching to a different ovulation induction plan.
- Don’t ignore the sperm factor: Every couple is different, but sometimes male fertility issues are quietly sabotaging your odds. Basic semen analysis takes the guesswork out of it.
One surprising fact: Lifestyle tweaks matter. Studies have shown that losing just 5-10% of body weight in people with PCOS can restore ovulation in up to half of patients. Managing insulin resistance, quitting smoking, and limiting caffeine also help hormonal balance. Even small improvements—more sleep, better nutrition, reduced alcohol—give therapies the best shot at working.
Fertility journeys can run longer than you’d expect. Some couples get results on the first cycle, while others need several tries, dose adjustments, or a shift to IVF. Stay open to pivoting, and line up emotional support along the way—friends, counselors, or online groups. Treatment can feel isolating, but your experience and questions are valid. If you’re feeling stuck, ask your doctor if it’s time to run more tests or adapt the plan. Information, flexibility, and stamina are your best tools.
Just remember: Ovulation induction medicine has come a long way since the early days. With a smart combination of meds, regular monitoring, and steady support, you have real options to boost your chances of success. If you feel like something’s missing, don’t be afraid to explore new treatments or look into an alternative to Clomid that fits your unique situation.

 Compare Rhinocort (Budesonide) with Alternatives: What Works Best for Nasal Allergies?
Compare Rhinocort (Budesonide) with Alternatives: What Works Best for Nasal Allergies?
 Childhood Obesity Prevention and Family-Based Treatment: What Works and Why
Childhood Obesity Prevention and Family-Based Treatment: What Works and Why
 Aspirin and Narcolepsy: Potential Benefits for Sleep Disorders
Aspirin and Narcolepsy: Potential Benefits for Sleep Disorders
 Feldene (Piroxicam) vs Topical NSAID Alternatives - Pros, Cons & Best Uses
Feldene (Piroxicam) vs Topical NSAID Alternatives - Pros, Cons & Best Uses
 Linagliptin & Diabetes Education: Why Staying Informed Matters
Linagliptin & Diabetes Education: Why Staying Informed Matters
Keli Richards
July 18, 2025 AT 11:25I appreciate this detailed overview on ovulation induction therapy. It's quite reassuring to see the science behind hormone pathways broken down simply without losing the essential complexity. Understanding the different drug classes is crucial for anyone considering this path, especially when all the medical jargon can be overwhelming.
One thing I found helpful is how the post touches on both the benefits and limitations of fertility meds, which really gives a balanced perspective. Often, patients tend to focus just on the success rates but knowing realistic expectations can save a lot of mental stress. I wonder if anyone here has personal experiences with alternative medications to Clomid? It’d be great to hear what worked or didn’t, especially with current evidence-based guidance.
Ravikumar Padala
July 19, 2025 AT 15:28Honestly, I found the entire discussion about hormonal tweaks and drug classifications quite elaborate. I appreciate the depth, however, sometimes it felt dense and could be a bit exhausting to process in one go. The extensive explanation about the pathways was informative, but I wish it came with some visual aids or summaries to help with retention.
That said, the focus on realistic success rates is essential. We, as readers and hopeful patients, need to be grounded in facts rather than just hopeful promises. I am curious, though, about the side effects mentioned subtly. Could someone elaborate on how severe they might be compared to the benefits?
John Keough
July 20, 2025 AT 19:31This post strikes a good balance between science and accessibility. I like how it highlights the quest for alternatives to Clomid; it's something many fertility patients consider since not everyone responds well to it. The hormone pathways section gave me new insights on how these therapies work beyond just stimulation. It’s fascinating how targeted the drugs have become.
Does anyone know if the latest drugs mentioned here require less monitoring or fewer injections compared to older meds? That could be a big game-changer for patient comfort and compliance. Also, have there been any recent studies that update the success rates significantly?
Graham Smith
July 21, 2025 AT 23:35Good thoroughly written post overall, but could do with a bit more attention to detail regarding grammar and clarity in some sections. For example, using consistent punctuation throughout would make reading much smoother. Aside from these minor nitpicks, the content is solid and informative.
What piqued my curiosity was the mention of 'top fertility medications' without clearly listing which ones besides Clomid. Including a specific list or chart might have been beneficial. Despite that, I appreciate the well-demonstrated understanding of hormonal mechanisms involved in ovulation induction.
Jeremiah Morgan
July 23, 2025 AT 03:38This is a very encouraging and well-explained guide. As someone who has supported friends through fertility struggles, I know how confusing and stressful these options can be. The realistic success rates and the pros and cons of medications like Clomid help set honest expectations, which is very important psychologically.
Additionally, the mention of hormonal tweaks at play provides a crucial perspective on why a one-size-fits-all approach doesn’t work. Each patient’s hormone profile and reaction are unique, so personalized care remains key. I hope more clinics adopt the nuanced approach outlined here.
nina greer
July 24, 2025 AT 07:41The article addresses the topic authoritatively, although I find the treatment alternatives to Clomid deserved more rigorous examination. The depth of pharmacology is merely scratched. For readers who desire factual precision and less anecdotal fluff, more references with clinical trial data would elevate this guide from moderate to excellent.
Montague Tilmen
July 25, 2025 AT 11:45Why is Clomid even still suggested as a first line when newer, better options exist? This guide is polite but doesn’t really challenge the outdated reliance on old drugs. The so-called 'hormonal tweaks' are barely a patch on the fundamental antagonism to effective treatment. If medical professionals want true progress, they need to stop clinging to relics and embrace the evolution of fertility medicine more aggressively!
Also, the success rates cited seem overly generous. From what I’ve seen, many patients are left in limbo with repeated failures. This therapy sounds like it’s been marketed more than truly elevated.
Clarise Wheller
July 26, 2025 AT 15:48This post really captures the essence of what people going through infertility issues need — clear info grounded in science yet accessible enough to not feel intimidating. The balanced discussion of medication effects and hormone pathways makes it easier to digest and trust the recommendations.
I also appreciate the focus on alternatives to Clomid, as many people hear that name but don’t really know what else is out there. It’d be nice if the author shared some patient-friendly resources or support groups that align with this updated knowledge base.
Riley Fox
July 27, 2025 AT 19:51Ah, the eternal dance with hormones — a veritable ballet of chemicals and receptors! 🌹 The post captures the complexity but also the beauty of ovulation induction. Yet, I must ask, what of the psychological ramifications that often swim just under the surface of these medical interventions? Let us not forget that beyond the science exists a human soul wrestling with hope and despair alike.
Furthermore, one might wonder if the 'realistic success rates' allude truly to the bounded potential of nature or simply the limitations imposed by our current pharmacopoeia. Either way, it is a fascinating symphony worth contemplating. Thoughts?
Vera REA
July 28, 2025 AT 23:55Such a well-written and carefully researched piece! I appreciate the grammatical precision and soothing tone throughout this guide. It makes the complex subject quite approachable for anyone, regardless of their scientific background.
One aspect that struck me was the explanation of hormone pathways — it's often glossed over elsewhere. Also, the consideration of limitations alongside benefits helps maintain a realistic view rather than overselling outcomes. Has anyone explored the long-term effects of these induction therapies beyond immediate success rates? Curious to hear if there's solid research on that.
John Moore
July 30, 2025 AT 03:58The post offers a hopeful yet pragmatic perspective, which is so necessary in the world of fertility treatments. I appreciate how it blends scientific detail with empathy, addressing the emotional toll alongside clinical facts. Such an approach can empower patients to make informed decisions with confidence rather than fear.
Would love to see more interactive content or community stories linked to this guide to build a stronger support network for those going through similar journeys. After all, knowledge paired with shared experience often makes the most meaningful difference.