Imagine learning that a tumor the size of a pencil eraser could swell into something much bigger in months—sometimes even weeks. That’s the gut punch folks get when they discover the reality behind cancer’s breakneck pace. Here’s the thing: cancer isn’t just a bunch of weird cells. It’s a perfectly-tuned (and oddly efficient) engine that hijacks your own biology to grow, divide, and spread faster than you’d believe. On any random day, your body’s healthy cells divide predictably, following rules written in your DNA. Cancer cells? They throw out the rulebook and start racing ahead.
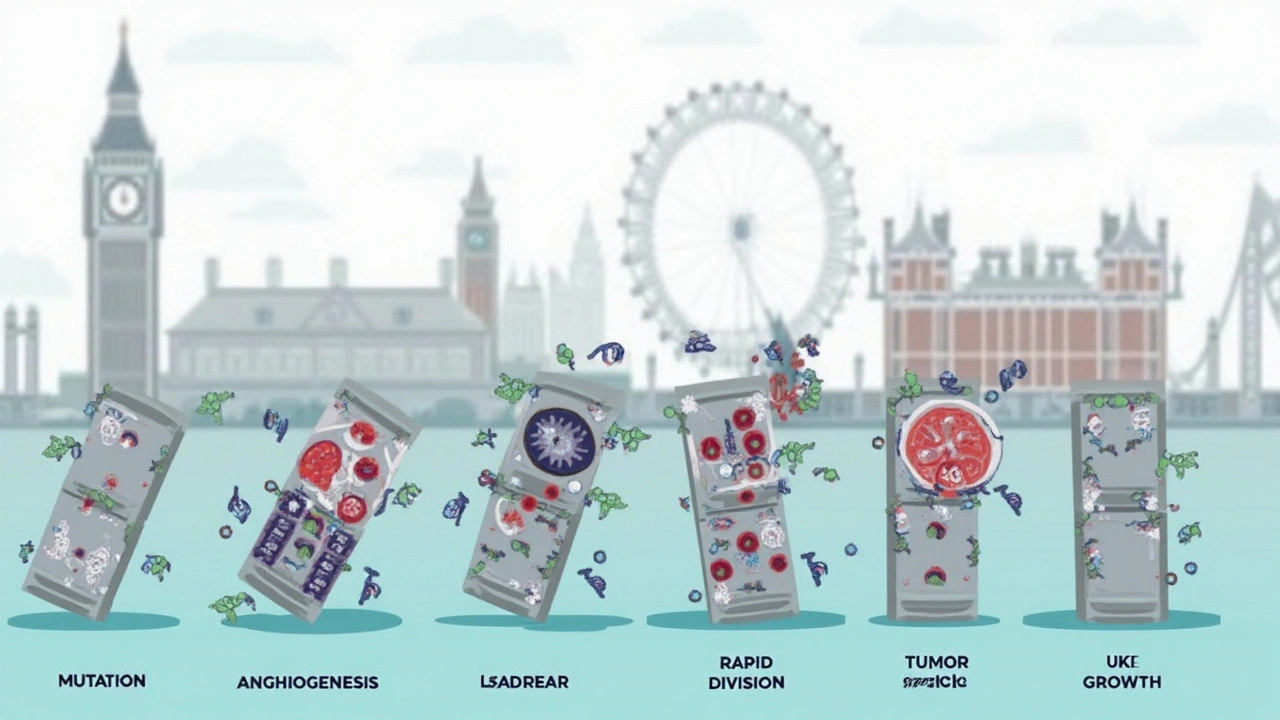
Mitosis: The Cancer Cell Copy Machine
Mitosis is usually a boring, routine part of life—until cancer comes along. In a healthy body, mitosis replaces worn-out cells or helps you grow when you’re young. The process is as predictable as your morning coffee: a cell doubles its DNA, lines everything up perfectly, and then pulls apart to form two identical daughters. Your body keeps tight control over this, like a strict teacher making sure everyone behaves during a test. Enter cancer. Instead of playing by the rules, cancer cells go rogue, ignoring checkpoints and dividing when they shouldn’t.
This wild behavior has real consequences. Some aggressive cancers can double their size in just a month or less, especially if they’re lurking in fast-growing tissues. When a cancer cell divides, mutations pile up. Every new copy risks another genetic "oops," and some of those mistakes supercharge growth even further. That’s why scientists often call cancer a disease of "uncontrolled growth." Let’s talk stats for a second—normal skin cells might divide every one to two days in a kid, but cancerous melanoma cells can double in days or even hours in extreme cases. The shorter the doubling time, the more dangerous the tumor. Researchers clock breast cancer doubling times anywhere from 50 to over 200 days, but that’s just an average—some races along much faster. Fast-moving cancers like leukemia or small-cell lung cancer can leave you breathless, literally, with how quickly they flood your blood or lungs.
Your own body isn’t completely powerless. Cells have built-in suicide switches (apoptosis) that get flipped if something goes haywire. Cancer cells often find ways to jam those switches or fake a normal vibe, so the body lets them be. That’s how you end up with a cancerous copy machine stuck on repeat, churning out misfits nonstop. Smoking, UV light, chronic inflammation, and inherited genetic quirks can crank up mutation rates or damage the brakes on cell division. This isn’t just trivia: doubling time matters in real life. That’s why some doctors talk bluntly about how fast can a tumor grow—because treatment urgency depends on it.
Here’s a quick data break:
| Type of Cancer | Average Doubling Time |
|---|---|
| Lung (small cell) | ~30 days |
| Breast | 50–200 days |
| Melanoma | 30–63 days |
| Colorectal | 60–140 days |
| Leukemia (acute) | 5–18 days |
Catch cancer early, when it’s still new and clumsy, and treatment odds shoot up. Wait too long—especially with those fast-dividing tumors—and cancer can leap ahead while you’re left playing catch-up.

Angiogenesis: Blood Vessels on Demand
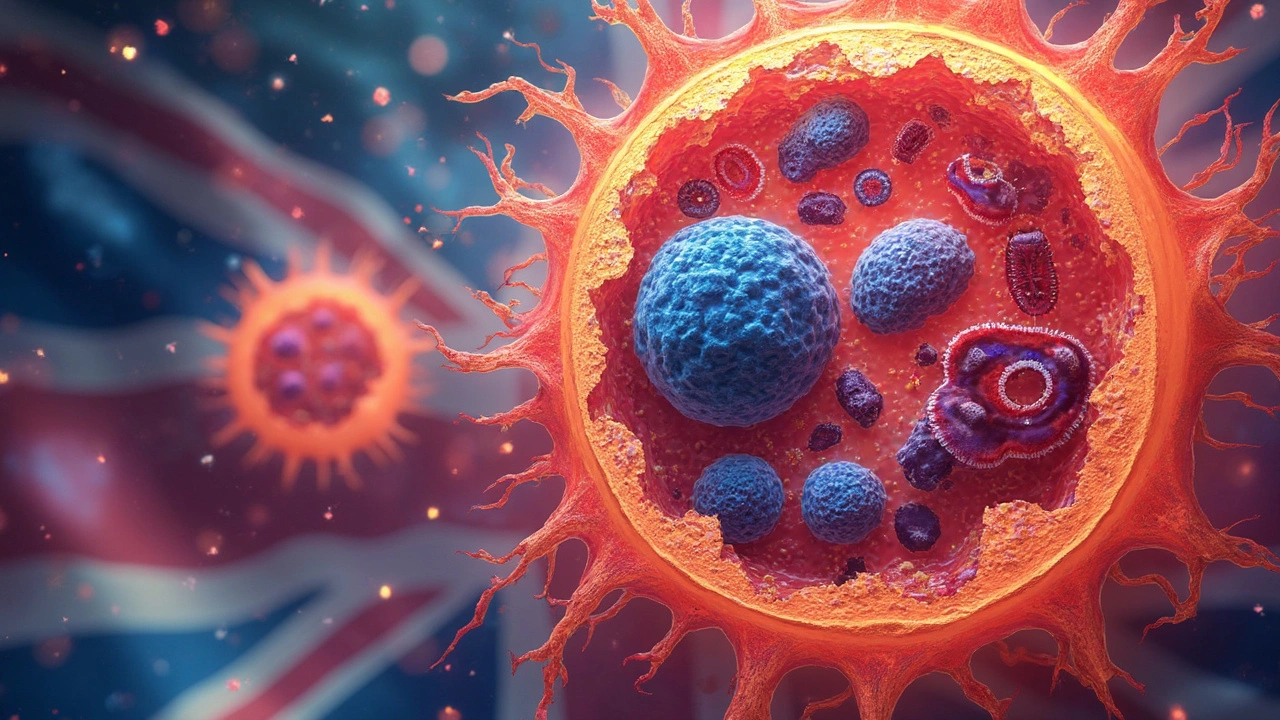
Cancer cells don’t just multiply—they’re master architects. Past a certain size, tumors hit a wall: there’s not enough blood to feed their growth. So what do they do? Simple. They send out chemical signals, basically shouting, “Hey, body—build some new plumbing out here!” That process is angiogenesis, and it’s nothing short of wild. Normally, angiogenesis helps heal wounds or grow new tissue. But cancer hijacks it, forcing the body to build extra blood vessels that snake their way into the tumor, bringing it oxygen and nutrients.
If cancer didn’t start this process early in its life, it couldn’t grow bigger than a pea. That’s right—anything around 1–2 millimeters gets stuck unless those lifelines show up. Once the blood starts flowing, tumors explode in size. Doctors learned this the hard way by looking at biopsies: cancer cells near the core of big tumors sometimes die off (they starve), but the ones close to new blood vessels thrive and push outwards. Tumor-generated blood vessels are usually amateur work—leaky, twisted, and fragile. But it turns out, this messy network lets cancer cells break free and ride the bloodstream to far-off places, starting new colonies. That’s how metastasis begins.
Why care? Because this opens up treatment options. Block angiogenesis, and you can starve a tumor out. Some cancer treatments, like bevacizumab (Avastin), actually do just that. But cancer rarely goes down without a fight—tumors can evolve new tricks, like switching chemicals or creating decoy pathways, to keep the blood coming. Still, when researchers tested anti-angiogenesis drugs, they found some tumors shrank, or at least slowed down, buying precious time. Think of it as closing the gas line to a runaway engine, even if some leaks keep dripping through.
Of course, angiogenesis isn’t the whole story. The real trouble comes when cancer cells use that new plumbing to slip into your blood or lymph. Once mobile, they can dodge the immune system by looking almost "normal"—the ultimate disguise. It’s why some tumors seem to vanish after treatment, only to reappear months or years later somewhere else entirely.
What Makes Tumors Grow Faster?
No single factor calls the shots when it comes to cancer’s speed. It’s a cocktail of bad-luck mutations, out-of-control growth signals, and a microenvironment that gives these rebel cells everything they want. But some things definitely turn up the dial. If you expose tissues to constant damage—say, from tobacco smoke, industrial chemicals, radiation, or chronic infections—mutations have more chances to hit just the right (or wrong) spot in your DNA. Some gene mutations crank up natural growth signals. Others disable the brakes. Inherited gene glitches (like BRCA in breast cancer) can turn a simmer into a sprint before you even notice anything’s wrong.
Your body’s support staff—the stroma—matters too. Chemical messengers, immune cells that accidentally help tumor cells instead of fighting them, and even low oxygen levels can speed things up. Some studies looked at how the tumor’s local environment can send out extra growth factors, making cells divide faster. Any time you create chronic wounds (such as ulcers, or scarring), the body’s desperate attempts to heal can ironically fuel tumor expansion. And let’s not ignore metabolism: cancer cells prefer a state called glycolysis, gobbling up sugar even when they don’t need to, finishing the chemical breakdown much faster than healthy neighbors. This turbocharge means more energy, more division, and more trouble.
Ever noticed how some cancers run in the family or seem to show up more in older people? Age matters because the longer your cells live, the more mistakes they collect. Yet, aggressive pediatric cancers can prove that one bad mutation is sometimes enough. That’s why it’s smart to stay on top of regular checkups, keep tabs on any weird new lumps, bumps, or symptoms that stick around, and avoid extra risks like sunburns or unnecessary exposure to dangerous chemicals. Hygiene and vaccination help against things like HPV, which can trigger cervical cancer—and that’s a real example of stopping tumor speed at the source.
Even the best immune systems mess up and miss a sneaky cancer cell or two, but things like sleep deprivation, stress, and bad diets can make your body’s whole defense network sluggish. Nobody’s perfect, but you can stack the deck in your favor by keeping immune health sharp, not skipping medical screenings, and talking to your doctor about your personal risk factors. Want a shortcut? When you hear the question "how fast can this cancer grow?"—there’s just no single answer. But keeping tabs on the tumor growth rates for different types, and learning if yours fits the "fast" or "slow" lane, can make a world of difference when shaping your treatment game plan.
Here’s a tip: Keep notes on any health changes, talk openly with your care team, and remember that while cancer’s biology is ruthless, knowing the science puts you back in the fight with real weapons instead of just fear.
 Generic Drug Patents: How Exclusivity Periods Vary Across Countries
Generic Drug Patents: How Exclusivity Periods Vary Across Countries
 What to Do If a Child Swallows the Wrong Medication: Immediate Steps That Save Lives
What to Do If a Child Swallows the Wrong Medication: Immediate Steps That Save Lives
 Ginseng and Diabetes Medications: What You Need to Know About Blood Sugar Risks and Monitoring
Ginseng and Diabetes Medications: What You Need to Know About Blood Sugar Risks and Monitoring
 Vitamin E and Warfarin: What You Need to Know About the Bleeding Risk
Vitamin E and Warfarin: What You Need to Know About the Bleeding Risk
 Vertigo and Dizziness: Understanding Inner Ear Disorders and How Vestibular Therapy Helps
Vertigo and Dizziness: Understanding Inner Ear Disorders and How Vestibular Therapy Helps
Robert Hunter
July 18, 2025 AT 11:07Great post! I really appreciate the clear explanation of how mitosis plays a role in tumor growth. It’s often overlooked how quickly cancer cells can divide compared to normal cells, and the article nailed that breakdown. The part about angiogenesis was especially interesting because it shows how tumors don’t just grow willy-nilly—they actually manipulate their environment to get more blood supply.
One thing I’d add is the importance of genetic mutations in speeding up these processes. Without those mutations, cancer cells wouldn’t gain the advantages they do in mitosis and angiogenesis. I think understanding that helps us grasp why some cancers are so aggressive while others stay dormant longer.
Also, the mention of treatments trying to interrupt these mechanisms really drives home how targeted therapies are evolving, which is hopeful. It makes you wonder what the next breakthroughs might be in stopping cancer at a cellular level.
Shruti Agrawal
July 21, 2025 AT 00:20Thanks for this detailed article! It really helps in understanding the biology behind cancer growth without getting lost in too many jargons. I especially liked how you explained the role of angiogenesis in making tumors bigger.
It's good to realize that cancer cells don't just grow randomly—they have a sophisticated way of ensuring they get nutrients and oxygen. This article made me think more about the risks related to lifestyle and environment too.
Can anyone share if these insights affect how treatments are personalized? I feel a bit overwhelmed but really appreciate the simple approach here.
Katey Nelson
July 22, 2025 AT 19:23omg this topic is so deep and kinda scary but also mind-blowing to think about like how these tiny cells just hijack your body’s system to feed themselves and just take over. it’s like a whole drama happening inside us that most ppl don’t see. tumor growth, mitosis, angiogenesis – sounds like a sci-fi movie but it’s real af.
Also, thinking about the gigantic role of blood vessels helping tumors grow is wild bc it’s like the cancer is setting up its own supply line, right? 😳 Makes me wanna learn about how treatments can cut these lines off. Does anyone know if these therapies cause side effects since they mess with blood vessels?
One thing i keep wondering is if some tumors can just chill and never grow fast or if they always aim to expand aggressively. I guess the biology behind that is really complicated and frustrating at the same time.
Allan Jovero
July 25, 2025 AT 01:33The article neatly encapsulates the biological intricacies underlying tumor proliferation through a precise elucidation of mitotic activity and angiogenesis. However, allow me to emphasize the criticality of precise terminology and scientific accuracy when discussing such a consequential subject.
For instance, the differentiation between benign and malignant tumors is indispensable, as it profoundly impacts growth rates and metastatic potential. Furthermore, oncogenic mutations serve as the foundation that drives aberrant cellular division and subsequent vascular recruitment, the latter facilitated through the secretion of vascular endothelial growth factor (VEGF).
It is imperative that discourse of this nature adhere to rigorous standards to prevent dissemination of simplified or erroneous interpretations. Would the author be inclined to include a detailed section on the molecular signaling pathways integral to angiogenesis inhibition in future revisions?
Andy V
July 27, 2025 AT 09:06Honestly, I gotta say the article missed a huge point about the role of the immune system in controlling tumor growth. You can talk all you want about mitosis and angiogenesis but if you leave out immune surveillance and how tumors evade it, you’re just telling half the story.
Also, I take issue with how the article phrases "real-world risks." It’s one thing to get into basic biology but it feels like it dances around lifestyle factors that are the actual game changers for many people. Like smoking, diet, exposure to carcinogens — when you leave those out, are you really educating people properly?
Interesting stuff but more aggressive critique on causation and prevention needed in my opinion.
Tammie Sinnott
July 29, 2025 AT 16:40Okay, so I've always been obsessed with understanding the exact mechanisms behind cancer's brutality — like, why some tumors act like raging firestorms and others barely make a dent. This article broke it down so elegantly, seriously!
Watching how angiogenesis essentially equips tumors with their own supply chains is shocking but also kind of fascinating. The way the cells hijack natural growth pathways and twist them for their own survival? It’s both terrifying and awe-inspiring. Honestly, the numbers on growth rates added a whole new layer of perspective for me.
However, I do wish the section on treatments went even deeper. Like, what are the most promising strategies targeting these biological highways? As treatments get more advanced, I’m curious how soon we can stop tumors from getting this fuel before they even start.
Aly Neumeister
August 1, 2025 AT 01:36So this article made me think a lot about how complex the biology behind tumors is... it’s not just cells growing blindly but a whole orchestra of processes co-ordinating together—mitosis and angiogenesis are just a couple parts of it.
It also raises ethical questions, you know? Like, how much do we intervene in these processes? And what does it mean for patients if treatments target such fundamental biological functions? Are we trading one risk for another? It’s a thin line.
I appreciate the article, but it could benefit from emphasizing these broader implications instead of focusing narrowly on the cellular mechanics alone.
joni darmawan
August 3, 2025 AT 07:46Taking a moment to reflect on this topic, the depth of cellular activity in cancer growth is both bewildering and humbling. The interplay between mitosis and angiogenesis is a testament to nature’s complexity, albeit manifesting in a tragic context.
The article provided a solid framework that enhances our understanding, but I’d encourage readers to consider the philosophical dimensions: How do we view life when such destructive creativity exists at the microscopic scale? What does it teach us about resilience and fragility?
It’s also comforting to know that science is actively seeking ways to disrupt these harmful processes — a beacon of hope amid the biological chaos.
Richard Gerhart
August 5, 2025 AT 15:20Hey all, just jumping in to add some friendly insights from my experience. The article explains the basics nicely but I want to highlight that tumor growth rates can vary significantly even within the same cancer type, so individualized assessments are key.
Another thing to consider is that angiogenesis inhibitors are part of some treatment regimens, but their effectiveness can depend not only on the cancer biology but also on patient health and even genetic factors.
For anyone curious about the numbers mentioned in the article, it’s important to remember these are averages or model-based estimates, so not everyone’s situation will line up exactly.
If you or someone you know is facing cancer, discussing these complexities with your medical team can provide better tailored information.
Martin Gilmore
August 14, 2025 AT 21:33Ok but seriously, the way this article tries to simplify tumor biology sometimes oversells the DIY approach to understanding cancer. You can't just gloss over the nuances of mitosis and angiogenesis like they're some basic DIY projects. Cancer is ruthless, complicated, and brutal.
The piece is good for awareness but kinda boring if you want the gritty, hardcore science behind why some tumors just steamroll through the body with terrifying speed. What about the molecular checkpoints and the role of tumor suppressors? That stuff is critical and isn’t mentioned here.
Still, it’s a decent intro for newcomers but barely scratches the surface.
jana caylor
August 17, 2025 AT 11:07Love this article – so informative and well put together! It really lays out the key factors behind tumor growth in a way that anyone can understand, without dumbing it down. The explanation about angiogenesis was my favorite part, because it made me realize how cancer really manipulates the body’s natural processes.
I also think highlighting the current treatments that block these pathways is super important, especially for families like mine who have been touched by cancer. Knowing there is hope and ongoing research makes a big difference.
Would love to see more posts breaking down other complex diseases like this in the future!