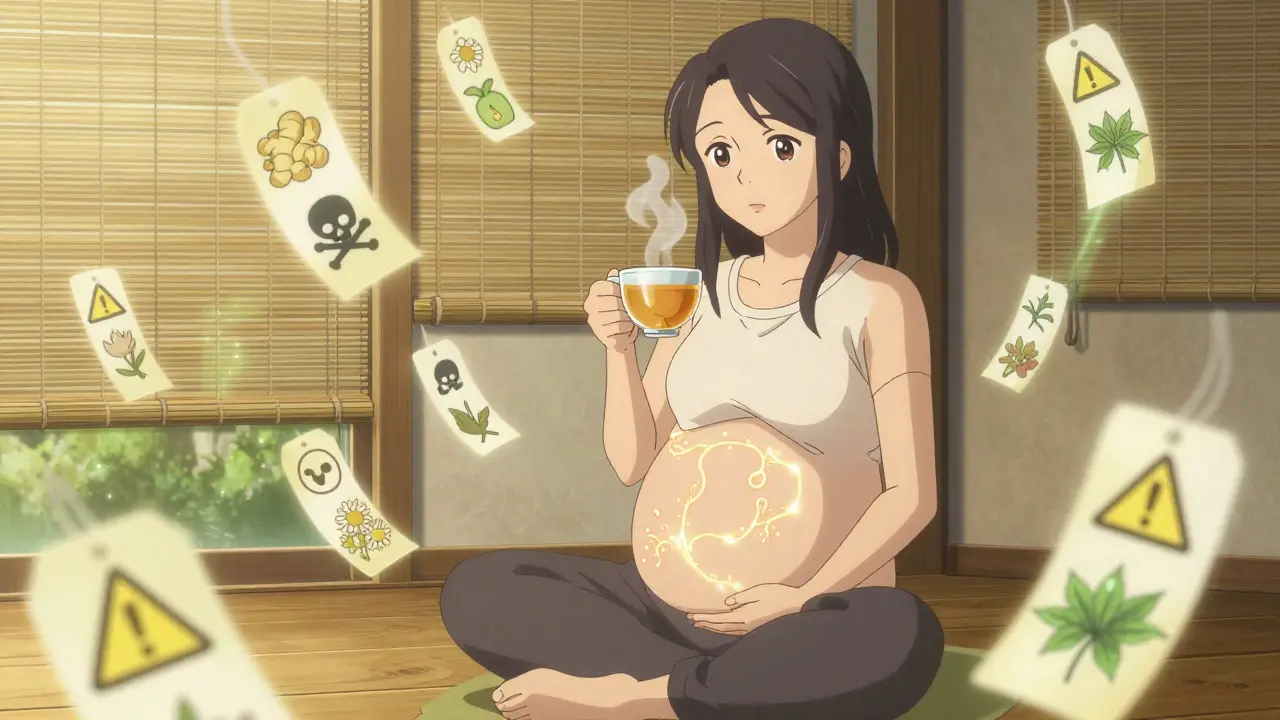
More than 1 in 4 pregnant women in the U.S. take herbal supplements during pregnancy. They reach for ginger tea to calm nausea, raspberry leaf to prepare for labor, or chamomile to sleep better. But here’s the problem: no one really knows if these are safe. Unlike prescription drugs, herbal supplements aren’t tested for pregnancy use. They’re sold as "natural," and that’s enough for many to assume they’re harmless. But "natural" doesn’t mean safe-especially when you’re growing a baby.
What Are You Actually Taking?
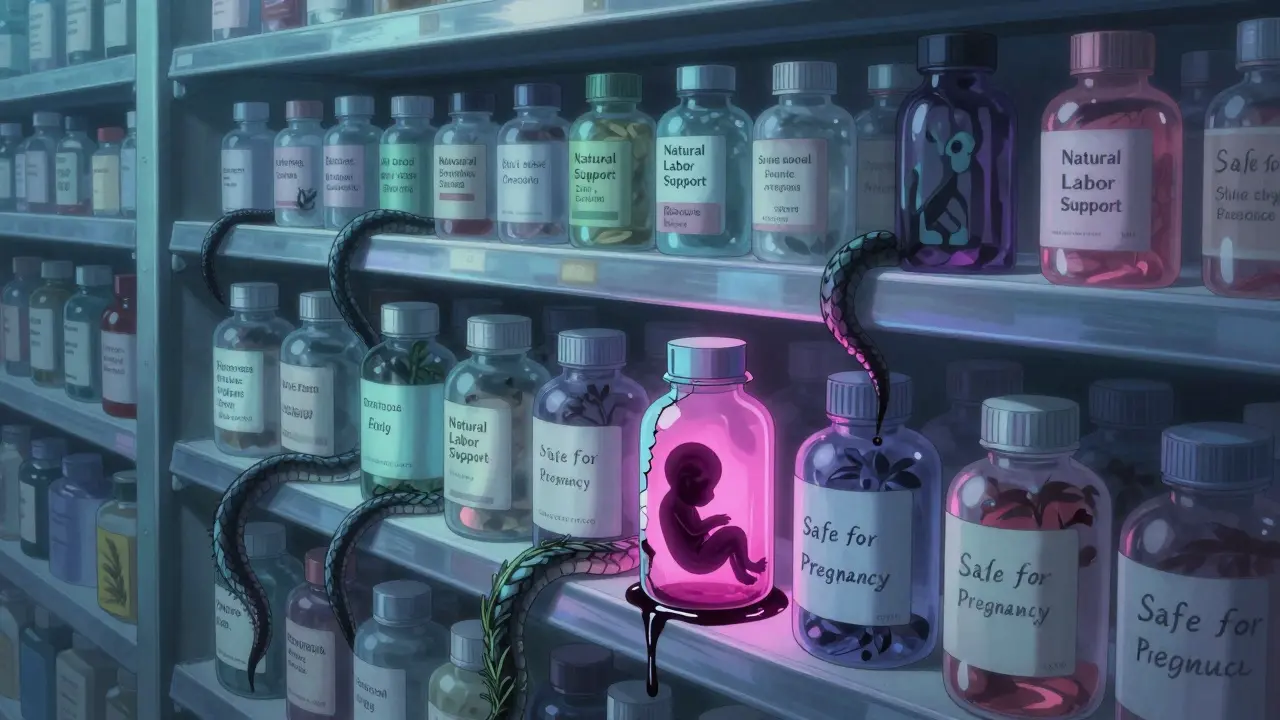
Herbal supplements aren’t standardized. One bottle of ginger might have 250 mg per capsule; another might have 750 mg. Some brands add fillers, heavy metals, or even unlisted herbs. The FDA doesn’t require proof of safety or purity before these products hit shelves. In fact, inspections show 20% to 60% of herbal supplements contain ingredients not listed on the label. That’s not a typo. You could be buying something you didn’t ask for-and it might be dangerous.Take red raspberry leaf, for example. It’s marketed as a "uterine tonic" to help labor go smoother. But a 2023 review by the American Academy of Family Physicians found that women who used it to induce labor had higher rates of cesarean delivery. It’s not just folklore-it’s a documented risk. And yet, 78% of women who took it in one Spanish study started using it in the third trimester, often without telling their doctor.
Ginger: The One That Actually Works
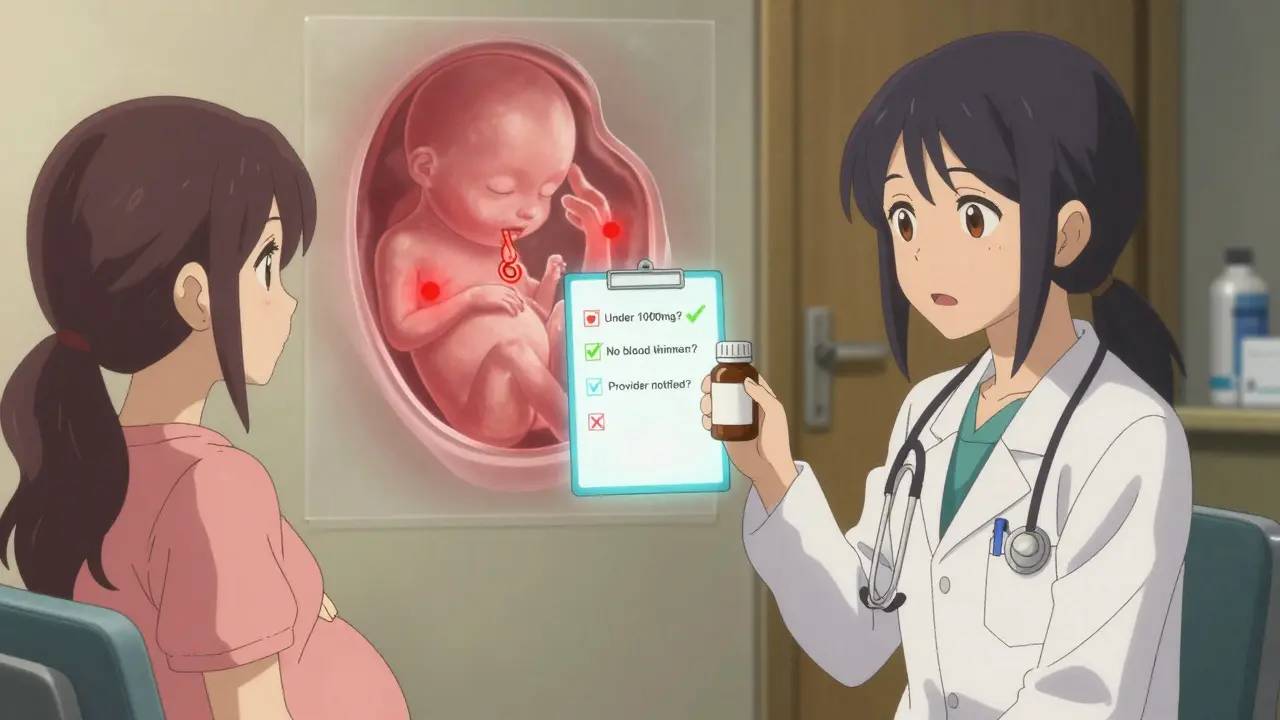
Ginger is the exception. It’s the most studied herb in pregnancy, and the evidence is clear: for nausea and vomiting, it works as well as over-the-counter anti-nausea meds-with fewer side effects. Doses under 1,000 mg per day are considered safe, according to multiple clinical reviews, including one from the Cleveland Clinic in 2023. It’s the only herbal supplement that has enough data to be recommended by major medical groups.But even ginger isn’t risk-free. If you’re taking blood thinners like warfarin, ginger can increase bleeding risk. If you have gallstones, it might make them worse. And if you’re not sure how much you’re getting-whether it’s tea, capsules, or candied ginger-you could be overdoing it. One cup of ginger tea might be fine. Three cups a day? That’s a different story.
The Dangerous Myths
Chamomile is everywhere-tea bags in grocery stores, bedtime blends, even baby products. But it’s not harmless in pregnancy. The same AAFP review flagged it for possible links to preterm birth, low birth weight, and problems with the baby’s heart duct. Still, it’s widely used for anxiety and sleep. Why? Because people believe "it’s just tea."Cranberry supplements are another trap. They’re promoted to prevent urinary tract infections (UTIs), and yes, they might help. But in the third trimester, they’ve been tied to spotting-something that can trigger panic and unnecessary medical visits. And while antibiotics like nitrofurantoin have their own risks, they’re tested, dosed, and monitored. Cranberry? You’re guessing.
And then there’s rosemary. Used topically in lotions? Probably fine. Taken orally as a supplement? Possibly unsafe. It can stimulate uterine contractions. Same goes for pennyroyal, blue cohosh, and high-dose black cohosh. These aren’t obscure herbs-they’re sold in health food stores. And many women have no idea they’re dangerous.
Why Do Women Use Them Anyway?
It’s not just about wanting to avoid pills. Many women feel unheard. Nausea, fatigue, anxiety-doctors sometimes shrug and say, "It’s just pregnancy." So women turn to what feels more natural: herbs, teas, home remedies. In one study in Catalonia, 42% of women started using herbal supplements without telling their provider. They got advice from their mom, a Facebook group, or a YouTube video.There’s also cultural influence. In Asian communities, herbal medicine is deeply rooted in tradition. Korean studies show nearly 60% of pregnant women use herbal remedies. In Scandinavian countries, that number drops to 22%. This isn’t about ignorance-it’s about different systems of care. But when those systems aren’t backed by modern research, the risks multiply.
What the Experts Say
The American College of Obstetricians and Gynecologists (ACOG) is blunt: "Don’t take any herbal product without talking to your provider first." The CDC says we have "limited information" to make decisions. The FDA says herbal supplements don’t go through the same scrutiny as drugs. And yet, millions of women use them anyway.Here’s what providers need to do: ask. Not once. Not at the first visit. Every visit. "Are you taking any herbs, teas, or supplements?" That question needs to be as routine as asking about prenatal vitamins. Most women won’t bring it up unless prompted. And if they do, they need honest answers-not dismissal.
Some doctors still say, "It’s just chamomile tea." But the data doesn’t support that. A 2023 study in BMC Complementary Medicine and Therapies tracked over 1,000 pregnant women in Spain. The most common herbs were ginger, chamomile, thyme, and raspberry leaf. But the study didn’t just track use-it tracked outcomes. And the results weren’t reassuring.
What You Should Do Right Now
If you’re pregnant and taking any herbal supplement-yes, even ginger-stop and talk to your provider. Bring the bottle. Take a photo of the label. Don’t assume it’s safe because it’s sold in a health food store or labeled "organic."- If you’re using ginger for nausea: keep it under 1,000 mg per day and avoid it if you’re on blood thinners.
- If you’re using raspberry leaf: stop before 36 weeks unless your provider specifically advises otherwise.
- If you’re using cranberry for UTIs: consider antibiotics instead-they’re more reliable and better studied.
- If you’re using chamomile for sleep: switch to non-herbal options like magnesium or cognitive behavioral therapy for insomnia.
- If you’re using anything else: don’t guess. Ask.
There’s no such thing as a "safe herbal supplement" in pregnancy-only ones with more or less evidence. Ginger has the most. Everything else? We’re flying blind.
The Bigger Problem
We’re not just missing data-we’re missing research. Pregnant women are excluded from clinical trials. It’s ethical, yes-but it leaves us with nothing but guesses. The NIH just launched a $12.7 million study to fix this. But it will take years. In the meantime, women are making life-altering choices with incomplete information.The market is booming. Global sales of herbal supplements hit $85 billion in 2023. Four percent of that is targeted at pregnant women. Companies are making claims about "natural labor support" and "safe pregnancy blends." The FDA issued warning letters to three manufacturers in January 2024 for exactly that. But enforcement is slow. And the labels? Still misleading.
Final Thought
You don’t need to fear every herb. But you need to stop assuming safety. Pregnancy is the one time in your life when every choice has two lives in the balance. If you’re going to take something-whether it’s a pill, a tea, or a capsule-you need to know why. And you need to know what you’re risking.Ask your provider. Bring the bottle. Write it down. And if they don’t know the answer? That’s not their fault. It’s the system’s. But you can still protect yourself.
 Questions to Ask Your Doctor About Medication Side Effects
Questions to Ask Your Doctor About Medication Side Effects
 Quality and Efficacy: Are Authorized Generics as Good as Brand-Name Drugs?
Quality and Efficacy: Are Authorized Generics as Good as Brand-Name Drugs?
 Safe Buspirone Tapering: Steps, Timelines, and Tips for Success
Safe Buspirone Tapering: Steps, Timelines, and Tips for Success
 Why a Multidisciplinary Approach Is Crucial for Poor Muscle Control
Why a Multidisciplinary Approach Is Crucial for Poor Muscle Control
 Modified-Release Formulations: What You Need to Know About Bioequivalence Standards
Modified-Release Formulations: What You Need to Know About Bioequivalence Standards
Kathy Scaman
January 28, 2026 AT 07:17So many people treat herbal stuff like it’s harmless candy. I had a friend take raspberry leaf tea because her mom swore by it-ended up in preterm labor. No joke. We need better education, not just fear-mongering.
Howard Esakov
January 28, 2026 AT 07:29Of course you’re going to get bad data when you let unregulated snake oil vendors sell to pregnant women. 🤦♂️ The FDA’s hands are tied because of that ridiculous ‘natural’ loophole. If it’s not a drug, it’s a free-for-all. Time to reclassify these as controlled substances. No more ‘it’s just tea’ nonsense.
Mindee Coulter
January 28, 2026 AT 10:25I used ginger for nausea and it saved my sanity. Just kept it under 800mg and never mixed it with anything else. My OB knew and said it was fine. Communication is everything. Don’t be scared, just be informed.
Timothy Davis
January 29, 2026 AT 09:48Let’s be real-most of these ‘studies’ are underpowered, observational, and funded by supplement companies pretending to be ‘independent researchers.’ The 2023 Spanish study? N=1000 sounds big, but they didn’t control for socioeconomic status, diet, or prenatal care quality. Correlation ≠ causation. And yet, people treat it like gospel.
Meanwhile, the real issue is systemic: OB-GYNs don’t get trained in herbal pharmacology. So they say ‘don’t take anything’ instead of ‘here’s what the actual evidence says.’ That’s lazy medicine.
Also, calling chamomile ‘dangerous’ is hyperbolic. One cup of tea isn’t going to induce preterm birth. But yes, high-dose extracts? Maybe. But that’s true of everything. Water can kill you if you drink 10 liters in an hour.
Stop treating herbal supplements like they’re inherently evil. Treat them like any other bioactive compound: evaluate dose, route, context, and evidence. Not fear, not folklore.
And for god’s sake, stop blaming mothers. They’re not idiots. They’re navigating a broken system where their concerns are dismissed until they’re in crisis.
Sue Latham
January 31, 2026 AT 09:20Ugh, I’m so tired of people acting like they’re the only ones who’ve ever thought about this. Like, hello? I’ve been taking ginger tea since week 6 and my baby is now 2 and climbing walls. 🙄 If you’re scared, fine. But don’t guilt-trip the rest of us for using what works. My grandma used rosemary for everything. We’re still here.
Colin Pierce
February 1, 2026 AT 13:51I’m a midwife and I see this all the time. Women come in with bottles of ‘natural labor prep’ blends that contain pennyroyal and blue cohosh. They don’t even know what’s in them. I don’t judge-I just say ‘can I see the label?’ and then we talk. Most are relieved someone finally asked. The real enemy isn’t the herbs-it’s the silence around them.
Here’s what works: ask every patient, every visit. Write it down. Keep a list. If they’re using chamomile, ask how much, how often, and why. If they’re using ginger, confirm the dose. Most of them have no idea. And that’s not their fault.
Also-yes, ginger is the only one with solid data. But even that’s not perfect. Some brands have 5x the labeled dose. Get your ginger from a reputable source. Or just make tea from fresh root. Less risk, same benefit.
Anna Lou Chen
February 3, 2026 AT 01:45Ah, the epistemological crisis of prenatal care: the neoliberal commodification of wellness culture colliding with the ontological insecurity of maternal subjectivity. We’re told to ‘trust our bodies’-but the body is a site of biopolitical regulation, where ‘natural’ becomes a neoliberal fetish masking structural abandonment. The FDA’s regulatory void isn’t negligence-it’s a feature of late-stage capitalism’s disinvestment in reproductive health infrastructure.
Women turn to herbalism not because they’re gullible, but because the medical-industrial complex has failed to provide embodied, trauma-informed care. The ‘danger’ isn’t the raspberry leaf-it’s the institutionalized dismissal of maternal intuition. We pathologize self-care because we’ve outsourced authority to a system that treats pregnancy as a pathology to be managed, not a phenomenon to be honored.
So yes, document the labels. Yes, ask your provider. But also: demand that the system stop treating pregnant bodies as experimental subjects while simultaneously denying them the tools to protect themselves. The real risk isn’t chamomile-it’s the silence that follows when you say, ‘I don’t know.’
John Rose
February 4, 2026 AT 18:29This is such an important conversation. I’m not a medical professional, but I’ve spent the last year researching this because I was terrified of doing something wrong. I’m so glad someone laid this out clearly. I stopped all supplements except ginger (under 800mg) and switched to magnesium for sleep. I wish my doctor had asked me about it earlier.
Can we make a simple checklist for OB offices? Like, ‘Herbal Use Screening’ as a standard form? It shouldn’t be up to the patient to bring it up.
Lexi Karuzis
February 6, 2026 AT 14:47WAIT. Did you know that 78% of these ‘herbal’ supplements are laced with synthetic hormones? The FDA doesn’t test them, but Big Pharma secretly funds the labs that DO test them-and then they bury the results. I’ve seen the documents. It’s not just unregulated-it’s a cover-up. They want you to think ginger is safe so you don’t question the real danger: the pharmaceutical industry’s monopoly on pregnancy care. They profit from C-sections. They profit from anxiety. They profit from you being afraid to ask.
Bring the bottle? Bring the WHOLE BOX. And then go to the FDA website and file a complaint. They’re watching. They’re always watching.
Brittany Fiddes
February 7, 2026 AT 06:04Oh, please. The Americans think they’re the only ones who’ve ever heard of herbal medicine. In the UK, we’ve been using chamomile and ginger for centuries. My great-grandmother drank raspberry leaf tea and had 7 kids without a single C-section. This is just American medical arrogance wrapped in ‘evidence.’ You don’t need a double-blind RCT to know what your ancestors knew.
Also, why is it always ‘don’t take anything’? Why not ‘take what’s been used safely for generations’? We’re not lab rats. We’re humans. Stop colonizing traditional medicine with your clinical trial fetish.
Mark Alan
February 7, 2026 AT 13:30MY WIFE TOOK GINGER TEA AND HAD A HEALTHY BABY 🎉🔥 NO REGRETS. IF YOU’RE SCARED, DON’T DO IT. BUT DON’T SCARE OTHERS. LIFE ISN’T A CLINICAL TRIAL. 🌿👶