Getting your medication list right isn’t just about writing down what you take. It’s about making sure the safety alerts tied to those drugs are clear, visible, and acted on-every single time. A single missed alert on a high-risk drug like insulin or warfarin can lead to a preventable emergency. This isn’t hypothetical. In U.S. hospitals, medication errors involving high-alert drugs cause over 1,000 deaths annually, and nearly half of them could have been stopped with proper documentation.
Why Safety Alerts on Your Medication List Matter
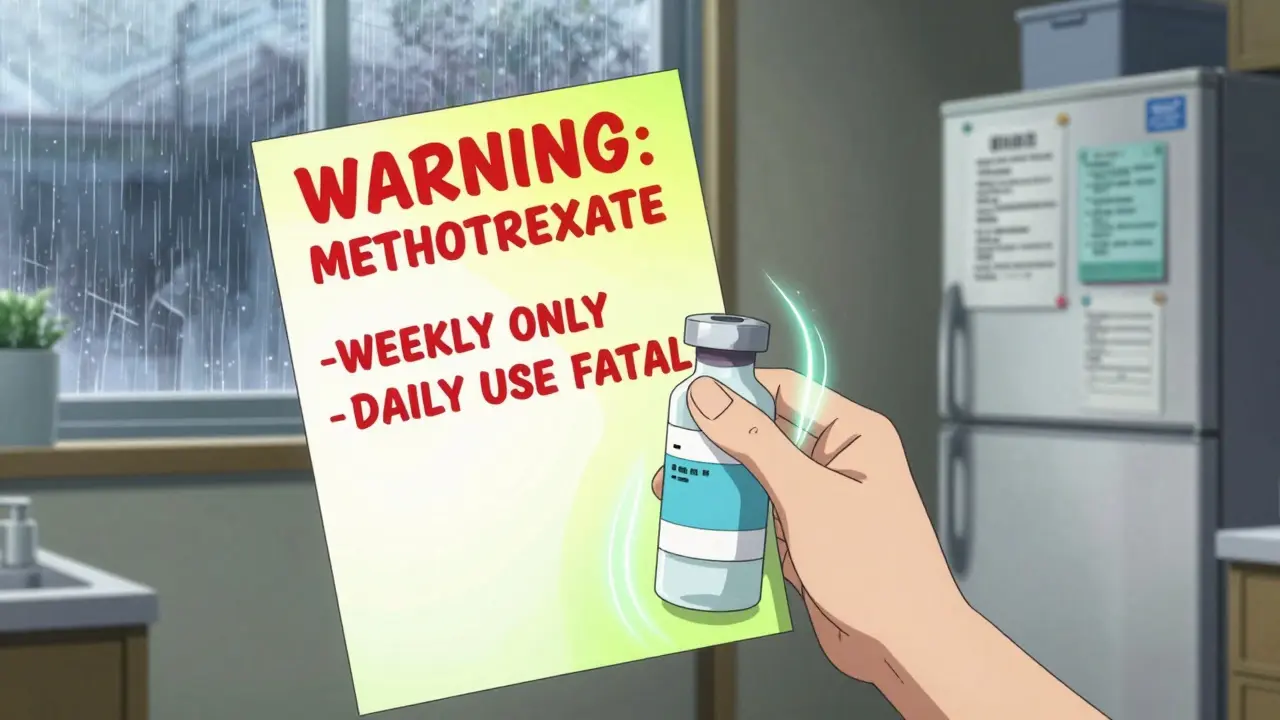
Not all medications carry the same risk. The Institute for Safe Medication Practices (ISMP) defines high-alert medications as drugs that have a higher chance of causing serious harm if used incorrectly. These include insulin, opioids, anticoagulants, neuromuscular blockers, and IV potassium chloride. A mistake with one of these isn’t just a typo-it’s a life-threatening event. The problem isn’t always the prescription. It’s the lack of clear, consistent documentation. Many patients and even some providers rely on handwritten lists or vague electronic notes. But a simple label like “Take 1 pill daily” on a bottle of methotrexate? That’s dangerous. Methotrexate is a chemotherapy drug. If taken daily instead of weekly, it can cause bone marrow failure. The difference between life and death is one word: weekly. Documentation isn’t about bureaucracy. It’s about creating a safety net. When safety alerts are clearly written into your medication list, every pharmacist, nurse, and doctor who sees it knows exactly what to watch for. Studies show that facilities using structured documentation cut medication errors by up to 50%. That’s not a small win-it’s a game-changer.What Counts as a Safety Alert?
A safety alert isn’t just a warning. It’s a specific, actionable instruction tied to a drug’s unique risk. Here’s what qualifies:- Dosage frequency warnings: “Methotrexate: Take ONLY once weekly. Do not take daily.”
- Concentration alerts: “Insulin: Use only 100 units/mL concentration. No other strength permitted.”
- Administration requirements: “Neuromuscular blocker: Must be given only in settings with immediate ventilatory support. Label: ‘WARNING: CAUSES RESPIRATORY ARREST - PATIENT MUST BE VENTILATED.’”
- Drug interaction flags: “Avoid NSAIDs with warfarin. Increases bleeding risk.”
- Special monitoring needs: “Lithium: Check kidney function and serum levels every 3 months.”
How to Build Your Safety-Ready Medication List
Start with what you’re already taking. Then, go through each drug and ask: What could go wrong? Here’s how to do it step by step.- Identify high-alert drugs. Use the ISMP’s official list of 19 categories. If you’re on insulin, opioids, heparin, or chemotherapy drugs, you’re in the high-risk group.
- Check the exact instructions. Don’t rely on memory. Look at the prescription label or pharmacy printout. Write down the precise wording: “Take 5 mg once weekly,” not “Take methotrexate.”
- Add the safety alert. After each high-alert drug, write the official warning in bold or all caps. Example: “WARNING: This is a chemotherapy drug. Must be taken weekly. Daily use can be fatal.”
- Include monitoring requirements. If you need blood tests, EKGs, or liver checks, list them. “Check INR weekly. Target range: 2.0-3.0.”
- Update every 30 days. Medications change. New alerts come out. Don’t wait for your next doctor’s visit. Review your list monthly.
Electronic Lists vs. Paper: Which Works Better?
Most people think digital is better. But it’s not always true. Electronic health records (EHRs) can be powerful. Systems like Epic or Cerner can be programmed to trigger hard-stop alerts: if a doctor tries to prescribe daily methotrexate, the system won’t let them proceed unless they select “weekly” and confirm the diagnosis. That’s automation doing the work. But here’s the catch: if the system doesn’t have the right alert set up, or if staff keep clicking “bypass” because they’re rushed, the alert becomes noise. Studies show that when EHRs generate more than 15 alerts per order, doctors ignore over half of them. That’s alert fatigue-and it kills. Paper lists, when done right, are more reliable. They don’t glitch. They don’t auto-bypass. If you’ve written “DO NOT GIVE WITH ALCOHOL” next to metronidazole, no system can override that. The key is consistency. Use the same format every time. Use the same font size. Put alerts in red or underline them. Make them impossible to miss. The best approach? Use both. Keep a paper copy for emergencies and a digital copy synced to your phone. Update them together.What to Do When an Alert Is Bypassed
Sometimes, an alert gets ignored. Maybe the nurse clicked through it too fast. Maybe the doctor didn’t see it. That’s not the end-it’s the beginning of a safety conversation. If you notice an alert was bypassed, ask: “Why was this skipped?” - Was the warning unclear? → Then it needs rewriting. - Was the system too noisy? → Then too many alerts are being generated. - Was the staff overwhelmed? → Then the workflow needs fixing. Document the bypass. Not to blame anyone. To fix the system. In hospitals, every bypassed alert must be logged and reviewed by the medication safety committee. At home, you can do the same. Write it down: “Feb 3, 2026: Insulin dose alert bypassed by pharmacist. Clarified: Use U-100 only.” Keep that note with your list.
Common Mistakes and How to Avoid Them
People mess up safety documentation in predictable ways. Here’s what to watch for:- Vague language: “Be careful with this drug.” → Too weak. Use exact warnings from ISMP or the FDA.
- Missing frequency: “Take 10 mg.” → Is that daily? Weekly? Monthly? Always specify.
- Outdated alerts: “Warfarin: Avoid green vegetables.” → That’s outdated. The real alert is: “Maintain consistent vitamin K intake.”
- One-size-fits-all: Assuming all patients need the same alerts. Not true. Your risk profile is unique.
- Ignoring new alerts: The FDA issues over 120 drug safety updates a year. Check your meds every time you refill.
What’s Changing in 2025?
The rules are getting stricter. Starting January 1, 2025, Medicare and Medicaid will require hospitals to prove they have documented safety protocols for high-alert medications as part of their reimbursement checks. That means hospitals are now under pressure to get this right. The FDA’s new Sentinel Initiative is rolling out automated safety alerts directly into hospital systems, cutting manual entry by 80%. That’s huge. But it also means you need to make sure your personal list matches what’s in the hospital’s system. Don’t assume they’re synced. AI tools are coming. Epic plans to launch an AI module in mid-2025 that auto-prioritizes alerts based on your history. But early versions have missed 18% of critical alerts. So don’t rely on it. Use it as a helper-not a replacement.Final Checklist: Your Safety Alert Document
Before you leave the pharmacy or doctor’s office, run through this:- Are all high-alert drugs clearly labeled?
- Is the exact warning copied from official sources (ISMP/FDA)?
- Is frequency (daily/weekly/monthly) written out?
- Are monitoring requirements listed?
- Is the list updated in the last 30 days?
- Have you shared this with at least one family member or caregiver?
What should I do if my doctor ignores my safety alerts?
If your doctor dismisses documented safety alerts, ask for a written explanation. If they refuse, request a referral to another provider. You have the right to safe care. If you’re in a hospital, ask to speak with the patient safety officer. Most facilities have a formal process for reporting concerns. Never assume your alert is too small to matter.
Can I use a mobile app to document safety alerts?
Yes-but only if the app lets you enter custom alerts with exact wording. Many apps auto-fill generic warnings like “Take with food.” That’s not enough. Look for apps that let you paste official ISMP or FDA language. MyMedList and Medisafe allow custom notes. Avoid apps that only show pre-set alerts without room for your specific warnings.
How often should I update my medication list with safety alerts?
Update it every time you get a new prescription, change a dose, or refill a medication. At minimum, review it every 30 days. New safety alerts from the FDA or ISMP come out frequently. If you’re on insulin or warfarin, check every week. A single outdated alert can be deadly.
Are safety alerts required by law?
For patients, no-but for hospitals and pharmacies, yes. The Joint Commission requires accredited facilities to document and act on high-alert medication risks. Starting in 2025, Medicare will tie reimbursement to this documentation. So while you’re not legally required to keep a list, the system is being forced to take it seriously-and you should too.
What if I can’t afford to see a pharmacist for help?
You don’t need to pay for help. Most pharmacies offer free medication reviews. Call ahead and ask: “Can I schedule a free safety check of my medications?” Pharmacists are trained to spot high-risk drugs and missing alerts. Bring your list. They’ll help you fix it-no cost, no appointment needed in most cases.
 Atomoxetine and Virtual Reality Therapy: The Future of ADHD Treatment?
Atomoxetine and Virtual Reality Therapy: The Future of ADHD Treatment?
 Coronary Calcium Score: What CT Scans Reveal About Plaque Buildup in Your Arteries
Coronary Calcium Score: What CT Scans Reveal About Plaque Buildup in Your Arteries
 Appearance Differences: Why Authorized Generics Look Different from Brand-Name Drugs
Appearance Differences: Why Authorized Generics Look Different from Brand-Name Drugs
 Buy Tamsulosin Online Safely: Where, How, and What You Need to Know
Buy Tamsulosin Online Safely: Where, How, and What You Need to Know
 How and Where to Buy Keppra Online: Safe Ordering & Tips
How and Where to Buy Keppra Online: Safe Ordering & Tips
RAJAT KD
January 9, 2026 AT 18:30Finally, someone who gets it. I’m a pharmacist in Delhi, and I see this every day-people write ‘take 1 pill’ for methotrexate and wonder why they end up in ER. That one word-‘weekly’-is the difference between life and a coffin. Write it in red. Capitalize it. Underline it. No exceptions.
tali murah
January 10, 2026 AT 13:27Oh please. You think writing ‘WARNING’ in bold fixes systemic incompetence? Hospitals ignore alerts because they’re overloaded, not because patients didn’t ‘do their part.’ This is victim-blaming dressed up as safety advice. Your list won’t save you if the nurse doesn’t read it.
Alicia Hasö
January 11, 2026 AT 00:43You’re absolutely right-and I’ve seen this save lives. Last month, my sister handed her list to a new oncologist. He almost prescribed daily methotrexate. She pointed to the red bolded line: ‘DO NOT TAKE DAILY-CHEMO.’ He paused. Apologized. Changed it. That’s not luck. That’s preparation. Do the work. It’s not extra-it’s essential.
Jacob Paterson
January 12, 2026 AT 05:27Let me guess-you also fold your socks by color and alphabetize your spice rack. This is the kind of obsessive control that makes people hate healthcare. You think a piece of paper stops a doctor from being lazy? Wake up. The system is broken. Your list is a Band-Aid on a hemorrhage.
Micheal Murdoch
January 12, 2026 AT 08:27There’s truth here, but it’s not just about writing alerts. It’s about trust. If you’re constantly reminding people you’re not stupid, they’ll tune you out. The goal isn’t to be the most documented patient-it’s to be the most heard one. Build relationships with your pharmacists. Ask them to flag changes. Let them see you care, not just control.
Elisha Muwanga
January 14, 2026 AT 04:48America’s healthcare system is collapsing, and you’re giving people sticky notes to fix it? We need national standards, not DIY safety lists. This reads like a blog post written by a nurse who’s had one too many coffee breaks. Real change requires policy, not panic-posting.
Diana Stoyanova
January 15, 2026 AT 21:45Y’ALL. I just updated my list with ALL the warnings. I used neon pink highlighter, big bold font, and even added little icons: ⚠️ for chemo, 💉 for insulin, 🚫 for alcohol. My mom took a pic and sent it to her whole book club. Now everyone’s doing it. We’re turning safety into a movement. 🌟 You got this. You’re not alone.
Aron Veldhuizen
January 16, 2026 AT 20:05Interesting. You assume patients are the ones failing. But what if the problem is that these ‘official’ alerts are written by bureaucrats who’ve never held a syringe? ‘Take only weekly’-who says? Who verified that? Did they test it on a 78-year-old with dementia? Or is this just another checklist designed to protect hospitals from lawsuits, not people from death?
Ian Long
January 18, 2026 AT 15:29Both sides have points. I’ve had doctors ignore my list. I’ve also had pharmacists say, ‘I’ve never seen a patient do this-and it’s the only thing that saved me.’ The answer isn’t ‘paper vs digital’-it’s ‘both, and make them talk to each other.’ If your app can sync with your hospital’s EHR and flag discrepancies? That’s the future. Until then? Keep the paper. And keep asking.
Pooja Kumari
January 20, 2026 AT 08:40I’ve been on warfarin for 12 years. I’ve had three near-deaths because someone didn’t see my alert. I wrote it in three places. I emailed it to every doctor. I even printed it on a T-shirt once. No one listened. So now I just scream when they open the chart. It’s the only thing that works. You think your list matters? It doesn’t. Your voice does.
Angela Stanton
January 21, 2026 AT 10:06Let’s be real: this is just another ‘patient empowerment’ marketing ploy. You’re being sold a checklist as a solution to a $1.5T systemic failure. You’re not a safety officer. You’re a patient. The burden shouldn’t be on you to audit the system. But hey-go ahead. Print it. Laminate it. Post it on LinkedIn. At least you’ll feel like you’re doing something.
Johanna Baxter
January 21, 2026 AT 21:09I cried reading this. My mom died because the nurse didn’t see the ‘weekly’ on her methotrexate. I wrote it in blood on her list. No one cared. Now I scream at every pharmacist. I don’t care if I’m ‘too much.’ If you’re not screaming, you’re not trying hard enough.
Phil Kemling
January 22, 2026 AT 17:06What does ‘safety’ mean when it’s reduced to a checklist? Is it protection-or compliance? We treat patients like failed systems that need manual overrides. But what if the real danger isn’t the drug-it’s the belief that a human can be reduced to a set of instructions?
Jerian Lewis
January 24, 2026 AT 04:17I’m not going to argue. I just update my list every 30 days. I don’t post it. I don’t talk about it. I just keep it in my wallet. And every time I hand it over, I say nothing. I let the words speak. Most providers don’t even look. But some do. And when they do? That’s the moment everything changes.
Drew Pearlman
January 25, 2026 AT 16:28I know it sounds like a lot, but honestly? This is the easiest way to take control of your health. Think of it like a seatbelt-you don’t wear it because you think you’ll crash. You wear it because you’re smart. Same here. You don’t write these alerts because you expect someone to mess up. You write them because you’re not willing to bet your life on someone else’s attention span. And that’s not paranoid. That’s wise.