Most people assume that a generic pill is just a cheaper version of the brand-name drug - and they’re mostly right. The active ingredient is the same. The effect on your body is supposed to be identical. But here’s the part no one tells you: generic medications can trigger allergic reactions that the brand-name version never did. And it’s not because the medicine doesn’t work. It’s because of what’s hiding in the filler.
Why a Generic Might Make You Sick When the Brand Didn’t
Generic drugs are required by the FDA to match the brand-name version in strength, dosage, and how the body absorbs the active ingredient. But they’re not required to match the inactive stuff. That means the dye, the binder, the preservative, or the filler can be completely different. And those ingredients? They can be allergens.Take lactose, for example. It’s in nearly 3 out of 10 generic pills. If you’re lactose intolerant, you might think, ‘It’s just a little sugar - how bad could it be?’ But for some people, even a tiny amount triggers bloating, cramps, or worse - hives, swelling, even breathing trouble. Gluten is another silent trigger. It shows up in 1 in 8 generics, and if you have celiac disease, that’s not just a stomachache - it’s an immune system explosion.
Dyes are a big problem too. Tartrazine (Yellow No. 5), a common coloring in liquid generics and some tablets, has been linked to rashes, asthma flare-ups, and anaphylaxis in sensitive people. One patient in Boston reported breaking out in hives every time she took generic sertraline - but never had a problem with Zoloft. Turns out, the generic had tartrazine. The brand didn’t.
Even something as simple as magnesium stearate, a common lubricant in pills, has been found to trigger reactions in people with penicillin allergies - even when the active ingredient was perfectly safe. That’s not a coincidence. It’s chemistry.
What Do These Reactions Look Like?
Allergic reactions to generics don’t always come screaming in. Sometimes they whisper. And that’s dangerous.
Mild reactions show up as skin stuff: itching, red patches, hives. These might seem like a rash from laundry detergent - until they don’t go away after 6 hours. That’s a red flag. About 7 in 10 mild reactions involve a rash. Nearly half involve hives. And 6 in 10 involve itching that doesn’t quit.
Moderate reactions mean your body is fighting back across systems. You might get swelling around your lips or eyes. Your stomach could churn with nausea or vomiting. You might feel tightness in your chest or start wheezing. These aren’t ‘just bad side effects.’ They’re signs your immune system is attacking something in the pill.
Severe reactions - anaphylaxis - are life-threatening. Throat closing. Blood pressure crashing. Skin turning pale or blue. Breathing faster than 30 times a minute. You might feel dizzy, faint, or like you’re going to pass out. This can happen within minutes of swallowing the pill. In nearly half of all severe cases, symptoms hit within 15 minutes.
And here’s the scary part: 19% of reactions don’t show up until hours later. You take the pill at 8 a.m., feel fine, go to work, then at 4 p.m., your face swells. You think it’s a cold. It’s not.
When to Call 911 - Not Wait It Out
If you’re taking a generic and suddenly feel like something’s wrong, don’t second-guess yourself. Don’t wait to see if it ‘gets better.’
Call 911 immediately if you have:
- Wheezing, stridor (a high-pitched sound when breathing), or breathing faster than 30 times per minute
- Systolic blood pressure below 90, or a drop of more than 30% from your normal baseline
- Swelling of the tongue, lips, or throat
- Two or more systems reacting at once - like hives + vomiting + dizziness
If you have an epinephrine auto-injector (EpiPen), use it right away. Don’t wait for an ambulance. Epinephrine is the only thing that stops anaphylaxis from killing you. Studies show that if you wait more than 15 minutes to use it, your chance of survival drops sharply.
And yes - this applies to generics too. If you’ve had a reaction to a generic, you might assume the brand-name version is safe. But if the active ingredient is the same, your body may still react. Always assume the worst until proven otherwise.

What to Do If It’s Not an Emergency - But Still Worrisome
Not every reaction is life-threatening. But that doesn’t mean it’s harmless.
If you get hives that last more than 6 hours, swelling that doesn’t fade in 24 hours, or stomach pain that won’t quit after 2 hours - call your doctor. Don’t brush it off as ‘just a side effect.’
Here’s why: 65% of people who have a mild reaction to a generic will have a worse one the next time they take it. That’s not luck. That’s how the immune system works. Once it flags something as a threat, it remembers. And next time, it goes harder.
See an allergist within 72 hours. They can run tests to figure out if it was the active drug - or one of the fillers. Many people think they’re allergic to penicillin, but 9 out of 10 aren’t. They just had a reaction to a dye or binder in the generic version. Proper testing can free you from unnecessary drug restrictions and dangerous alternatives.
How to Protect Yourself Going Forward
Here’s what works - and what doesn’t.
Don’t assume all generics are the same. Two different companies make generic lisinopril. One has lactose. One doesn’t. One has a red dye. One is white. You can’t tell by looking.
Do ask your pharmacist: ‘Is this generic the same as the last one I got?’ If they say ‘yes,’ ask again: ‘What’s the inactive ingredient list?’ They have access to the FDA’s Inactive Ingredient Database. They should be able to tell you if there’s a change.
Do keep a ‘medication allergy passport.’ Write down every ingredient you’re allergic to - lactose, gluten, tartrazine, peanut oil, FD&C dyes, etc. Show it to your doctor and pharmacist every time you get a new script. One study found this simple habit cuts adverse events by nearly a third.
Do ask for ‘dye-free,’ ‘gluten-free,’ or ‘lactose-free’ versions. About 4 in 10 major generic makers now offer them. They’re not always cheaper, but they’re safer. And if your insurance won’t cover them, ask for a prior authorization - your doctor can justify it if you have a documented reaction.
Do get your prescription labeled. If you’ve had a reaction, ask your doctor to write ‘Do Not Substitute’ on the script. That forces the pharmacy to give you the exact brand or generic you’ve tolerated.

Why This Is Getting Worse - And What’s Changing
Generics make up 9 out of 10 prescriptions filled in the U.S. That’s huge. And as more people switch, more reactions are being reported. Between 2019 and 2022, complaints about generic-related allergies jumped 22%.
Part of the problem? Doctors and pharmacists don’t always ask. A 2023 survey found that only 71% of allergy specialists now routinely ask patients whether they’ve had reactions to generics - up from 42% in 2019. That’s progress, but it’s still not standard.
And patients? Most don’t know to look. They see ‘generic’ and assume it’s safe. They don’t check the label. They don’t compare pills. They don’t realize that the little white dot on one pill and the red stripe on another could be the difference between feeling fine and ending up in the ER.
The FDA is finally stepping up. By 2025, manufacturers will be required to clearly label high-risk inactive ingredients on packaging. But until then, you have to be your own advocate.
Real Stories, Real Risks
A man in Ohio took a generic version of propofol for a procedure. He’d had it before - brand-name - with no issues. This time, he went into cardiac arrest. Turns out, the generic version used peanut oil as a solvent. He had a peanut allergy. No one asked.
A woman in Chicago developed severe hives after switching from brand-name metoprolol to a generic. She thought it was stress. Two weeks later, she couldn’t breathe. She was rushed to the hospital. Testing showed she was allergic to the dye in the generic - the same dye that’s used in some candies and sodas.
These aren’t rare. They’re predictable. And they’re preventable.
If you’ve ever had a reaction to a generic - even a mild one - you’re not crazy. You’re not overreacting. You’re paying attention. And that’s the first step to staying safe.
Can a generic medication cause an allergic reaction even if the brand-name version didn’t?
Yes. Generic medications must match the active ingredient of the brand-name drug, but they can use different inactive ingredients like dyes, fillers, or preservatives. These can trigger allergic reactions in people who tolerate the brand-name version just fine. For example, someone might react to tartrazine dye in a generic version of sertraline but have no issue with Zoloft, which doesn’t contain that dye.
What are the most common allergens in generic medications?
The most common allergens in generics include lactose (found in 28% of oral generics), gluten (in 12%), tartrazine (FD&C Yellow No. 5, in 15% of liquid generics), and peanut oil (in 8% of injectables). Magnesium stearate and other lubricants have also been linked to reactions in sensitive individuals, particularly those with known drug allergies.
When should I go to the ER after taking a generic medication?
Go to the ER or call 911 immediately if you experience difficulty breathing, wheezing, throat swelling, a sudden drop in blood pressure (below 90 mmHg), dizziness or fainting, or if two or more body systems are affected at once - like hives plus vomiting or swelling plus chest tightness. These are signs of anaphylaxis, a life-threatening reaction that requires epinephrine and emergency care.
What should I do if I get a mild reaction like a rash or itching from a generic?
Even mild reactions like hives, itching, or swelling that lasts more than 6 hours should be evaluated by a doctor within 24 hours. These can be early warning signs. About 65% of people who have a mild reaction to a generic will have a more severe reaction the next time they take it. See an allergist within 72 hours to identify the trigger and avoid future reactions.
How can I avoid allergic reactions to generics in the future?
Keep a list of all inactive ingredients you’re allergic to - like lactose, gluten, or tartrazine - and carry it with you as a ‘medication allergy passport.’ Always ask your pharmacist if the generic you’re getting has the same inactive ingredients as your last prescription. Request dye-free, gluten-free, or lactose-free versions when available. And ask your doctor to write ‘Do Not Substitute’ on your prescription if you’ve had a reaction before.
Are generic medications less safe than brand-name drugs?
No - generic medications are just as safe and effective as brand-name drugs when it comes to the active ingredient. The risk isn’t from the medicine itself, but from differences in inactive ingredients that aren’t always disclosed or understood. The FDA requires generics to meet strict standards for potency and absorption. But because inactive ingredients aren’t always tested for allergenic potential, patients need to be proactive about checking labels and communicating with their care team.

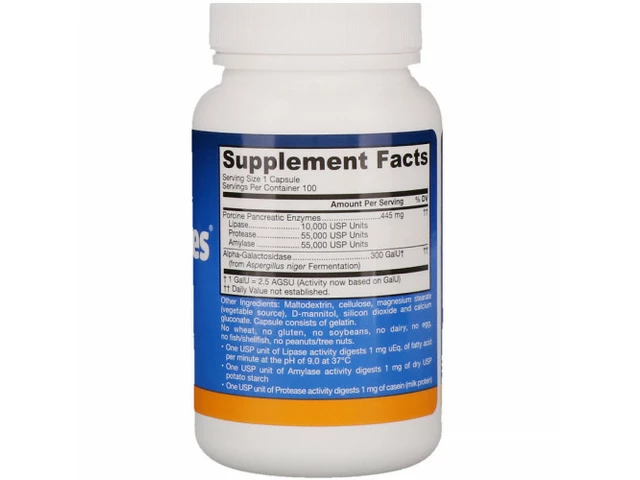 Unlock the Power of Lipase: The Ultimate Dietary Supplement for Improved Digestion
Unlock the Power of Lipase: The Ultimate Dietary Supplement for Improved Digestion
 How to Buy Cheap Generic Claritin Online Safely and Save Money
How to Buy Cheap Generic Claritin Online Safely and Save Money
 Understanding Zollinger-Ellison Syndrome and Its Link to Pancreatic Tumors
Understanding Zollinger-Ellison Syndrome and Its Link to Pancreatic Tumors
 Can Tazarotene Reduce Wrinkles? Anti‑Aging Benefits Explained
Can Tazarotene Reduce Wrinkles? Anti‑Aging Benefits Explained
 Nebulizers vs. Inhalers: Which One Really Works Better for Asthma and COPD?
Nebulizers vs. Inhalers: Which One Really Works Better for Asthma and COPD?
Elen Pihlap
January 7, 2026 AT 03:26I took a generic pill last month and broke out in hives. Thought it was my laundry detergent. Turns out it had tartrazine. Now I check every pill like it's a bomb. My pharmacist thinks I'm crazy but I'd rather be safe than dead.
Also why does no one talk about this?!
Sai Ganesh
January 7, 2026 AT 11:07In India, generics are the only option for most people. But we don't always know what's inside. I once had swelling after a generic antibiotic. The pharmacist didn't know the filler was gluten. We need better labeling here too.
Not just in the US.
Adam Gainski
January 8, 2026 AT 01:26This is one of the most important posts I've read in years. I'm a pharmacist and I see this all the time. Patients assume 'generic = same' and don't realize the fillers can be totally different between brands.
That's why I always ask patients: 'Did you switch generics recently?' and I check the inactive ingredients in the FDA database before dispensing. It's not part of the standard script, but it should be.
Also, if you've had a reaction, ask for the lot number. Sometimes it's not even the generic - it's a bad batch from one manufacturer.
Jonathan Larson
January 8, 2026 AT 12:36There is a profound irony in our healthcare system: we demand cost-efficiency, yet we ignore the human cost of hidden variables in medication.
Generics are not inferior - they are merely incomplete in their disclosure. The body does not distinguish between 'active' and 'inactive' - it responds to molecular presence, regardless of label.
Perhaps the real question is not whether generics are safe, but why we have allowed our regulatory frameworks to prioritize economics over transparency.
Until every pill carries a full, legible, allergen-free ingredient list - we are not treating patients. We are gambling with their biology.
Alex Danner
January 10, 2026 AT 09:50OMG I had this happen with sertraline. I was on Zoloft for 5 years. Switched to generic - woke up with my face swollen like a balloon. Thought I was having a stroke. Went to ER. They said 'allergic reaction to Yellow No. 5.'
Turns out the generic had it. Zoloft didn't. I now carry a printed list of banned ingredients in my wallet. My doctor calls it my 'Medication Survival Kit.'
Also - if you're on thyroid meds? Watch out for lactose. It's everywhere.
THIS IS REAL. DON'T IGNORE IT.
Andrew N
January 11, 2026 AT 17:23Most of these reactions are probably placebo. People get anxious about generics so they feel symptoms. Also, 19% delayed reactions? That's not science - that's cherry-picked data. The FDA approves these drugs. If they were dangerous, they'd be pulled.
Stop fearmongering.
Jessie Ann Lambrecht
January 12, 2026 AT 18:30YESSSSS this is so important!! I used to be the person who said 'it's just a pill' - until my sister almost died from a generic antibiotic with peanut oil.
Now I carry my 'allergy passport' like a badge of honor. I even printed it on a laminated card. My pharmacist cries when she sees it - in a good way.
TO EVERYONE READING: If you’ve ever had a weird reaction - even if it was 'just a rash' - GO SEE AN ALLERGIST. Don't wait. Your future self will thank you.
Also - ask for dye-free. They exist. And yes, they're worth the extra $2.
Katrina Morris
January 14, 2026 AT 01:16i switched generics last week and my throat felt tight but i thought it was allergies
then i read this and i freaked out
went to the pharmacy and asked about the filler
they said it had lactose
i dont even know i was lactose intolerant
now im scared to take anything
but also kind of glad i know
thank you for writing this
LALITA KUDIYA
January 14, 2026 AT 11:22Same in India we dont know what is in generics
but now i ask my pharmacist for the list
and i write it down on my phone
thank you for this post
its life saving :)