Hypernil vs. Alternative Blood Pressure Drugs Comparison Tool
Comparison Results
If you or a loved one have been prescribed a pill to tame high blood pressure, you’ve probably heard the name Hypernil is the brand name for Lisinopril, an angiotensin‑converting enzyme (ACE) inhibitor. It’s a go‑to option for many clinicians because it’s cheap, once‑daily, and backed by decades of data. Still, a handful of other drugs can do the same job, and choosing the right one isn’t always obvious. Below we break down how Hypernil stacks up against its most common peers, so you can decide what matters most for your health, wallet, and lifestyle.
What makes Hypernil (Lisinopril) work?
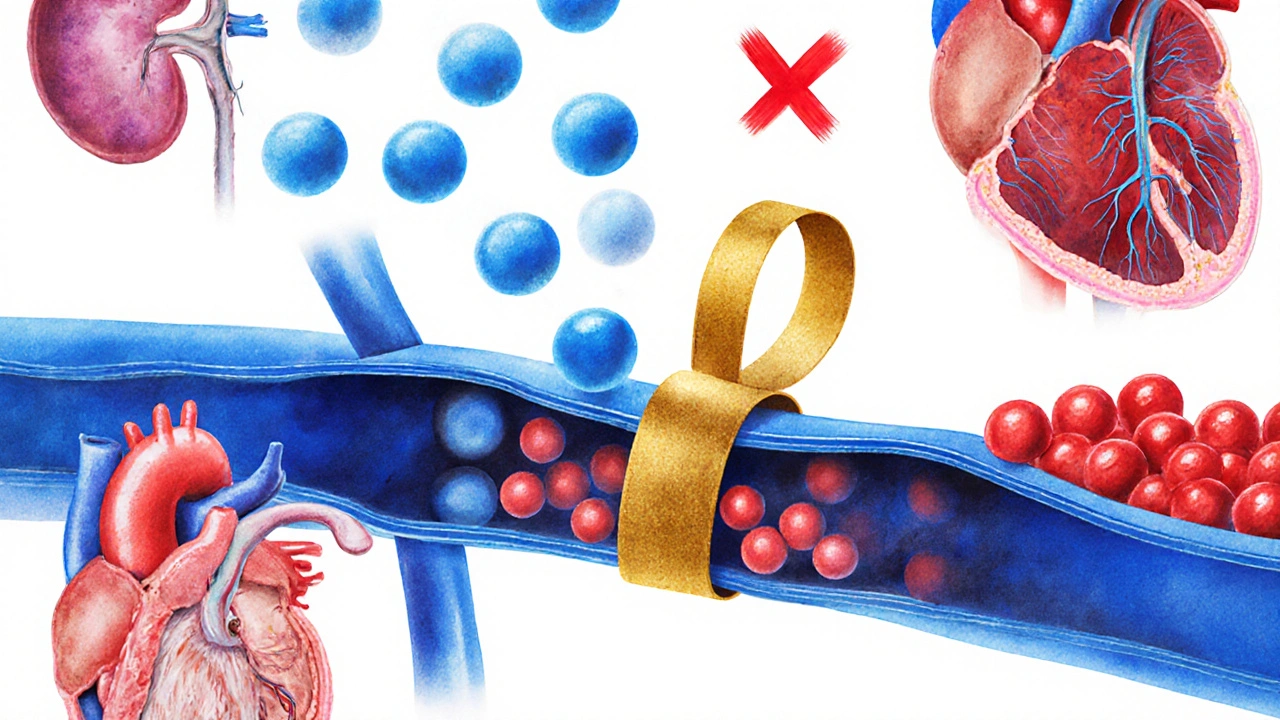
Hypernil belongs to the ACE‑inhibitor class, which blocks the conversion of angiotensin I to angiotensin II-a potent vasoconstrictor. By keeping angiotensinII levels low, blood vessels stay relaxed, blood pressure drops, and the heart doesn’t have to pump as hard. The drug also reduces aldosterone secretion, helping the kidneys excrete excess sodium and water. These mechanisms translate into proven benefits for Hypertension, heart‑failure management, and kidney‑disease slowdown.
Key factors to compare
When weighing Hypernil against alternatives, keep an eye on six practical dimensions:
- Efficacy: How well does the drug lower systolic and diastolic pressure?
- Dosage flexibility: Can you start low and titrate up easily?
- Side‑effect profile: Which adverse reactions are most common?
- Drug interactions: Does it clash with other meds you’re on?
- Cost & insurance coverage: What out‑of‑pocket price can you expect?
- Special population suitability: Pregnancy, elderly, or renal‑impaired patients.
Let’s see how the major alternatives measure up.
Alternative ACE inhibitors
ACE inhibitors share a core mechanism but differ in half‑life, potency, and side‑effect nuance. The three biggest competitors are:
- Enalapril - a pro‑drug converted to enalaprilat in the liver; often used for heart‑failure.
- Ramipril - noted for its long half‑life (13‑17hours) and strong evidence in post‑myocardial‑infarction care.
- Benazepril - metabolized to benazeprilat, its efficacy is comparable to lisinopril but it tends to cause fewer cough complaints.
| Drug (Brand) | Typical Dose Range | Half‑Life | Key Advantages | Common Side‑Effects |
|---|---|---|---|---|
| Hypernil (Lisinopril) | 5-40mg daily | 12hours | Once‑daily, low cost, strong evidence base | Cough, hyperkalemia, renal function rise |
| Vasotec (Enalapril) | 2.5-20mg daily | 11hours (active metabolite) | Effective in heart‑failure, can be split for titration | Cough, dizziness, elevated creatinine |
| Altace (Ramipril) | 2.5-10mg daily | 13-17hours | Proven mortality benefit after heart attack | Cough, headache, angio‑edema (rare) |
| Lotensin (Benazepril) | 5-40mg daily | 10-12hours | Lower incidence of dry cough | Hyperkalemia, hypotension, rash |
All four drugs lower blood pressure by roughly 10-12mmHg on average, so the choice often boils down to tolerability and personal health history.
AngiotensinII receptor blockers (ARBs) as alternatives
For patients who can’t tolerate the lingering cough that some ACE inhibitors cause, ARBs are the go‑to backup. They block the same downstream receptor without interfering with bradykinin metabolism, which is why the cough rate is dramatically lower.
- Losartan - the first ARB on the market; modest blood‑pressure drop, also approved for protecting kidneys in diabetes.
- Valsartan - slightly more potent than losartan, often combined with a thiazide diuretic for resistant hypertension.
Both ARBs share a similar dosing convenience (once daily) and have side‑effects limited to dizziness, hyperkalemia, and rare angio‑edema. Cost is generally a bit higher than generic ACE inhibitors, but many insurance plans cover them similarly.
Cost and insurance landscape in 2025
Pricing can swing wildly based on insurance tier and pharmacy network. As of October2025, average wholesale prices (AWP) for a 30‑day supply are:
- Hypernil (Lisinopril) - $4.20
- Enalapril - $5.30
- Ramipril - $6.10
- Benazepril - $5.80
- Losartan - $8.40
- Valsartan - $9.00
Most Medicare PartD and major private plans treat the generic ACE inhibitors as Tier1, meaning a $0-$5 co‑pay, while ARBs land in Tier2 or3, pushing co‑pays to $10-$30. If you have a high‑deductible health plan, the out‑of‑pocket difference can widen, so it pays to check your formulary before settling on a brand.
How to decide: a quick decision tree
- Do you have a history of ACE‑inhibitor cough? If yes, skip Hypernil and consider an ARB like Losartan.
- Are you pregnant or planning pregnancy? ACE inhibitors and ARBs are contraindicated; discuss alternatives such as methyldopa with your provider.
- Is kidney function (eGFR) below 30ml/min? Choose a lower starting dose of Hypernil or switch to an ACE inhibitor with more renal‑friendly data, like Ramipril.
- Do you need a cheap, once‑daily pill? Hypernil wins on price and convenience.
- Is cardiovascular mortality reduction after a heart attack a priority? Ramipril has strong trial evidence (HOPE) supporting that benefit.
Use this flow to have a focused conversation with your clinician; the right choice is rarely a one‑size‑fits‑all.

Common pitfalls and how to avoid them
- Starting dose too high: Jumping straight to 40mg of Hypernil can cause a sudden BP drop, leading to dizziness or fainting. Begin at 5-10mg unless you’re already on a stable ACE inhibitor.
- Ignoring potassium levels: ACE inhibitors and ARBs raise serum potassium. If you’re on a potassium‑sparing diuretic or a high‑potassium diet, schedule labs every 2-4weeks after initiation.
- Missing the cough cue: A mild, dry cough may signal bradykinin buildup. Don’t ignore it-switching to an ARB often resolves the symptom within weeks.
- Renal function oversight: Patients with chronic kidney disease require dose adjustments and closer monitoring of creatinine. A rise of >30% after starting Hypernil warrants a dose cut.
- Assuming all ACE inhibitors are interchangeable: While they share a class, differences in half‑life and metabolic pathways affect dosing schedules and drug‑interaction risk (e.g., enalapril with NSAIDs).
Bottom line
Hypernil (Lisinopril) remains a solid first‑line option for most people battling hypertension because it’s cheap, effective, and backed by decades of data. If you’re prone to cough, have specific heart‑failure needs, or require a drug with proven post‑MI mortality benefit, alternatives like Ramipril or an ARB such as Losartan may be a better fit. The key is to line up efficacy, side‑effect tolerance, cost, and any comorbid conditions with your personal health goals. Talk to your clinician, bring your lab results, and use the comparison points above to make an informed decision.
Frequently Asked Questions
Can I switch from Hypernil to an ARB without a washout period?
Yes. Because both drug classes act on the renin‑angiotensin system, a short gap (24‑48hours) is enough to avoid overlapping effects. Your doctor will usually schedule a lab draw a week after the switch to check potassium and creatinine.
Why do some people develop a persistent cough on Hypernil?
ACE inhibitors block the breakdown of bradykinin, a peptide that can irritate the airway lining. In about 5‑10% of patients, this irritation shows up as a dry cough that doesn’t improve with cough suppressants. Switching to an ARB eliminates the bradykinin buildup.
Is Hypernil safe for people with diabetes?
Absolutely. In fact, ACE inhibitors like Hypernil are recommended for diabetic patients because they protect the kidneys by reducing intraglomerular pressure. Just monitor blood‑sugar and kidney labs regularly.
How often should I have my blood pressure checked after starting Hypernil?
Check your pressure at least twice a week for the first two weeks, then settle into a weekly routine. If you notice readings below 90/60mmHg, contact your provider-dose reduction might be needed.
Can I take Hypernil together with a potassium supplement?
Usually not without medical supervision. Both Hypernil and potassium supplements raise serum potassium, which can lead to dangerous arrhythmias. Your doctor may order a serum potassium test before approving the combo.

 Benzodiazepines: Benefits, Risks, and Dependence Potential
Benzodiazepines: Benefits, Risks, and Dependence Potential
 Buy Cheap Generic Amoxicillin Online - Safe Guide 2025
Buy Cheap Generic Amoxicillin Online - Safe Guide 2025
 Serum Sickness-Like Reactions to Antibiotics: What Parents and Doctors Need to Know
Serum Sickness-Like Reactions to Antibiotics: What Parents and Doctors Need to Know
 Nebulizers vs. Inhalers: Which One Really Works Better for Asthma and COPD?
Nebulizers vs. Inhalers: Which One Really Works Better for Asthma and COPD?
 What Is a Mentat? The Real‑World Meaning Behind Dune’s Human Computers
What Is a Mentat? The Real‑World Meaning Behind Dune’s Human Computers
Summer Medina
October 8, 2025 AT 21:47Look folks, when you talk about Hypernil you gotta remember that this is a proudly American made ACE inhibitor that has been around longer than most of our modern gadgets, and it's still the go‑to for many doctors because it doesn't cost an arm and a leg, it just works and it does it once a day which is perfect for people who forget to take meds.
Now, when comparing it to the other ACE inhibitors you see that the half‑life is about twelve hours which is just right to keep the pressure down over night without the spikes you get from shorter acting stuff.
The side‑effect profile is pretty classic – cough, a little potassium rise and some kidney numbers to watch – but that’s the same story across the class.
What really sets Hypernil apart in my opinion is the sheer amount of data behind it, hundreds of trials that have proven it reduces mortality in heart failure and protects the kidneys in diabetic patients.
If you’re on a budget the price tag of four dollars for a month’s supply is unbeatable compared to the ten‑plus dollars you pay for some of the newer ARBs.
People tend to overlook the fact that it can be titrated from five up to forty milligrams, giving doctors flexibility for almost any stage of hypertension.
All in all, it’s a solid, no‑nonsense choice for the average American dealing with high blood pressure.
And yes, if you start feeling that annoying cough just know you’ve got options, don’t just suffer in silence.
Joshua Brown
October 9, 2025 AT 20:00When selecting an ACE inhibitor, the first factor to evaluate is the efficacy measured by the average reduction in systolic pressure – Hypernil typically achieves a 10‑12 mmHg drop, which is comparable to Enalapril and Ramipril.
Next, consider the dosing convenience; a once‑daily regimen improves adherence, and Hypernil’s 5‑40 mg range allows fine‑tuning without the need for split tablets.
Don’t forget to monitor serum potassium and creatinine within the first month, especially if the patient is on a potassium‑sparing diuretic.
Cost‑effectiveness is also crucial – at roughly $4.20 per thirty‑day supply, Hypernil is a tier‑1 drug for most insurers, keeping out‑of‑pocket expenses low.
If the patient develops a persistent dry cough, switching to an ARB such as Losartan eliminates the bradykinin‑mediated irritation, while preserving blood‑pressure control.
andrew bigdick
October 10, 2025 AT 18:13Hey everyone, if you’re new to ACE inhibitors just remember they all block the same pathway, so Hypernil works just as well as the others for most folks.
What matters is how you feel on the medication – if the cough is a deal‑breaker, there’s an easy swap to an ARB.
Talk to your clinician about your lifestyle and any other meds you’re taking, and they’ll help you find the right fit.
Shelby Wright
October 11, 2025 AT 16:27Some people act like Hypernil is the holy grail of hypertension therapy, but let’s be real – the cough side‑effect can be a nightmare, turning a simple pill into a nightly torment.
Meanwhile, the newer ARBs stroll in with almost no cough, yet they cost double, double, double the price, which makes you wonder who’s really benefitting here.
If you love drama, imagine the irony of paying extra for a “cough‑free” drug that still gives you dizziness and rare angio‑edema.
Bottom line: every drug has its dark side, don’t worship any of them blindly.
Ryan Wilson
October 12, 2025 AT 14:40It’s important to recognize that prescribing medication isn’t just about numbers on a chart; it’s about the patient’s overall well‑being and moral responsibility to avoid unnecessary harm.
Choosing Hypernil simply because it’s cheap can feel like cutting corners, especially when alternatives might better suit an individual’s kidney function or risk of cough.
Doctors should weigh the ethical implications of side‑effects against cost, rather than assuming a one‑size‑fits‑all approach.
Encouraging patients to discuss their preferences openly also respects their autonomy and promotes shared decision‑making.
Ultimately, the right choice aligns efficacy, safety, and fairness.
EDDY RODRIGUEZ
October 13, 2025 AT 12:53Listen up, folks! Hypernil can be your ally in the battle against high blood pressure, but you’ve got to give it a fair shot – start low, monitor, and stay consistent.
If the cough shows up, don’t throw in the towel; switch to an ARB and keep crushing those BP numbers.
Remember, consistency beats perfection – taking your pill every day is the real victory.
And keep your eyes on the prize: a healthier heart, fewer doctor visits, and more freedom to live life on your terms.
Christopher Pichler
October 14, 2025 AT 11:07From a pharmacodynamic standpoint, Hypernil’s inhibition of angiotensin‑converting enzyme yields a predictable reduction in systemic vascular resistance, which is why it remains a first‑line agent in most guidelines.
Clinically, the trade‑off is the bradykinin‑mediated cough, a side‑effect that some patients find delightful – obviously not.
Economically, the generic status translates to tier‑1 formulary placement, a real boon for cost‑conscious payers.
Comparatively, ARBs such as Losartan sidestep the cough issue but suffer from a marginally higher out‑of‑pocket cost, a classic example of “you get what you pay for.”
So, if you enjoy paying more for the same blood‑pressure drop, go ahead and pick the ARB; otherwise, stick with the tried‑and‑tested ACE inhibitor.
VARUN ELATTUVALAPPIL
October 15, 2025 AT 09:20Hypernil-also known as Lisinopril-offers a once‑daily dosing schedule; this is particularly advantageous for patients who have difficulty adhering to multiple daily doses!
However, the potential for a dry cough, hyperkalemia, and renal function changes requires vigilant monitoring, especially in individuals with pre‑existing kidney disease.
Cost‑effectiveness remains a strong point, with the generic formulation typically priced below $5 for a 30‑day supply.
April Conley
October 16, 2025 AT 07:33Hypernil is cheap and works well.
Sophie Rabey
October 17, 2025 AT 05:47Great news, everybody-if you love paying pennies for your blood pressure meds, Hypernil is here to save the day while also giving you a charming cough as a bonus feature.
On the bright side, the drug’s kidney‑protective properties are solid, so diabetics can breathe easier-actually, maybe not breathe, because of that cough.
Just remember to check potassium levels, because who doesn’t enjoy a little extra electrolyte drama?
All in all, it’s a solid starter drug for the budget‑conscious and cough‑tolerant alike.
Bruce Heintz
October 18, 2025 AT 04:00Totally agree, staying consistent is key! 😊
richard king
October 19, 2025 AT 02:13The paradox of Hypernil lies in its dual nature – a guardian of the heart yet a potential harbinger of a relentless cough that haunts the night.
It embodies the age‑old dilemma: to endure a fleeting discomfort for the promise of longevity, or to forsake the comfort of silence for the certainty of health.
In the quiet moments when you inhale, the drug whispers of reduced mortality; in the exhale, it reminds you of the price you pay.
Thus, the choice becomes a meditation on what we value more – the fleeting breath of ease or the sustained rhythm of life.
Each patient must weigh the scales of benefit and burden, for medicine is as much philosophy as it is science.
And in that weighing, the true healer is the one who listens to both the heart and the cough.
Dalton Hackett
October 20, 2025 AT 00:27When I first encountered Hypernil in the clinic, I was immediately struck by the sheer volume of clinical evidence supporting its use across a broad spectrum of cardiovascular conditions, ranging from uncomplicated hypertension to heart failure with reduced ejection fraction.
One of the most compelling aspects of lisinopril, the active ingredient in Hypernil, is its long half‑life of approximately twelve hours, which permits once‑daily dosing without the peaks and troughs associated with shorter‑acting agents.
The pharmacokinetic profile also ensures stable plasma concentrations, thereby minimizing the risk of sudden blood‑pressure spikes that could precipitate adverse events.
From a therapeutic standpoint, the drug’s ability to inhibit the conversion of angiotensin I to angiotensin II not only reduces vasoconstriction but also diminishes aldosterone secretion, leading to decreased sodium and water retention.
This dual mechanism contributes significantly to its renoprotective effects, especially in patients with diabetes mellitus, where hyperfiltration can be mitigated.
Nevertheless, clinicians must remain vigilant for the well‑documented side‑effect of a dry cough, which is thought to arise from increased bradykinin levels in the respiratory tract.
In practice, I have observed that up to ten percent of patients discontinue therapy solely due to this cough, prompting a switch to an angiotensin‑II receptor blocker when appropriate.
Another consideration is the potential for hyperkalemia, particularly in individuals concurrently using potassium‑sparing diuretics or those with compromised renal function.
Regular monitoring of serum potassium and creatinine at baseline and after dose adjustments is therefore essential to avert dangerous electrolyte imbalances.
Cost‑effectiveness remains a hallmark of Hypernil; the generic formulation typically costs less than five dollars for a thirty‑day supply, placing it in Tier 1 formularies for most insurance plans.
This affordability contrasts sharply with many newer ARBs, which can exceed eight dollars for an equivalent supply, creating a financial burden for patients without comprehensive coverage.
From a prescriber’s perspective, the flexibility to titrate from five to forty milligrams allows for individualized therapy, accommodating patients with varying degrees of hypertension severity.
In addition, the once‑daily regimen simplifies adherence, a critical factor given that medication non‑compliance is a leading cause of uncontrolled blood pressure in real‑world settings.
While the drug is contraindicated in pregnancy due to teratogenic risks, it remains a cornerstone of therapy for the majority of adult patients, especially those with concomitant heart or kidney disease.
In summary, Hypernil offers a robust balance of efficacy, safety, and cost, but providers must tailor its use to each patient’s clinical profile, monitoring for cough, potassium elevation, and renal function changes to optimize outcomes.