Hospitals don’t just stock any drug that’s available. Every medication you receive - even a simple generic pill - has gone through a strict, evidence-based review process before it ever reaches your bedside. This process is called a hospital formulary, and it’s the backbone of how hospitals decide which drugs to use, especially when it comes to generic medications.
What Exactly Is a Hospital Formulary?
A hospital formulary is a living list of approved medications. It’s not a static catalog you print once a year. It’s updated regularly - often quarterly - based on new clinical data, cost changes, and supply issues. In U.S. hospitals, this list typically includes between 300 and 1,000 drug dosage forms. Most are closed formularies, meaning only the drugs on the list are routinely available. If a doctor wants to prescribe something off-formulary, they usually need special approval. The goal? To give patients the safest, most effective drugs at the lowest possible cost. That’s not just a slogan - it’s the official definition from the American Society of Health-System Pharmacists (ASHP). And it’s why generic drugs make up the vast majority of prescriptions in hospitals: they’re just as effective as brand-name drugs, but cost a fraction of the price.How Do Hospitals Pick Which Generic to Use?
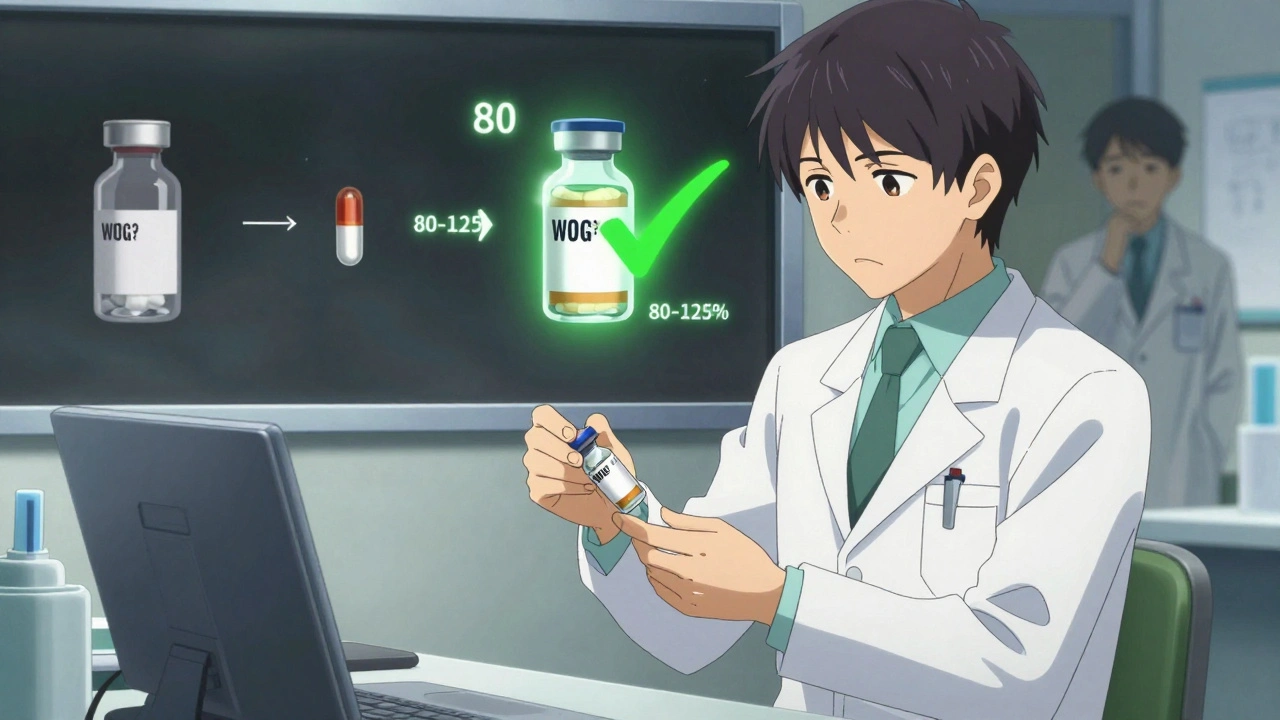
It’s not enough that a generic drug is FDA-approved. That’s just the starting point. Every generic drug must be listed in the FDA’s Orange Book as therapeutically equivalent to its brand-name counterpart. That means it delivers the same active ingredient at the same strength, in the same way, and works the same way in the body - with bioequivalence within 80-125% of the original drug’s absorption rate. But hospitals go further. A Pharmacy and Therapeutics (P&T) committee, made up of pharmacists, physicians, and sometimes economists, reviews each drug using multiple criteria:- Clinical efficacy: They look at 15-20 peer-reviewed studies per drug class. Not just any studies - high-quality randomized trials and meta-analyses.
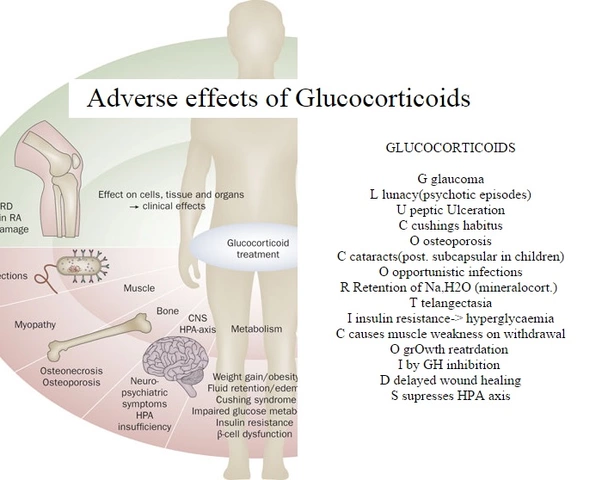
- Safety profile: They check FDA’s Adverse Event Reporting System for red flags. Even a slightly higher rate of dizziness or nausea can matter in a hospital setting.
- Cost-effectiveness: It’s not just the sticker price. They calculate total cost of care: how the drug affects length of stay, readmission rates, and complications.
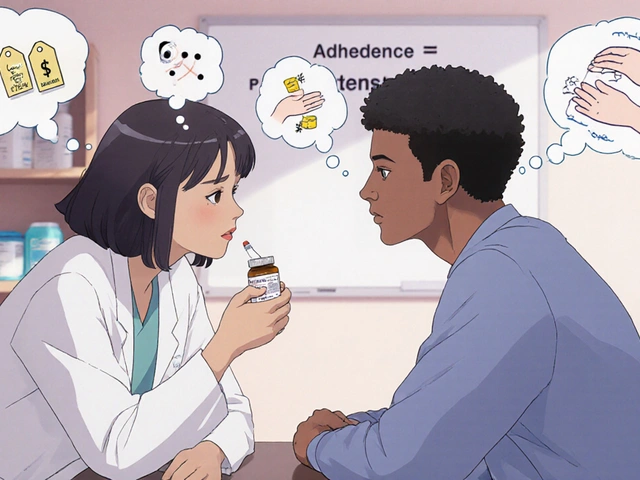
- Formulation differences: A generic pill might look different, or have a different filler. For patients on multiple meds, that can affect compliance. A pill that’s easier to swallow or less likely to cause stomach upset might win out, even if it’s slightly more expensive.
Tiers and Costs: Why Generics Are at the Bottom
Most hospital formularies use a tier system. Think of it like a pricing ladder:- Tier 1: Preferred generics - lowest cost to the hospital and patient. These are the first choice.
- Tier 2: Non-preferred generics or older brand-name drugs.
- Tier 3 and above: Newer brand-name drugs or specialty medications, often requiring prior authorization.
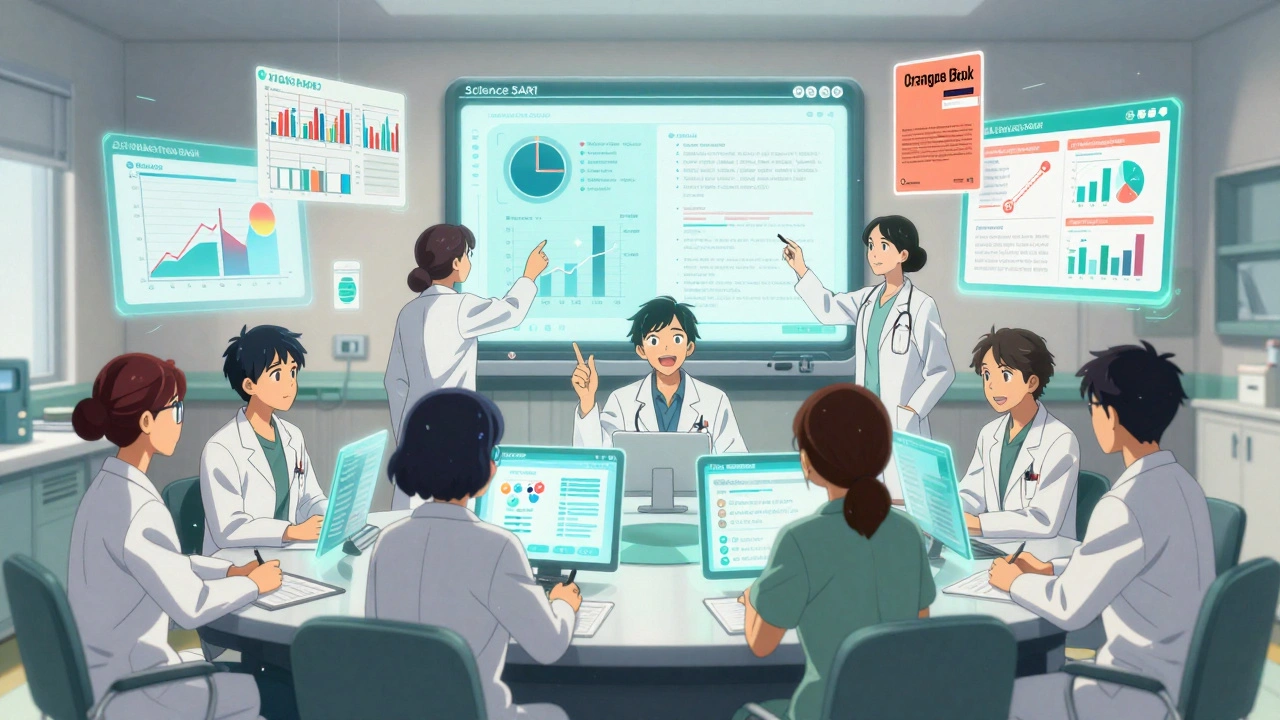
Who Decides? The P&T Committee
This isn’t a group of administrators making decisions over coffee. P&T committees are highly structured. They typically have 12-15 members: board-certified pharmacists (BCPP), physicians with specialty training, and healthcare economists. Every member must complete annual conflict-of-interest training - no pharmaceutical reps can influence votes. When a new generic drug is proposed, the manufacturer or a hospital clinician submits a dossier. This includes:- Full clinical trial data
- Pharmacokinetic studies
- Comparative cost analysis
- Real-world usage data
Real Problems, Real Solutions
It’s not all smooth sailing. Hospitals face real challenges:- Drug shortages: In 2022, 268 generic drugs were in short supply. When one generic runs out, the formulary team must quickly switch to another approved alternative - or risk delays in treatment.
- Physician resistance: Some doctors are used to prescribing a specific brand. When the formulary changes, they push back. A 2021 AMA survey found 32% of physicians felt formulary restrictions affected patient care.
- Workflow disruptions: Nurses reported 73% of medication errors during formulary transitions, often because a pill looked different or a dose changed slightly.

Industry Influence and Hidden Biases
Pharmaceutical companies still try to sway decisions. Dr. Jerry Avorn from Harvard documented how drug reps use detailing - personalized marketing visits - to promote their products, even when cheaper, equally effective generics exist. Even with conflict-of-interest policies, subtle influence can linger. That’s why many hospitals now rely on independent analysts like the Institute for Clinical and Economic Review (ICER). ICER’s cost-effectiveness reports are used by 65% of large hospital systems. They don’t take money from drugmakers. Their evaluations are transparent, peer-reviewed, and focused on patient outcomes, not profits.The Future: Total Cost of Care and Personalized Medicine
The biggest shift in formulary decisions isn’t about price anymore - it’s about total cost of care. Hospitals are using predictive analytics to model how a drug choice affects readmissions, emergency visits, and long-term complications. For example, a cheaper generic might seem better - but if it causes more GI side effects, leading to more ER visits, the real cost is higher. Now, hospitals track that. Another emerging trend? Pharmacogenomics. Some academic hospitals are starting to use genetic testing to guide formulary choices. If a patient has a gene variant that makes them metabolize a drug poorly, the formulary might automatically prefer a different generic - even if it’s slightly more expensive. This isn’t common yet, but 18% of major medical centers are piloting it. The 2022 Inflation Reduction Act will also push hospitals to align more closely with Medicare’s evolving drug policies. By 2028, the Agency for Healthcare Research and Quality predicts all Medicare-certified facilities will need formal formularies.Why This Matters to You
If you’re a patient, you might never see the formulary - but it’s why you get a $4 generic instead of a $400 brand-name drug. It’s why your blood pressure pill works just as well, but costs less. It’s why your hospital doesn’t run out of essential meds during a shortage. If you’re a healthcare worker, you know the headaches: the training, the paperwork, the pushback. But you also know the wins - the lives saved, the millions saved, the smarter care. Hospital formularies aren’t perfect. But they’re the most systematic, evidence-based way we have to ensure that everyone - no matter their income - gets the right drug at the right price.Are generic drugs really as good as brand-name drugs in hospitals?
Yes. Hospitals only include generics that are FDA-approved as therapeutically equivalent, meaning they deliver the same active ingredient in the same way and work the same way in the body. Hospitals go even further - reviewing clinical studies, safety data, and real-world outcomes. In practice, studies show no difference in effectiveness or safety between hospital-formulary generics and their brand-name counterparts.
Why do some doctors resist using generic drugs?
Some doctors are used to prescribing a specific brand and worry that switching could affect patient outcomes - even when evidence says otherwise. Others have had bad experiences with certain generic manufacturers, like inconsistent pill quality or supply issues. Formulary changes can also disrupt established routines, especially when a generic looks or tastes different. But most of these concerns are based on perception, not data.
How often are hospital formularies updated?
Academic medical centers typically review their formularies every three months. Community hospitals do it twice a year. Updates happen when new drugs become available, when a drug is recalled or has a shortage, or when new clinical evidence emerges. Urgent changes, like during a drug shortage, can be made in as little as two weeks.
Do formularies limit patient access to medications?
They can, but they’re designed to prevent unnecessary or ineffective use. If a drug isn’t on the formulary, a doctor can still prescribe it - but they usually need to justify it through prior authorization. This prevents overuse of expensive or unproven drugs. For most patients, the formulary ensures access to the best, most cost-effective options - not the most expensive ones.
What’s the difference between a hospital formulary and a Medicare Part D formulary?
Hospital formularies focus on clinical outcomes and total cost of care within an inpatient setting. They use therapeutic interchange - pharmacists can switch a drug at the point of dispensing if it’s equivalent. Medicare Part D is designed for outpatient use and prioritizes patient cost-sharing through tiered copays. Hospitals care about preventing readmissions; Medicare plans care about monthly premiums and patient satisfaction.
How do drug shortages affect hospital formularies?
Drug shortages force hospitals to temporarily remove a generic from the formulary and switch to an alternative. In 2022, 268 generic drugs faced shortages. Hospitals use pre-identified backup options and “therapeutic alternatives committees” to minimize disruption. Sometimes, they temporarily allow off-formulary drugs until the shortage ends. These decisions are made quickly - often within days - to ensure patient care isn’t interrupted.
Why do some hospitals use different generics for the same drug?
Even within the same system, affiliate hospitals might have different formularies if they have different supply chains, contracting agreements, or patient populations. But most large hospital systems now require central formulary adoption to standardize care. Differences usually come down to which generic manufacturer has the most reliable supply or best pricing at a given time.
 L-Tryptophan and Antidepressants: What You Need to Know About Serotonin Overlap and Risks
L-Tryptophan and Antidepressants: What You Need to Know About Serotonin Overlap and Risks
 What Is Medication Adherence vs. Compliance and Why It Matters
What Is Medication Adherence vs. Compliance and Why It Matters
 The Link Between Bimatoprost and Dry Eye Syndrome
The Link Between Bimatoprost and Dry Eye Syndrome
 Ginseng and Diabetes Medications: What You Need to Know About Blood Sugar Risks and Monitoring
Ginseng and Diabetes Medications: What You Need to Know About Blood Sugar Risks and Monitoring
 Dose Adjustments After Switching to Generics: When Doctors Change Medication Doses
Dose Adjustments After Switching to Generics: When Doctors Change Medication Doses
Jimmy Kärnfeldt
December 11, 2025 AT 17:04Man, I never thought about how much work goes into picking a simple pill. It’s not just ‘cheaper = better’ - it’s science, data, and real people trying to balance cost with actual health outcomes. Kinda beautiful when you think about it.
Ariel Nichole
December 12, 2025 AT 21:12Love that hospitals use real evidence and not just marketing. I’ve seen too many places go for the flashy new drug because it’s ‘trendy.’ Glad someone’s keeping it grounded.
john damon
December 14, 2025 AT 08:16So generics are just as good??? 😱 I thought they were like knockoff sneakers 🤯
Taylor Dressler
December 16, 2025 AT 05:49The P&T committee process is one of the most underappreciated systems in modern healthcare. Rigorous, transparent, and anchored in clinical outcomes - not corporate incentives. The fact that they require conflict-of-interest training and rely on independent analysts like ICER sets a gold standard. Most patients assume their meds are chosen randomly. They’re not. They’re chosen by experts who’ve read dozens of peer-reviewed papers. That’s worth knowing.
And the shift toward total cost of care? Brilliant. A $4 pill that causes three ER visits isn’t saving money - it’s costing the system more. Hospitals are finally starting to think like actuaries instead of accountants.
Pharmacogenomics is the next frontier. Imagine tailoring generics based on your DNA. It’s not sci-fi - it’s happening in pilot programs right now. The future isn’t about brand names. It’s about precision, predictability, and preventing harm before it happens.
And yes, drug shortages are a nightmare. But the fact that places like Mayo and Hopkins have built proactive backup systems? That’s resilience. That’s leadership.
This isn’t bureaucracy. It’s care, systematized.
Sylvia Frenzel
December 17, 2025 AT 11:52This is why America’s healthcare is broken. You’re telling me we spend billions on drug reviews just to save a few bucks on pills? We should be spending that money on actual doctors, not committees arguing over filler ingredients.
Courtney Blake
December 17, 2025 AT 15:10Wow. So the real villain here isn’t Big Pharma - it’s the ‘experts’ who think they know better than doctors? 😏 Let me guess, they also think your grandma’s blood pressure pill should be switched because some ‘study’ says so. Meanwhile, patients are getting confused, errors are rising, and no one’s asking what the person on the receiving end actually wants.
And don’t even get me started on ‘ICER.’ Another ivory tower group with no skin in the game deciding what lives and dies based on cost-per-QALY. Real people aren’t data points.
Lisa Stringfellow
December 18, 2025 AT 17:2592% generics? That’s not evidence. That’s corporate control. Who even decided that ‘equivalent’ means ‘good enough’? What if the placebo effect matters? What if the brand-name pill just makes people feel better? You can’t measure that in a lab. But you can measure how much money you save by switching. That’s not healthcare. That’s accounting with a stethoscope.
Kristi Pope
December 18, 2025 AT 22:29Generics aren’t just cheaper - they’re smarter. They’re the quiet heroes of the hospital. No flashy ads. No sales reps. Just science and sweat. And yeah, sometimes the pill looks different. But if it keeps you alive and out of the ER? That’s a win. No emoji needed.
matthew dendle
December 19, 2025 AT 13:25lol so the hospital committee is like a bunch of pharm nerds deciding if your blood pressure pill is cool enough to be on the list? and you call that medicine? 🤡