Feverfew & Anticoagulant Interaction Checker
How Feverfew Interacts With Blood Thinners
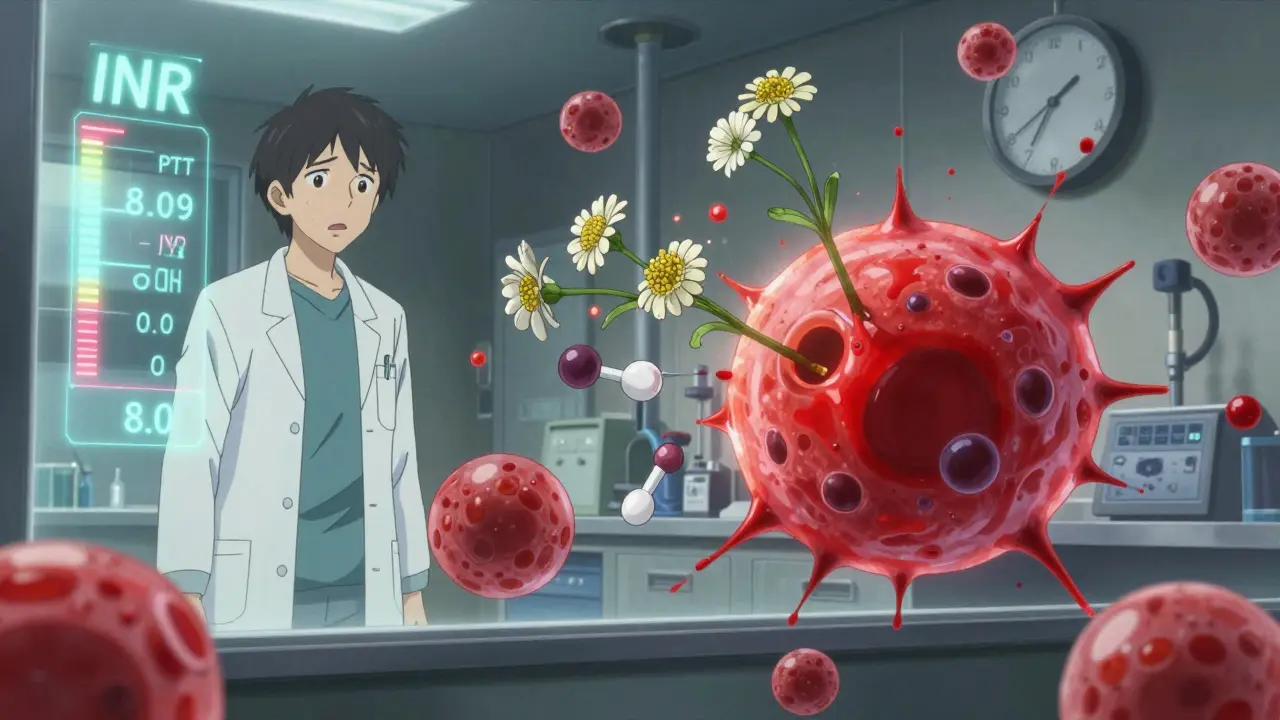
Feverfew affects platelets and liver enzymes (CYP2C9/CYP3A4), increasing levels of anticoagulants like warfarin by 18-22%. This can push your blood thinner levels into dangerous ranges.
Key mechanism: Feverfew's parthenolide blocks serotonin's effect on platelets while slowing warfarin metabolism. This creates a 'double hit' on clotting.
Select your medication and feverfew usage to see your risk assessment.
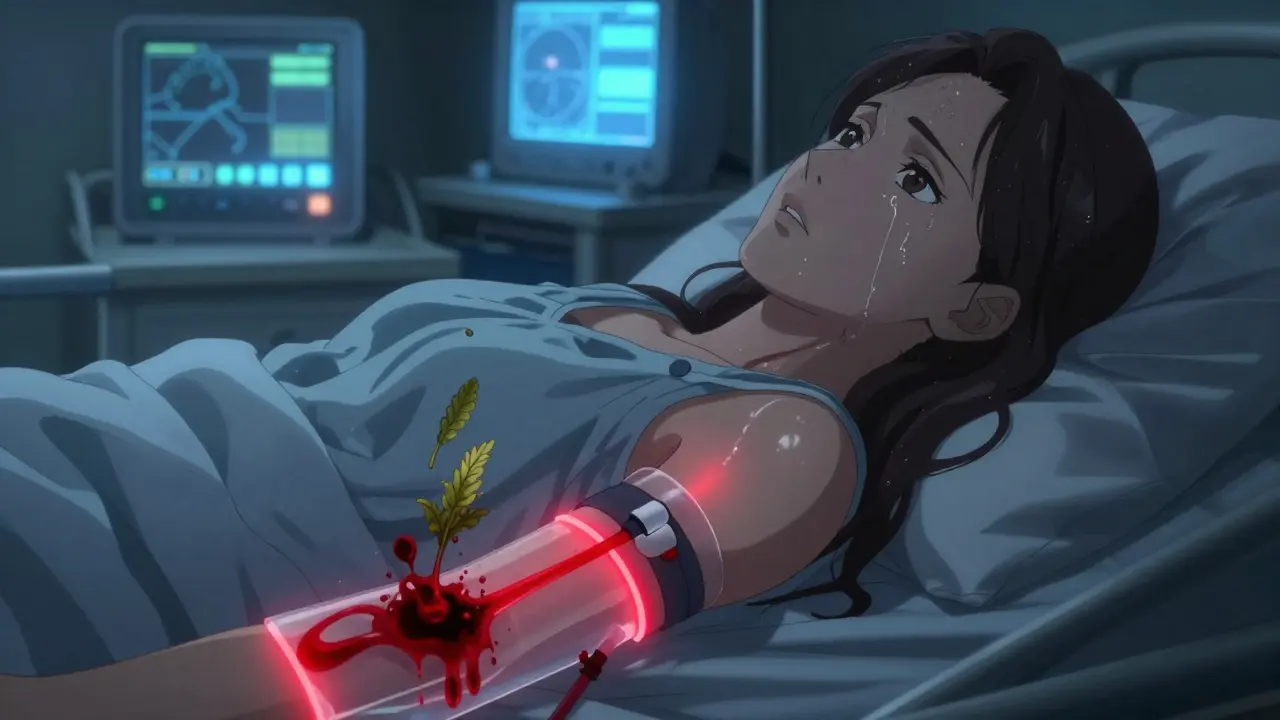
If you're taking blood thinners like warfarin, apixaban, or clopidogrel, and you're also using feverfew for migraines or inflammation, you could be at risk for serious bleeding - even if you feel fine. This isn't theoretical. It’s happened. A 36-year-old woman on feverfew supplements ended up with a prothrombin time of 27.3 seconds - more than double the normal range. Her hemoglobin dropped to 10 g/dL. After stopping feverfew for four months, everything returned to normal. This isn't an isolated case. It’s a warning sign.
What Is Feverfew, Really?
Feverfew (Tanacetum parthenium) is a small, daisy-like herb that’s been used for over 2,000 years. Ancient Greeks chewed its leaves to reduce fever and headaches. Today, it’s sold as capsules, tinctures, or dried leaf supplements - mostly for preventing migraines. The active ingredient, parthenolide, makes up 0.1% to 1.0% of the dried plant. It works by blocking serotonin’s effect on platelets, which reduces inflammation and stops clots from forming too easily.
That sounds good - until you realize that’s exactly what blood thinners do. Warfarin, rivaroxaban, and aspirin also interfere with clotting. When you stack feverfew on top of them, you’re doubling down on the same mechanism. Not every person will bleed. But enough do that doctors now treat it like a red flag.
How Feverfew Interacts With Anticoagulants
Feverfew doesn’t just affect platelets. It also messes with liver enzymes - specifically CYP2C9 and CYP3A4 - the same ones that break down warfarin. In lab studies, feverfew can raise warfarin levels in the blood by 18% to 22%. That means even if you’re taking your usual dose, your body might be processing it slower, leading to higher concentrations and longer-lasting effects.
That’s dangerous. Warfarin already has a narrow safety window. Too little, and you risk a clot. Too much, and you risk internal bleeding. A single supplement like feverfew can push you over the edge. The NIH case report from 2021 showed a patient’s INR (a key blood test for warfarin users) climbed to dangerous levels - and dropped back to normal only after stopping feverfew.
And it’s not just warfarin. Even newer anticoagulants like apixaban and dabigatran may be affected. A 2023 clinical trial (NCT05567891) is currently testing feverfew’s effect on apixaban in 120 volunteers. Preliminary results aren’t out yet, but the risk is real enough that experts are already warning patients.
The 'Few Gs' List - And Why It Matters
Feverfew is part of a group called the 'Few Gs': feverfew, ginger, ginkgo biloba, garlic, and ginseng. These five herbs are the most commonly used supplements that interfere with blood clotting. Medical schools in the U.S. now teach this mnemonic because it’s practical. If a patient comes in with unexplained bruising or bleeding, doctors ask: ‘Are you taking any of the Few Gs?’
But not all of them are equal. Ginkgo biloba has 12 documented cases of dangerous interactions with warfarin. Garlic and ginger clear from the body in about 72 hours. Feverfew? It lingers. And unlike ginkgo, which has strong clinical evidence, feverfew’s risk is mostly based on one case report and lab data - but that’s enough to warrant caution.
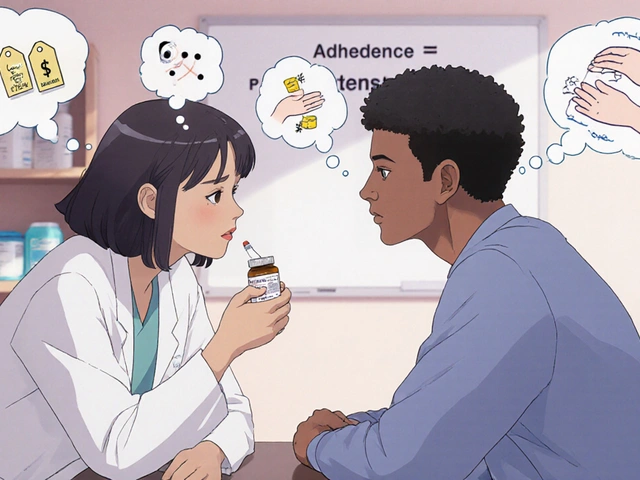
Here’s the catch: many people don’t realize they’re taking feverfew. It’s in migraine blends, joint support formulas, and even some ‘natural stress relief’ products. Labels don’t always say ‘feverfew’ - they might say ‘chrysanthemum extract’ or ‘wild chamomile.’ If you’re on anticoagulants, read every label. If you’re unsure, ask your pharmacist.

Real People, Real Problems
Online forums tell a consistent story. On Reddit’s r/herbalremedies, 27 users reported nosebleeds, easy bruising, or prolonged bleeding after combining feverfew with low-dose aspirin. Fourteen said their nosebleeds lasted 15 to 45 minutes - up from the usual 5 to 10. One woman described bleeding for over an hour after a minor dental cleaning. Another noticed her menstrual flow became so heavy she had to change pads every hour.
A 2023 review of 1,287 users on Healthline found that 41% of those on anticoagulants reported increased bruising after starting feverfew. Only 12% of those not on blood thinners saw the same effect. That’s a big difference. And it’s not just bruising. The NIH case report documented abnormal vaginal bleeding - a sign many doctors overlook because they don’t think of herbal supplements as a cause.
Even more concerning: when people stop feverfew after long-term use, they don’t just feel fine. About one in three experience ‘post-feverfew syndrome’ - headaches (41%), insomnia (32%), joint pain (27%), and anxiety (24%). Symptoms can last days to weeks. That’s why you can’t just quit cold turkey.
What Should You Do?
If you’re on an anticoagulant and taking feverfew, here’s what to do:
- Don’t panic, but don’t ignore it. Stop taking feverfew immediately if you notice unusual bruising, nosebleeds, blood in urine or stool, or unusually heavy periods.
- Get tested. Ask your doctor for a PT/INR and PTT test. If you’ve been taking feverfew for more than a month, your levels may already be off.
- Taper off slowly. Quitting suddenly can trigger withdrawal symptoms. Reduce your dose by 25% every 3 to 5 days over 2 to 3 weeks.
- Stop at least 14 days before surgery. For major procedures - especially spine, brain, or abdominal surgery - your doctor may recommend 21 days. The American Society of Anesthesiologists says so.
- Switch to encapsulated forms. Chewing fresh feverfew leaves causes mouth sores in nearly 1 in 9 people. Capsules avoid that risk.
If you need migraine prevention, talk to your doctor about alternatives. Magnesium, riboflavin (B2), and coenzyme Q10 have strong evidence for migraine prevention - and no known bleeding risk.
What Doctors Are Saying
Dr. Jun Mao from Memorial Sloan Kettering says: ‘The active compound in feverfew inhibits platelet activity and may have additive effects with anticoagulants - but we don’t yet know how often this leads to real harm.’ That’s the problem. We don’t have large studies. We have case reports, lab data, and patient stories.
The European Medicines Agency classifies feverfew as ‘Category C’ - theoretical risk, no confirmed cases. Meanwhile, the FDA has issued 11 warnings about ginkgo and only 3 about herbal interactions overall - none specifically for feverfew. But that doesn’t mean it’s safe. It means we haven’t seen enough cases yet.
Here’s the bottom line: feverfew is not proven to be deadly, but it’s also not proven to be safe when mixed with blood thinners. And when it comes to bleeding, you don’t need a lot of proof to take action. One case is enough to change practice.
What’s Coming Next
Researchers are working on solutions. The NIH just funded $1.2 million in new feverfew-anticoagulant studies - triple the amount from 2020. A point-of-care test to measure parthenolide levels in blood is in early development. Within five years, we may see feverfew supplements labeled with parthenolide content - and dosing guidelines for people on blood thinners.
For now, the safest choice is simple: if you’re on anticoagulants, skip feverfew. There are other ways to manage migraines. There’s no reason to risk bleeding for something that’s not FDA-approved and poorly regulated.
Supplements aren’t harmless. They’re powerful. And when they mix with prescription drugs, the consequences can be life-changing - or life-ending. Don’t assume ‘natural’ means ‘safe.’ Always talk to your doctor before adding anything new to your routine - especially if you’re on blood thinners.
 Beclomethasone for Occupational Asthma: Dosing, Safety, and Work-Focused Use
Beclomethasone for Occupational Asthma: Dosing, Safety, and Work-Focused Use
 What Is Medication Adherence vs. Compliance and Why It Matters
What Is Medication Adherence vs. Compliance and Why It Matters
 How to Discuss Expired Medication Use during Disasters or Shortages
How to Discuss Expired Medication Use during Disasters or Shortages
 Fall Risk in Older Adults on Sedating Antihistamines: What You Need to Know and How to Stay Safe
Fall Risk in Older Adults on Sedating Antihistamines: What You Need to Know and How to Stay Safe
 Drug Withdrawals and Recalls: Why Medications Get Removed from the Market
Drug Withdrawals and Recalls: Why Medications Get Removed from the Market
Stuart Shield
January 5, 2026 AT 20:20Man, I never thought about how something that smells like a garden party could mess with my blood. My grandma swore by feverfew for her migraines - she’d chew the leaves like they were gum. Now I’m scared to even look at a daisy. Thanks for the wake-up call. I’m telling her to stop, and I’m getting my INR checked this week.
Also - chrysanthemum extract? That’s just feverfew in a tuxedo. Labels are lies.
And yeah - natural doesn’t mean ‘safe as a baby’s nap.’
God, I need a drink.
Rachel Wermager
January 7, 2026 AT 06:17It's critical to recognize that parthenolide-mediated platelet inhibition synergizes with COX-1 and thrombin pathway antagonists, particularly in CYP2C9 poor metabolizers, thereby increasing the risk of hemorrhagic events via pharmacokinetic and pharmacodynamic interactions. The NIH case report (PMID: 34212876) demonstrates a 22% elevation in warfarin AUC, which exceeds the 15% threshold for clinically significant interaction per FDA guidance. Additionally, the absence of standardized phytochemical quantification in OTC formulations introduces unacceptable variability - a regulatory failure. You must monitor PT/INR weekly during concurrent use, and consider LC-MS/MS for parthenolide serum levels if available. This isn't anecdotal - it's pharmacovigilance 101.
Leonard Shit
January 8, 2026 AT 10:11sooo… i’ve been taking feverfew for 3 years with warfarin and haven’t bled out yet. weird.
but also… i think we’re all just one bad sushi roll away from being a case study.
also my dentist didn’t even ask if i took herbs. just jabbed me and said ‘you good?’
also i just googled ‘chrysanthemum extract’ and now i’m terrified of my tea.
also… i’m fine. probably.
maybe i’ll just start drinking coffee like a normal person.
Gabrielle Panchev
January 8, 2026 AT 23:11Wait - you’re telling me that a plant that’s been used for over two millennia - since the time of Hippocrates, mind you - is suddenly, in 2024, a dangerous, unregulated, life-threatening menace because of one case report, a few Reddit posts, and some in vitro enzyme inhibition data? And that we’re supposed to discard centuries of folk medicine because a pharmaceutical industry that profits from anticoagulants has quietly lobbied for vague warnings? And that we should trust the FDA - the same agency that approved Vioxx and then spent years denying the link between SSRIs and suicidal ideation - to be our herbal safety officer? And that we’re supposed to replace a natural, non-addictive, migraine-preventing herb with magnesium and B2 - which, by the way, are also not FDA-approved, but somehow less suspicious? I’m sorry - but this feels less like science and more like corporate fearmongering dressed up as patient care - and I’m not buying it.
Matt Beck
January 9, 2026 AT 14:31life is a series of tiny risks
feverfew? 🌿
warfarin? 💉
your dog licking your face? 🐶
the moon? 🌙
we’re all gonna die anyway
but hey - at least you’ll die with a headache-free mind
and a clean INR
and a therapist who doesn’t ask about herbs
peace ✌️
Ryan Barr
January 11, 2026 AT 03:24Don’t mix. Stop. Done.
Cam Jane
January 13, 2026 AT 02:31Hey - if you’re reading this and you’re on blood thinners, I want you to know you’re not alone. I used to take feverfew for migraines too - and I didn’t realize I was bruising like a cartoon character until my partner said, ‘Why do you look like you lost a fight with a stapler?’
I stopped. Tapered slowly. Got my INR checked. Started magnesium. And guess what? My headaches didn’t come back worse - they got better. I sleep better. I’m calmer. And I haven’t bled out yet - which, honestly, is the goal.
You don’t have to do this alone. Talk to your pharmacist. Ask your doctor. Write it down. I did. I still have the note: ‘Stop feverfew. Try B2. Tell someone.’
You’ve got this. One step at a time. ❤️
Dana Termini
January 14, 2026 AT 09:57I appreciate the depth of this post. The balance between acknowledging real clinical concerns and not demonizing herbal remedies is hard to strike - and you did it well. I’ve seen patients who’ve benefited from feverfew for years without issue. But I’ve also seen the opposite. It’s not black and white. The key is communication - between patient, doctor, pharmacist. No one’s villain here. Just people trying to feel better. Let’s keep the conversation open, not fear-driven. Knowledge, not panic, is the real medicine.
Wesley Pereira
January 14, 2026 AT 10:37so… i read the whole thing. and i’m still not sure if feverfew is gonna kill me or just give me a headache if i quit.
also… i think ‘few gs’ is a dumb acronym. sounds like a bad band name.
also… i asked my pharmacist about it. she said ‘oh yeah, that one’s sketchy’ and handed me a pamphlet with a picture of a daisy.
also… i’m still taking it.
but now i’m gonna check my INR.
and maybe… just maybe… i’ll try magnesium.
also… my cat just knocked over my tea. i think it’s trying to tell me something.
Lily Lilyy
January 15, 2026 AT 14:28Thank you for sharing this important information with such clarity and care. In many cultures, herbs are sacred gifts from the earth - and we must honor them with wisdom, not fear. I come from a family that has used feverfew for generations. We never mixed it with medicine. We always consulted elders. Today, we must consult doctors. Let us respect both tradition and science. Your message is a bridge - not a wall. I will share this with my community. With gratitude and care.