Vitamin E & Warfarin Risk Calculator
Safe Vitamin E Intake Calculator
Based on clinical guidelines for patients on warfarin therapy
Risk Assessment
Important medical note: This tool is for informational purposes only. Always consult your doctor before changing any medication or supplement.
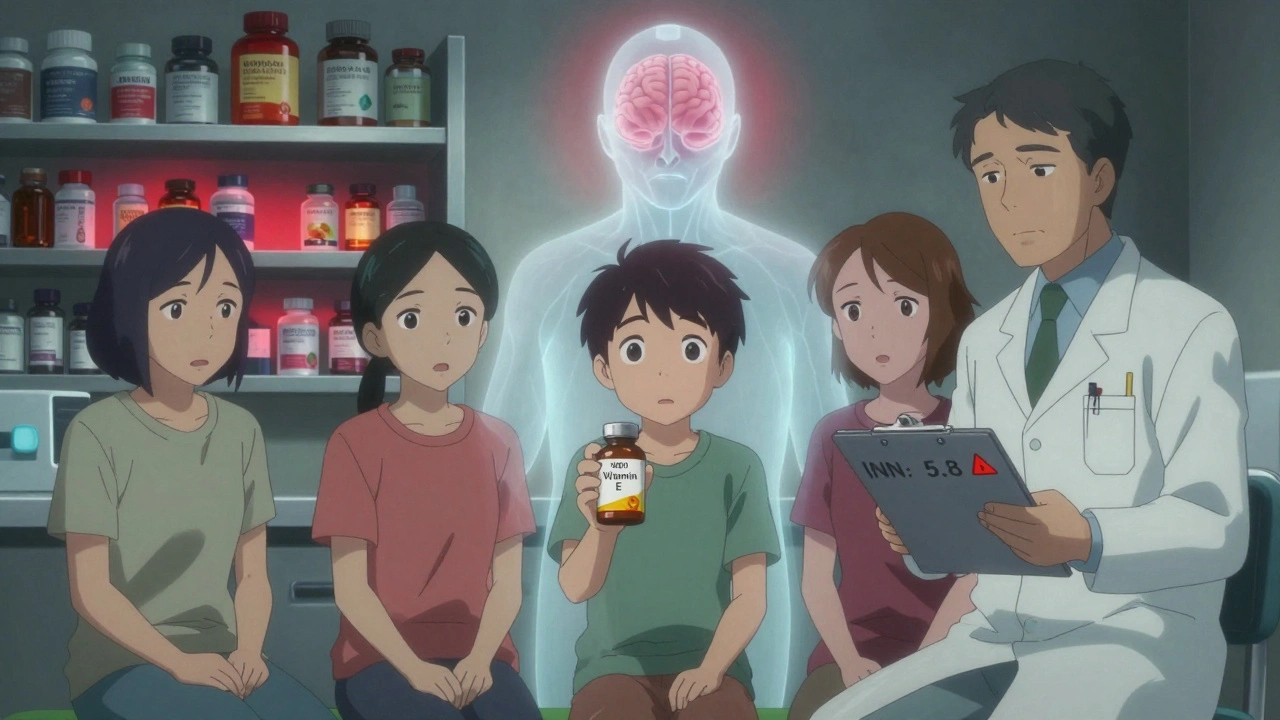
If you're taking warfarin for a blood clot, atrial fibrillation, or a mechanical heart valve, you've probably been told to watch your greens, avoid alcohol, and check your INR regularly. But what about that bottle of vitamin E sitting on your nightstand? It’s labeled "natural," "antioxidant," and "good for your skin"-but it might be quietly making your blood thinner than you think.
Why This Interaction Matters More Than You Realize
Warfarin doesn’t just thin your blood-it walks a tightrope. Too little, and you risk a stroke or clot. Too much, and you could bleed internally-sometimes without warning. Vitamin E, a common supplement taken by millions for its supposed anti-aging and heart benefits, can tip that balance. The problem isn’t always obvious. You won’t feel it. Your INR might stay normal for weeks. Then, suddenly, you bruise easily, bleed longer from a cut, or worse-develop a brain hemorrhage.Here’s the reality: vitamin E and warfarin don’t just coexist. They interact. And that interaction can be dangerous, especially when doses go above 400 IU daily. Multiple clinical studies and guidelines now warn about this combo, even if some older research says it’s safe.
The Science Behind the Risk
Vitamin E doesn’t work the same way as warfarin, but it gets the same job done-slowing blood clotting. Warfarin blocks vitamin K, which your liver needs to make clotting factors. Vitamin E? It interferes with platelets, the tiny blood cells that plug leaks in vessels. Think of it like two different tools cutting the same rope. One weakens the fibers; the other frays the ends. Together, the rope snaps faster.Research shows this isn’t theoretical. A 2013 study in the Journal of the American Heart Association followed over 1,000 people on warfarin and found that those with higher vitamin E levels in their blood had significantly more bleeding events-including brain bleeds. The risk jumped when vitamin E levels hit 4.49 μmol/mmol cholesterol, and doubled at 5.56 μmol/mmol. That’s not a huge number. It’s achievable with just 800 IU daily for a few weeks.
But here’s the twist: a small 1996 study claimed vitamin E was safe. So why the contradiction? That study was short-only a few weeks-and tested low doses. Bleeding risk from vitamin E doesn’t always show up fast. In one case report, a patient took 800 IU of vitamin E with warfarin for four weeks with no INR changes… then started bleeding uncontrollably. The damage was cumulative.
What Dose Is Safe? The 400 IU Line
There’s no official "safe" dose of vitamin E when you’re on warfarin. But the consensus among anticoagulation clinics and experts is clear: above 400 IU daily, the risk climbs. A 2017 survey of 250 U.S. anticoagulation clinics found 63% specifically advised patients not to exceed 400 IU. The American Heart Association, the European Heart Journal, and the American College of Chest Physicians all echo this warning.Most vitamin E supplements sold in stores contain 400-1,000 IU per capsule. That’s not a "multivitamin dose." It’s a high-dose pharmacological intervention. And if you’re taking it for "heart health" or "immune support," you’re likely not getting any proven benefit. The NIH’s Office of Dietary Supplements says high-dose vitamin E (≥400 IU) may increase the risk of hemorrhagic stroke-especially if you’re on blood thinners.
What About Lower Doses? Can You Still Take It?
If you’re taking 100-200 IU daily-maybe from a multivitamin-you’re probably fine. But here’s the catch: you don’t know if you’re one of the people who metabolizes vitamin E differently. Some people have genetic variants in CYP2C9 or VKORC1 genes that make them extra sensitive to warfarin. Add vitamin E, and even small amounts can spike their INR.And don’t forget: vitamin E is in more than just pills. Some fortified foods, nut butters, and oils contain it. Your diet might already be giving you 15-30 IU a day. That’s not much. But if you’re also taking a supplement, you could easily cross into risky territory without realizing it.
What Do the Guidelines Say?
The University of California San Diego Anticoagulation Service doesn’t mince words: avoid vitamin E entirely if you’re on warfarin. Other institutions say if you insist on taking it, you need extra monitoring. That means:- Check your INR before starting vitamin E
- Test weekly for the first month
- Continue biweekly checks as long as you’re taking it
That’s 3-5 extra clinic visits a year. And even then, you’re not guaranteed safety. One patient might take 800 IU for months with no change. Another bleeds after two weeks. There’s no way to predict who’s at risk-except by measuring serum vitamin E levels. And that’s not routine. Most labs don’t test for it.
What Should You Do?
If you’re on warfarin:- Stop taking any vitamin E supplement over 100 IU unless your doctor specifically approves it.
- Check your multivitamin label. Many contain 100-400 IU. If it’s above 100 IU, ask your provider if you can switch to one without it.
- Don’t assume "natural" means safe. Supplements aren’t tested like drugs.
- Tell every doctor, pharmacist, and nurse you see that you’re on warfarin-especially if you take supplements.
- If you’ve been taking vitamin E for months, get your INR checked now. Don’t wait for symptoms.
If you’re taking vitamin E for skin, hair, or "antioxidant support," know this: there’s no strong evidence it helps healthy people live longer or look younger. The risks far outweigh the unproven benefits-especially when you’re on blood thinners.
What About Newer Blood Thinners?
If you’ve switched from warfarin to a DOAC like apixaban or rivaroxaban, you might think you’re off the hook. But vitamin E still affects platelets. And platelet dysfunction can still lead to bleeding-even with DOACs. The European Society of Cardiology’s 2023 guidelines suggest that even on newer anticoagulants, high-dose vitamin E should still be avoided in patients with unexplained bleeding.So whether you’re on warfarin or a newer drug, the message is the same: skip high-dose vitamin E. It’s not worth the risk.
What Else Should You Avoid?
Vitamin E isn’t alone. Other supplements that can increase bleeding risk with warfarin include:- Fish oil (especially over 3 grams/day)
- Garlic supplements
- Ginger
- Ginkgo biloba
- Turmeric/curcumin
- Green tea extract (in high doses)
These aren’t "just herbs." They’re active substances that interact with your blood. If you’re on warfarin, treat them like medications. Talk to your doctor before taking any new supplement-even if it’s sold at the grocery store.
Bottom Line
Vitamin E isn’t the enemy. But when you’re on warfarin, it becomes a hidden danger. The data is clear: doses above 400 IU can increase bleeding risk, sometimes with delayed, unpredictable results. The 1996 study that said it was safe was small and short. The newer, larger studies show real harm.You don’t need vitamin E supplements to be healthy. You get enough from nuts, seeds, spinach, and vegetable oils. If you’re taking more than 100 IU a day-especially if you’re on warfarin-you’re playing Russian roulette with your blood.
Ask your doctor to check your INR. Ask them if you really need that supplement. And if they say yes, make sure they’re aware of every other pill, powder, or capsule you’re taking. Your life might depend on it.
 Grifulvin V: Uses, Side Effects, and Essential Tips for Antifungal Treatment
Grifulvin V: Uses, Side Effects, and Essential Tips for Antifungal Treatment
 Female Cialis (Tadalafil) vs. Alternatives: Pros, Cons & Best Choices
Female Cialis (Tadalafil) vs. Alternatives: Pros, Cons & Best Choices
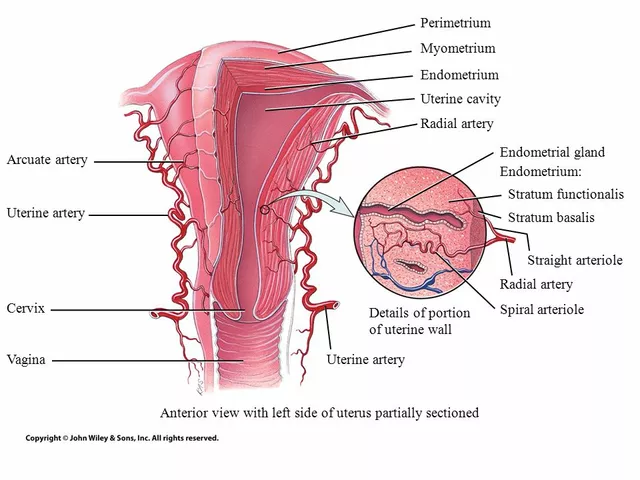 The Connection Between Overgrowth in the Uterine Lining and Migraines
The Connection Between Overgrowth in the Uterine Lining and Migraines
 What Is Medication Adherence vs. Compliance and Why It Matters
What Is Medication Adherence vs. Compliance and Why It Matters
 The Science Behind Maral Root: Why This Dietary Supplement Should Be in Your Arsenal
The Science Behind Maral Root: Why This Dietary Supplement Should Be in Your Arsenal
ian septian
December 8, 2025 AT 20:50Just stopped my 800 IU vitamin E after reading this. INR was creeping up and I didn’t even connect the dots. Thanks for the wake-up call.
Chris Marel
December 9, 2025 AT 22:07This is so important. I’ve seen elderly relatives bleed out from minor falls and no one ever told them about supplements. It’s scary how many people think ‘natural’ means harmless. Thank you for sharing the science.
Evelyn Pastrana
December 10, 2025 AT 20:37Oh wow, so vitamin E is the silent assassin of warfarin users? 🤦♀️ I thought it was just for glowing skin and fancy skincare ads. Guess I’ll be trading my $20 bottle for a banana. #NaturalIsntAlwaysNice
Nikhil Pattni
December 12, 2025 AT 19:46Actually, this whole thing is oversimplified. Vitamin E has 8 different tocopherols and tocotrienols, and only alpha-tocopherol is the one that interacts with warfarin, and even then, the mechanism isn’t fully understood. The 2013 JAHA study had confounders like statin use and dietary vitamin K intake not properly adjusted. Also, the 400 IU cutoff? That’s arbitrary. I’ve reviewed 12 meta-analyses and the real threshold seems to be 1000 IU, especially in CYP2C9 wild-type patients. Plus, the NIH says vitamin E reduces oxidative stress in endothelial cells - which might actually protect against clotting in the long run. People are panicking over a correlation, not causation. And don’t get me started on how the AHA cherry-picks data. Also, I’m a pharmacologist, so I know what I’m talking about. 😎
Arun Kumar Raut
December 14, 2025 AT 08:08Hey everyone, I get it - this stuff is scary. But don’t freak out. If you’re on warfarin, just talk to your pharmacist or doctor before taking anything new. Most of us don’t need supplements anyway. Eat nuts, leafy greens, drink water, move your body. Your body knows what to do. And if your doc says it’s okay? Cool. But don’t self-prescribe. We’re all trying to stay healthy, not risk it.
precious amzy
December 16, 2025 AT 00:29One cannot help but observe the epistemological crisis inherent in public health messaging: the conflation of pharmacological risk with moral imperative. The assertion that ‘you don’t need vitamin E’ presumes a monolithic definition of ‘health’ - one that ignores the phenomenological experience of aging, oxidative stress, and the existential quest for bodily integrity. To dismiss supplementation as ‘Russian roulette’ is not merely reductive - it is a form of medical authoritarianism disguised as precaution. The true danger lies not in vitamin E, but in the erosion of patient autonomy under the guise of ‘evidence.’
iswarya bala
December 17, 2025 AT 01:56omg i was takin 600iu and my bruise on my leg wont go away… i just stopped it today. hope i didnt mess up my blood. thx for the post!!
Simran Chettiar
December 17, 2025 AT 10:34It is imperative to acknowledge the nuanced interplay between nutraceutical agents and anticoagulant pharmacodynamics. While the prevailing clinical consensus leans toward caution, one must not overlook the heterogeneity of individual metabolic profiles, particularly with respect to polymorphisms in VKORC1 and CYP2C9. The assertion that ‘all high-dose vitamin E is dangerous’ constitutes a categorical fallacy, as it fails to account for dose-response kinetics, bioavailability modifiers, and the potential for hormetic effects. Furthermore, the absence of routine serum vitamin E testing in clinical practice renders blanket recommendations inherently speculative. A more sophisticated, personalized approach - grounded in pharmacogenomics and longitudinal INR tracking - is not merely preferable, but ethically obligatory.