Every year, over 1.3 million people in the U.S. end up in the emergency room because of unexpected reactions to their medications. Many of these cases aren’t accidents-they’re preventable. The biggest reason? Patients don’t ask the right questions. You’re not alone. Most people leave the doctor’s office with a prescription in hand but still unsure about what to expect, what to watch for, or when to call back. This isn’t about being nervous or overcautious. It’s about taking control of your health before something goes wrong.
Why asking about side effects matters
Side effects aren’t just annoying-they can be dangerous. Some are mild, like a dry mouth or a little dizziness. Others can lead to hospital stays, organ damage, or even death. The FDA reports that about 4.2% of all reported adverse drug events result in hospitalization. And here’s the kicker: half of all medication errors happen during the prescribing stage. That means the mistake starts before you even walk out of the office. The good news? When patients ask clear, specific questions, they cut their risk of preventable harm by up to 22%. That’s not a guess. It’s from a 2022 study in JAMA Internal Medicine that tracked over 12,000 patients. The ones who asked about side effects had fewer ER visits, fewer missed doses, and fewer bad reactions. You don’t need to be a medical expert. You just need to know what to ask.What’s this medicine for? (And why am I really taking it?)
Start here: “Why am I taking this?” Sounds simple, right? But a 2023 Medscape report found that over 12% of patients can’t even name their own medication correctly. That’s a red flag. If you don’t know why you’re taking it, how can you tell if it’s working-or if it’s causing harm? Ask your doctor to explain the goal. Is it to lower your blood pressure? Reduce inflammation? Prevent a stroke? Sometimes, medications are prescribed out of habit, not necessity. A 2023 Cochrane Review found that 15.2% of meds taken by older adults are continued long after they’re needed. That’s why you also need to ask: “Do I still need this?” Especially if you’ve been on it for years.What are the side effects-and which ones matter most?
This is where most people get lost. Your pill bottle lists 15 side effects. Most are rare. But you need to know which ones to watch for. Don’t just nod along. Say: “What are the most common side effects? And which ones mean I should call you right away?” The FDA defines serious side effects as those that cause death, hospitalization, disability, or birth defects. But you don’t need to wait for those. Some early signs are easy to miss:- Dizziness or lightheadedness (affects nearly 30% of people on certain blood pressure meds)
- Dry mouth or trouble swallowing (common with anticholinergics, which are found in many sleep aids, antidepressants, and allergy pills)
- Confusion or memory lapses (linked to anticholinergic burden-especially in people over 65)
- Unusual bruising or bleeding (could mean your blood thinner is too strong)
What can I do if I get side effects?
You’re not stuck with them. Many side effects can be managed-without stopping the medicine. Ask: “What can I do to reduce or avoid these side effects?” Here are real, practical fixes:- Take metformin with food to cut nausea and diarrhea (affects 20-30% of users)
- Drink water and chew sugar-free gum if you have dry mouth
- Take blood pressure meds at night if dizziness hits during the day
- Use a pill organizer to avoid double-dosing
Are there alternatives?
Not every drug is the only option. The Beers Criteria-a trusted guide for doctors treating older adults-lists 56 medications that are often inappropriate due to side effect risks. If you’re over 65, or have kidney, liver, or heart issues, ask: “Is there a safer alternative?” Sometimes, lifestyle changes can replace meds. For mild high blood pressure, weight loss and reduced salt intake can work. For depression, therapy combined with low-dose meds often works better than high doses alone. Even over-the-counter drugs matter. Diphenhydramine (found in Benadryl and many sleep aids) interacts dangerously with 17.4% of polypharmacy cases. Ask if your OTC meds are safe with your prescription.Could this interact with other meds, supplements, or food?
You’re probably taking more than one thing. The Lexicomp database tracks over 1,200 drug interactions. Some are deadly. For example:- Warfarin + ibuprofen = 2.8x higher risk of bleeding
- Statins + grapefruit juice = toxic buildup in the liver
- SSRIs + St. John’s Wort = serotonin syndrome (can be fatal)
Is there a cheaper or generic version?
Cost isn’t just a budget issue-it’s a safety issue. If a med is too expensive, people skip doses or split pills. That leads to worse outcomes. The FDA says generics are just as effective as brand names and save patients up to 89%. Ask: “Is there a generic version? Is it approved by the FDA? Is it right for me?” Some generics have different fillers that can trigger allergies or digestive issues. Don’t assume they’re all the same.Will this make my other conditions worse?
If you have diabetes, heart disease, kidney problems, or depression, your meds can make those worse. For example:- Some beta-blockers can hide low blood sugar symptoms in diabetics
- NSAIDs like naproxen can raise blood pressure and hurt kidney function
- Antidepressants can worsen glaucoma or cause urinary retention in men
When should I call you-or go to the ER?
This is the most important question of all. Most people wait too long. They think, “Maybe it’ll go away.” But some side effects need immediate action. Ask for clear red flags:- Swelling in your face, lips, or throat (sign of allergic reaction)
- Chest pain or irregular heartbeat
- Severe rash or blistering skin
- Sudden confusion, slurred speech, or weakness on one side
- Unexplained bruising or bleeding that won’t stop
How do I keep track of all this?
You can’t remember everything. Write it down. The Agency for Healthcare Research and Quality found that patients who write questions before their appointment are twice as likely to ask them. Keep a simple list:- Medication name (brand and generic)
- Dose and schedule
- Reason for taking it
- Side effects you’ve noticed
- Questions for next visit
What if my doctor dismisses my concerns?
It happens. A 2024 Medscape survey found that 41.3% of patients say their doctors brush off side effect complaints-especially with antidepressants, where sexual dysfunction affects up to 73% of users but is only discussed in 52.6% of visits. If you feel ignored, say: “I’m not trying to argue. I just want to make sure this is safe for me.” If that doesn’t work, ask for a referral to a pharmacist. Pharmacists spend 45 minutes per patient on medication reviews under Medicare’s new program. They’re trained to catch interactions, side effects, and dosing errors. In one study, patients were 87% more satisfied with pharmacist counseling than doctor visits.Final tip: Bring your whole list
Don’t just bring your current prescription. Bring everything: vitamins, supplements, OTC drugs, even herbal teas. Many people don’t think of these as “meds.” But they can be just as risky. A 2024 FDA analysis found that 63% of serious adverse events involved patients who didn’t tell their doctor about their OTC or supplement use. You’re not being difficult. You’re being smart. And you’re not alone. Over 147,000 people used a free online tool last year to build a personalized list of questions based on their meds. It cut their anxiety by over 34 points on a standard scale. The goal isn’t to scare you. It’s to help you stay in control. Medications can save your life. But only if you know how to use them safely.What should I do if I miss a dose of my medication?
Don’t double up unless your doctor says to. Call your pharmacist or doctor for specific instructions. Some meds can be taken late, others need to be skipped. Taking two doses at once can cause dangerous side effects, especially with blood thinners, diabetes drugs, or heart medications.
Can side effects show up weeks or months after starting a drug?
Yes. Some side effects are delayed. For example, statins can cause muscle damage after months of use. Antidepressants may cause sexual side effects that appear after 4-6 weeks. Bone density loss from long-term steroid use can take years. Always report new symptoms-even if they seem unrelated.
Are natural supplements safer than prescription drugs?
No. Supplements aren’t tested the same way as prescription drugs. St. John’s Wort can interfere with antidepressants, birth control, and blood thinners. Garlic and ginkgo can increase bleeding risk. Always tell your doctor what you’re taking-even if you think it’s “natural.”
Why do some side effects go away after a few days?
Your body often adjusts. Nausea, dizziness, or fatigue from new meds usually improve in 1-2 weeks as your system gets used to the drug. But if symptoms get worse, or you develop new ones like rash, swelling, or confusion, don’t wait-call your doctor.
How do I know if a side effect is normal or serious?
Ask your doctor to define “serious” for your specific drug. General signs: symptoms that interfere with daily life, get worse over time, or come with fever, swelling, chest pain, or trouble breathing. If you’re unsure, it’s better to call than wait.
Can I stop a medication if I don’t like the side effects?
Never stop suddenly without talking to your doctor. Some meds, like antidepressants or blood pressure pills, can cause dangerous withdrawal symptoms. Instead, ask for alternatives or a tapering plan. Your doctor can help you switch safely.
Should I ask about side effects even if I’ve been on the medicine for years?
Yes. Your body changes with age, weight, or new health conditions. A drug that was safe five years ago might not be now. Also, you may be taking new meds that interact with your old ones. Review your list at least once a year.

 How Azilsartan Affects Blood Pressure in Psoriasis Patients
How Azilsartan Affects Blood Pressure in Psoriasis Patients
 Where and How to Buy Folic Acid Online Safely
Where and How to Buy Folic Acid Online Safely
 Organ Donation Awareness: How It Lowers Transplant Rejection Rates
Organ Donation Awareness: How It Lowers Transplant Rejection Rates
 Zovirax Cream vs Topical Antiviral Alternatives: A Detailed Comparison
Zovirax Cream vs Topical Antiviral Alternatives: A Detailed Comparison
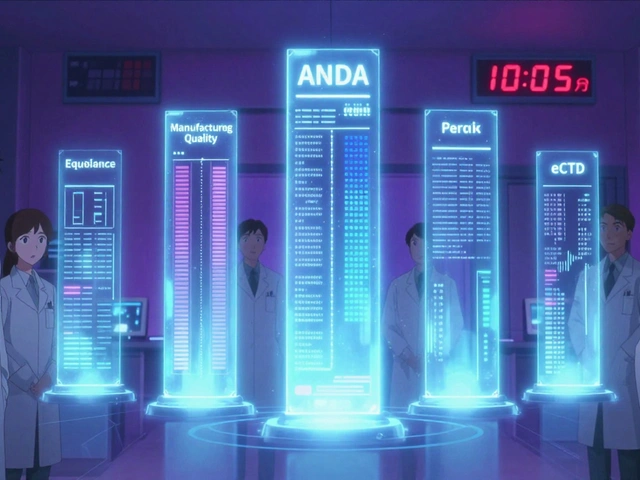 FDA Generic Drug Approval: Step-by-Step Process for ANDA Submission
FDA Generic Drug Approval: Step-by-Step Process for ANDA Submission
Christina Weber
December 21, 2025 AT 12:32Let’s be clear: if you don’t ask about side effects, you’re not a patient-you’re a liability. The FDA doesn’t list every possible reaction because they assume you’re not an idiot. But apparently, 1.3 million people are. You want to avoid the ER? Ask about anticholinergic burden. Ask about the ACB scale. Ask if your ‘sleep aid’ is secretly turning your brain to mush. If your doctor doesn’t know these terms, find one who does. This isn’t paranoia-it’s basic hygiene.
Michael Ochieng
December 22, 2025 AT 10:32I love this. My grandma took 12 meds for years and never asked a single question. She ended up in the hospital with confusion and a UTI-turns out two of her pills were causing both. Now I print out the Beers Criteria and bring it to every appointment. Pharmacists are the real MVPs. I even got my whole family to use the free question generator tool. We’re all way less anxious now. Seriously, if you’re over 50, do this. Your future self will thank you.
Dan Adkins
December 22, 2025 AT 20:43It is indeed a matter of grave concern that the majority of patients exhibit a disturbing lack of intellectual engagement regarding pharmacological interventions. The statistical prevalence of preventable adverse events, as cited, is not merely an epidemiological anomaly-it is a systemic failure of patient education. One must not presume that the physician possesses omniscience regarding polypharmacy interactions; rather, the onus of informed participation rests squarely upon the individual. I commend the author for advocating for structured inquiry, yet I must emphasize that the absence of standardized patient literacy programs remains a critical deficit in contemporary American healthcare.
Jerry Peterson
December 24, 2025 AT 04:08My dad had a bad reaction to a blood pressure med and didn’t say anything because he didn’t want to ‘bother’ the doctor. Ended up in the ER with dizziness and a fall. Now he brings a notebook. He writes down every med, every side effect, every question. It’s weird at first, but now he feels in control. I wish I’d known this years ago. Just ask. Seriously. It’s not rude-it’s smart.
Meina Taiwo
December 25, 2025 AT 23:51Always ask about the ACB scale. If you’re on 2+ anticholinergics, you’re at risk. Simple.
Southern NH Pagan Pride
December 27, 2025 AT 17:46They don’t want you to know this but the pharma companies pay doctors to push certain meds. The side effects? They bury them in tiny print. That ‘free tool’? Probably funded by Big Pharma. And why are generics always ‘just as good’? Because they’re cheaper. But the fillers? Those are the real killers. I know a guy who had a seizure because his generic had a dye that wasn’t listed. The FDA doesn’t test fillers. They don’t want you to know that.
Orlando Marquez Jr
December 29, 2025 AT 12:41The empirical evidence presented in this post is both compelling and methodologically sound. The referenced JAMA Internal Medicine study, with its cohort of over 12,000 patients, provides a robust foundation for the assertion that patient-initiated inquiry reduces adverse outcomes. Furthermore, the Kaiser Permanente data on ER visit reduction aligns with broader public health literature on patient activation. It is imperative that healthcare systems institutionalize structured patient questionnaires as a standard of care.
Jackie Be
December 29, 2025 AT 19:52OMG I just found out my sleep aid was making me forget my own kids names 😭 I was like ‘why am I zoning out during school pickup’ and then I looked up diphenhydramine and BOOM-anticholinergic overload. I stopped it and my brain came back. Like literally. I’m not crazy. I just needed to ask. THANK YOU for this post. I’m sending this to my whole family.
John Hay
December 31, 2025 AT 19:25This is exactly what we need more of. No fluff. Just facts. I used to take two blood pressure meds until I asked if I really needed both. Turns out one was prescribed for a condition I no longer had. Got cut from two pills to one. No side effects, same results. Just ask. It’s not hard.
Jon Paramore
January 1, 2026 AT 18:39For those asking about delayed side effects: statin-induced myopathy can present as fatigue or weakness after 3–6 months, often misattributed to aging. SSRI sexual dysfunction may emerge after 4–8 weeks and is frequently underreported due to stigma. The key is longitudinal monitoring-not just baseline assessment. Always request a medication reconciliation during annual reviews. The ACB score should be recalculated annually for patients >65. This isn’t optional-it’s standard of care.
Swapneel Mehta
January 3, 2026 AT 03:16I came from India where people don’t ask questions to doctors. But after my mom had a bad reaction to a common painkiller, I started asking. Now I bring a list to every appointment. It feels awkward at first, but honestly? Doctors respect it more. They don’t mind questions-they mind silence. Just be polite and clear. You’re not arguing. You’re partnering.
Stacey Smith
January 3, 2026 AT 23:08Why are we letting big pharma control our health? This is why America’s healthcare is broken. We’re being sold pills like candy while real solutions like diet and exercise get ignored. Ask your doctor? Yeah right. They’re paid to prescribe. Do your own research. Read the studies. Don’t trust the system.