IBS Management: Practical Tips and Medications That Actually Work
When you live with irritable bowel syndrome, a chronic condition causing bloating, cramping, diarrhea, or constipation without visible damage to the gut. Also known as spastic colon, it doesn't show up on scans—but it can wreck your daily life. Unlike Crohn’s or colitis, IBS isn’t about inflammation or ulcers. It’s about your gut reacting badly to things most people handle fine—stress, certain foods, or even changes in routine. The good news? You don’t have to just suffer. Real, science-backed IBS management exists, and it starts with understanding what triggers your body.
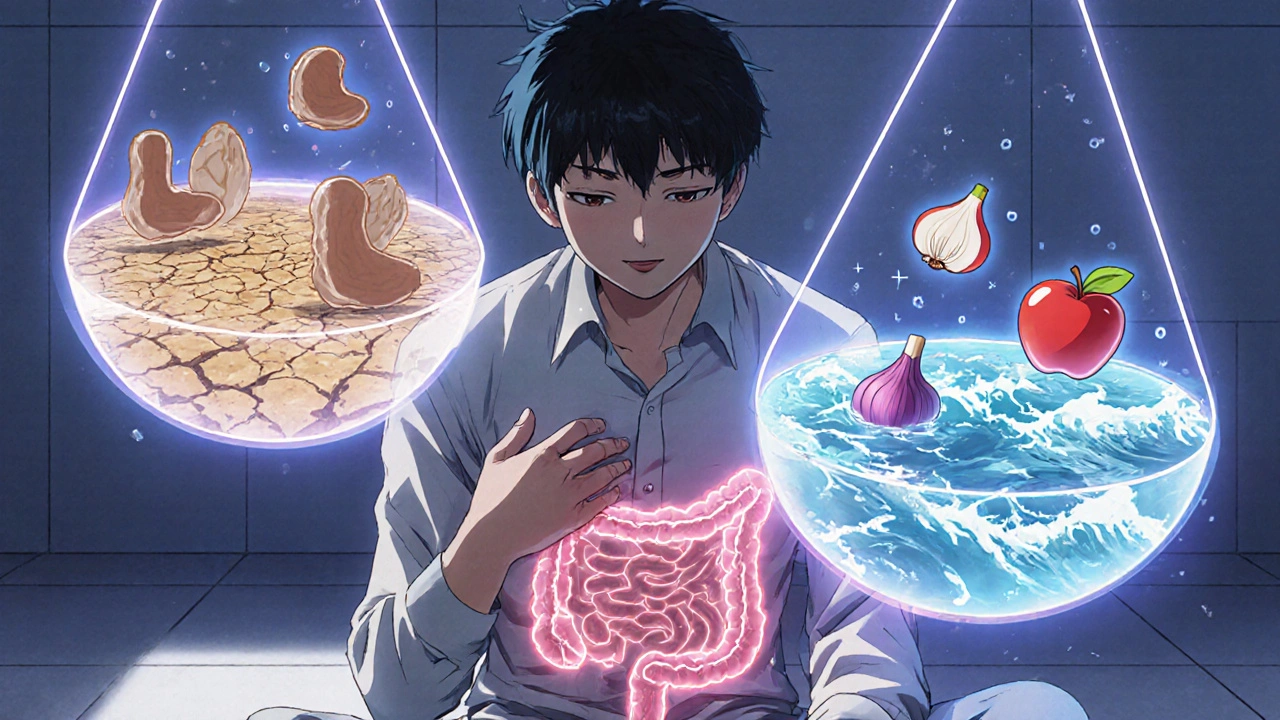
Many people try eliminating dairy or gluten, but those aren’t the only culprits. FODMAPs, a group of short-chain carbs that ferment in the gut and cause gas and bloating are a major player. Foods like onions, garlic, apples, and beans can trigger symptoms even if you’re not lactose intolerant. A low-FODMAP diet isn’t a lifelong punishment—it’s a tool. Start by cutting out high-FODMAP foods for 2-6 weeks, then slowly add them back to find your personal triggers. This isn’t guesswork; it’s detective work, and your gut is the crime scene.
Medications play a role too, but not always the one you expect. Proton pump inhibitors, drugs that reduce stomach acid might seem helpful for IBS, but they’re not a fix. In fact, they can make things worse by changing gut bacteria. Instead, targeted options like antispasmodics for cramps, laxatives for constipation, or low-dose antidepressants for nerve sensitivity can help. And yes, some people benefit from gut-directed hypnotherapy—not because it’s "all in your head," but because your brain and gut talk to each other constantly. When stress hits, your digestive system feels it.
What you eat matters, but so does when and how you eat. Eating too fast, skipping meals, or drinking caffeine on an empty stomach can all flip the IBS switch. Small, regular meals. Chew slowly. Avoid carbonated drinks. These aren’t just tips—they’re habits that change outcomes. And while supplements like peppermint oil or probiotics show promise in studies, they’re not magic pills. Find what works for you, not what worked for someone else.
There’s no one-size-fits-all cure for IBS, but there are dozens of proven ways to take back control. Below, you’ll find real comparisons of medications, insights into how food interacts with your gut, and guides on avoiding common mistakes that make symptoms worse. No fluff. No hype. Just what actually helps people live better with IBS.