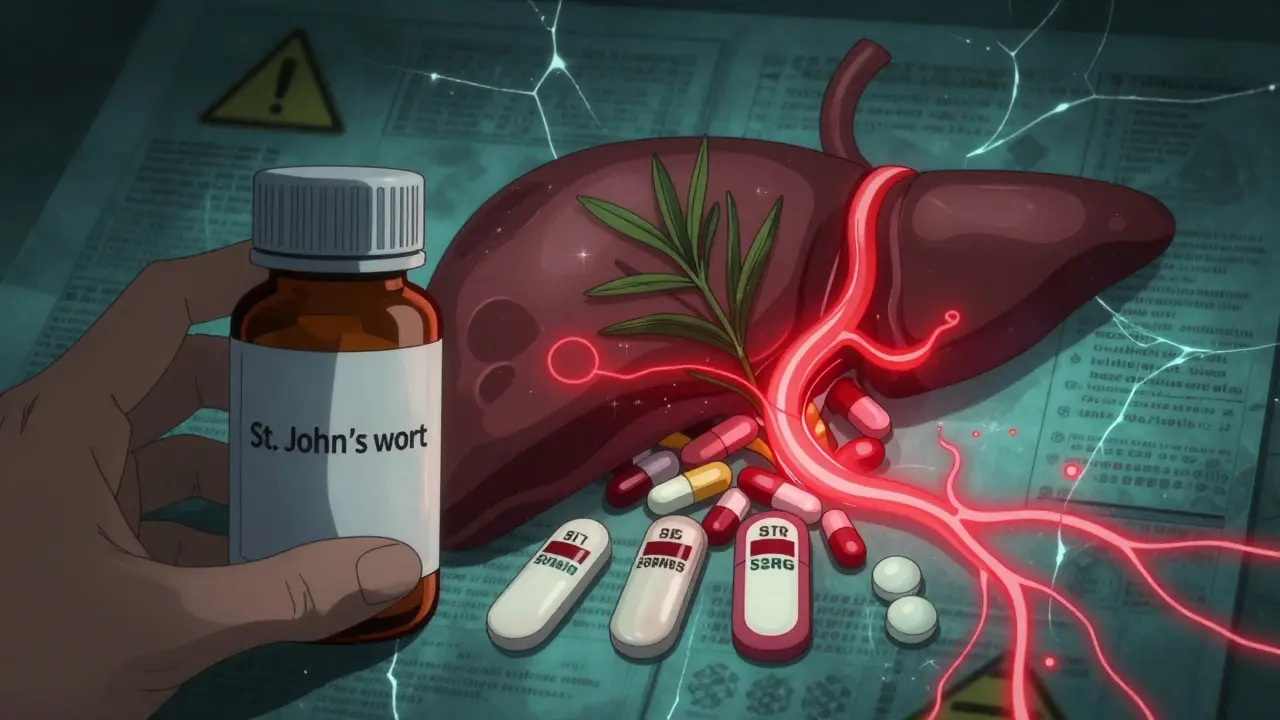
St. John’s Wort might seem harmless - it’s natural, widely available, and often marketed as a gentle fix for low mood. But here’s the truth: if you’re taking any prescription medication, this herb could be quietly undermining your treatment. It doesn’t just mix poorly with drugs - it can make them stop working entirely. And in some cases, that’s not just inconvenient. It’s dangerous.
How St. John’s Wort Changes How Your Body Processes Medications
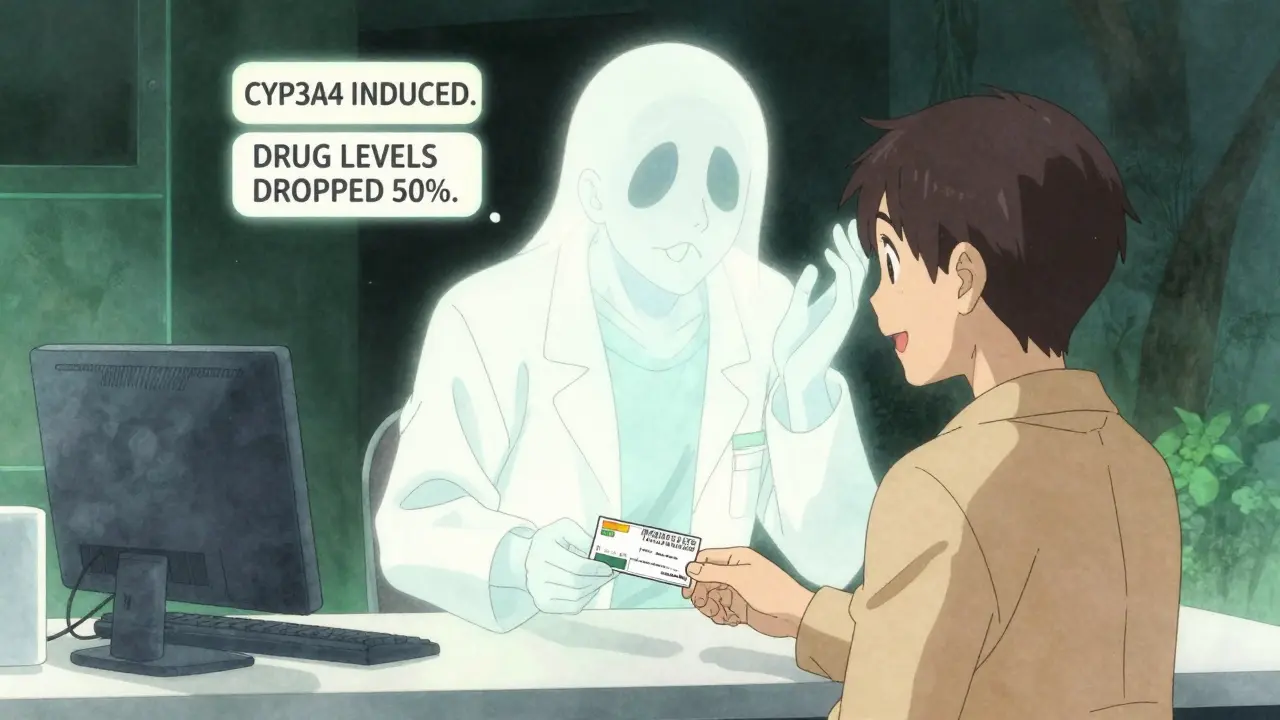
St. John’s Wort doesn’t just sit in your system. It actively changes how your liver and gut handle other drugs. The key player is a compound called hyperforin. This substance turns on enzymes - specifically CYP3A4 and CYP2C9 - that break down medications. Think of it like a turbocharger for your body’s drug-cleaning system. Suddenly, drugs that used to last 12 hours are cleared in 6. Your blood levels drop. And if you’re on something that needs to stay at a steady level - like blood thinners, birth control, or transplant drugs - that drop can be catastrophic.
Studies show St. John’s Wort can reduce the concentration of some medications by 30% to 50%. That’s not a small tweak. That’s the difference between a drug working and failing completely. And it doesn’t matter if you take it in the morning and your pill at night. The enzyme induction lasts for days. Even stopping St. John’s Wort doesn’t fix things right away - it can take up to two weeks for your body to reset.
Medications That Can Become Ineffective - or Dangerous
There are over 50 prescription drugs with documented, clinically significant interactions with St. John’s Wort. Here are the most critical ones:
- Warfarin and other blood thinners: INR levels can plunge from a safe therapeutic range (2.0-3.0) down to 1.2 or lower. That means clots. One documented case saw a patient’s INR drop from 2.8 to 1.5 in just 10 days - leading to a stroke.
- Immunosuppressants like cyclosporine and tacrolimus: Organ transplant patients have lost grafts because St. John’s Wort caused drug levels to fall 40%. One patient reported being “hours away from rejection.”
- HIV medications: Protease inhibitors like saquinavir and non-nucleoside reverse transcriptase inhibitors like efavirenz can lose up to 50% of their potency. That’s not just treatment failure - it’s drug resistance.
- Antidepressants (SSRIs, SNRIs, nefazodone): St. John’s Wort itself increases serotonin. Add it to fluoxetine, sertraline, or citalopram, and you risk serotonin syndrome - a potentially fatal condition with high fever, seizures, and heart rhythm problems. Six Australian cases were reported between 2000 and 2020.
- Birth control pills: Ethinyl estradiol levels drop by 25-35%. There are over a dozen documented cases of unintended pregnancy in women taking birth control perfectly - while also taking St. John’s Wort.
- Anticonvulsants like phenytoin and carbamazepine: Seizure control can collapse. Patients have had breakthrough seizures after starting the herb.
- Digoxin: Levels drop by 25%. That can trigger heart failure in people with atrial fibrillation or heart disease.
- Benzodiazepines like alprazolam (Xanax): Anxiety returns because the drug is cleared too fast. One study showed a 40% drop in plasma levels.
- Statins: Atorvastatin and simvastatin lose effectiveness. Pravastatin and fluvastatin are safer - but only because they’re not metabolized by the same liver enzymes.
Why People Don’t Realize the Risk
Most people don’t think of supplements as drugs. They see “natural” and assume “safe.” That’s the biggest trap. A 2022 Johns Hopkins study found that 41% of patients taking prescription medications didn’t tell their doctor they were using St. John’s Wort. Why? Because they didn’t think it counted.
Pharmacists report the same pattern. Patients say, “I just take this herbal thing for my mood,” as if it’s tea. But it’s not. It’s a potent enzyme inducer. And when you’re on a drug with a narrow therapeutic window - where the difference between working and failing is tiny - that’s a recipe for disaster.
Even worse, many online reviews paint St. John’s Wort as a miracle cure. WebMD has over 1,200 user reviews, with 68% rating it effective for depression. But those reviews rarely mention the hidden risks. No one says, “It worked great - until my INR crashed.”
What to Do If You’re Taking It - or Thinking About It
If you’re currently taking St. John’s Wort and any prescription medication, stop immediately - but only after talking to your doctor. Don’t quit cold turkey if you’re on antidepressants. Withdrawal can cause dizziness, nausea, or mood swings. Your doctor needs to guide the transition.
Here’s what you need to do:
- Stop taking St. John’s Wort if you’re on any of the high-risk drugs listed above.
- Wait at least two weeks before starting any new medication that interacts with it. The enzyme induction doesn’t vanish overnight.
- Ask your doctor for therapeutic drug monitoring. If you’re on warfarin, cyclosporine, or anticonvulsants, your levels need to be checked 3-5 days after stopping St. John’s Wort.
- Use the checklist. The University of Adelaide has a 57-item interaction checklist. Print it. Bring it to your next appointment.
- Change how you answer the question. Doctors often ask, “Are you taking any other medications?” That’s not enough. Ask yourself: “Do I take any herbs, vitamins, or supplements?” If the answer is yes - say it out loud.
Regulations Are Catching Up - But Not Fast Enough
Australia has required warning labels on all St. John’s Wort products since 2018. Germany and Sweden treat it as a prescription-only medicine. The U.S. FDA still classifies it as a dietary supplement under DSHEA, meaning no pre-market safety review. That’s why the FDA issued a Drug Safety Communication in January 2023 - demanding stronger labels that specifically mention warfarin, cyclosporine, and SSRIs.
But labels aren’t enough. The Institute for Safe Medication Practices added St. John’s Wort to its 2023 List of High-Alert Herbal Products. Hospitals are now being urged to build automatic alerts into their electronic systems. When a doctor prescribes cyclosporine, the system should pop up: “Do not use with St. John’s Wort.”
There’s some hope on the horizon. A June 2023 study found that extracts with less than 0.3% hyperforin had significantly reduced interaction potential - while still helping with mild depression. That could lead to safer formulations. But right now, every bottle on the shelf contains enough hyperforin to cause serious harm.
Bottom Line: Natural Doesn’t Mean Safe
St. John’s Wort isn’t evil. For some people with mild depression, it works. But it’s not a harmless herb. It’s a powerful biochemical agent with the ability to override carefully calibrated medical treatments. The risks aren’t theoretical. They’re documented in hospital records, case reports, and patient stories.
If you’re considering St. John’s Wort - even for something as “minor” as low mood - talk to your doctor first. If you’re already taking it, tell them. Don’t assume they know. Don’t assume it’s safe. And don’t let the word “natural” fool you. When it comes to prescription drugs, your body doesn’t care if something came from a plant or a lab. It only cares about the chemistry.
Can I take St. John’s Wort with antidepressants?
No. Combining St. John’s Wort with SSRIs, SNRIs, or other antidepressants can cause serotonin syndrome - a potentially life-threatening condition. Symptoms include high fever, rapid heart rate, confusion, muscle rigidity, and seizures. Six documented cases in Australia involved people taking St. John’s Wort with citalopram, fluoxetine, or nefazodone. Even if you feel fine, the risk is real and avoidable.
How long does St. John’s Wort stay in your system?
The herb itself clears in a few days, but its effects on liver enzymes last much longer. Hyperforin induces CYP3A4 and other enzymes, and this induction can persist for up to two weeks after you stop taking it. That’s why experts recommend waiting at least two weeks before starting medications like warfarin, cyclosporine, or birth control pills after discontinuing St. John’s Wort.
Is St. John’s Wort safe if I only take it occasionally?
No. Even short-term use can trigger enzyme induction. Studies show that just two weeks of standard dosing (900 mg daily) increases CYP3A4 activity by up to 40%. There’s no safe “on-and-off” pattern. If you’re on a medication that interacts with St. John’s Wort, any use - even once - can put you at risk.
Are all St. John’s Wort supplements the same?
No. The amount of hyperforin - the main interaction-causing compound - varies widely between brands. Some contain less than 0.3%, others over 1%. Most supplements don’t list hyperforin content on the label. Until standardized, low-hyperforin products become widely available and regulated, assume every product carries the same risk.
What should I tell my pharmacist?
Tell them you’re taking St. John’s Wort - even if you think it’s just a “natural mood booster.” Pharmacists can run interaction checks and flag dangerous combinations. Don’t say “I take an herb.” Say exactly what it is: “I take St. John’s Wort, 300 mg three times a day.” Precision saves lives.
Is there a safer alternative for depression?
Yes. For mild to moderate depression, evidence supports exercise, cognitive behavioral therapy (CBT), and certain FDA-approved antidepressants with lower interaction risks. St. John’s Wort was downgraded in the American Psychiatric Association’s 2023 guidelines precisely because of its interaction profile. Talk to your doctor about alternatives that won’t interfere with your other medications.
What to Do Next
If you’re on any prescription medication - especially blood thinners, birth control, HIV drugs, or immunosuppressants - review your supplement list today. Look for St. John’s Wort. If you find it, don’t panic. But do schedule a quick call with your doctor or pharmacist. Bring the bottle. Ask: “Could this interfere with my other meds?”
And if you’re thinking about trying it - don’t. There are safer, better-studied ways to manage mood. Your body doesn’t need another unregulated chemical in the mix. The risks are too high, the consequences too real.
 Buy Generic Premarin Online? Safe Options, Cheaper Estradiol Alternatives, and 2025 Prices
Buy Generic Premarin Online? Safe Options, Cheaper Estradiol Alternatives, and 2025 Prices
 Evaluation for on-line pharmacy store sureviagra.com
Evaluation for on-line pharmacy store sureviagra.com
 Strength Training for Fat Loss: How to Program for Real Results
Strength Training for Fat Loss: How to Program for Real Results
 Caverta vs Other ED Pills: Detailed Comparison of Sildenafil Alternatives
Caverta vs Other ED Pills: Detailed Comparison of Sildenafil Alternatives
 Ovulation Induction Therapy: Your Guide to Success, Drugs & How Hormones Work
Ovulation Induction Therapy: Your Guide to Success, Drugs & How Hormones Work
Sonal Guha
January 12, 2026 AT 13:27Lawrence Jung
January 12, 2026 AT 14:32Alice Elanora Shepherd
January 12, 2026 AT 23:59Konika Choudhury
January 14, 2026 AT 14:50Darryl Perry
January 15, 2026 AT 13:36Windie Wilson
January 15, 2026 AT 21:30Amanda Eichstaedt
January 17, 2026 AT 07:23jordan shiyangeni
January 17, 2026 AT 16:32Abner San Diego
January 18, 2026 AT 09:54Eileen Reilly
January 18, 2026 AT 11:15Monica Puglia
January 20, 2026 AT 00:29steve ker
January 20, 2026 AT 02:10Rebekah Cobbson
January 20, 2026 AT 09:45Audu ikhlas
January 21, 2026 AT 07:47TiM Vince
January 21, 2026 AT 22:16