When you walk down the street and suddenly your legs feel like they’re filled with lead, you stop, bend forward, and the pain disappears-just like that. If this sounds familiar, you’re not alone. Thousands of people over 50 experience this exact scenario every day, often thinking it’s just aging or poor circulation. But it could be something more specific: neurogenic claudication caused by spinal stenosis.
What Exactly Is Neurogenic Claudication?
Neurogenic claudication isn’t a disease on its own. It’s a symptom. A very telling one. It happens when the space around your spinal nerves in the lower back gets too narrow-usually because of wear and tear over time. This narrowing, called lumbar spinal stenosis, presses on the nerves that control sensation and movement in your legs. The result? Pain, numbness, tingling, or weakness that shows up when you’re upright and walking, and vanishes when you sit or lean forward. It’s not like regular muscle fatigue. This pain doesn’t go away with just resting. You have to change your posture. That’s the key. Most people describe it as a heaviness in the buttocks or thighs, sometimes radiating down to the calves. You might feel like your legs are going to give out. The relief isn’t random-it comes when you bend forward, like you’re leaning on a shopping cart, or when you sit down with your back curved. This is called the “shopping cart sign,” and it’s seen in 68% to 85% of confirmed cases.Why It’s Not Vascular Claudication
A lot of people get this confused with vascular claudication, which comes from poor blood flow to the legs. Both cause leg pain when walking. But here’s the difference: vascular claudication pain goes away with rest, no matter how you sit. Neurogenic claudication? It only goes away when you bend forward. That’s because it’s not about blood-it’s about nerves being pinched. Doctors check for this by testing your foot pulses. If they’re strong and equal on both sides, vascular disease is unlikely. If your reflexes are weak, or if you’ve lost some sensation in your feet, that points to nerve compression. One simple test they use is the five-repetitive sit-to-stand test. If you can do five stands in under 10 seconds, your leg strength is likely fine. If it takes longer, it’s a red flag.How Doctors Diagnose It
There’s no single blood test or scan that confirms neurogenic claudication. Diagnosis is built on clues. The first clue? Your story. Did your pain start slowly? Does it get worse the longer you walk? Do you have to stop and lean forward to feel better? If you answer yes to those, you’re already halfway there. Next comes the physical exam. Doctors look at how you walk. Do you have a bent-over posture? Do you avoid standing straight? They’ll check your spine’s range of motion-extending your back often makes the pain worse. They’ll test your reflexes, muscle strength, and sensation in your legs. A telltale sign? Wasting in the small muscles of the foot, especially the extensor digitorum brevis. That’s a subtle but reliable indicator of long-term nerve pressure. Imaging helps, but it’s not the whole picture. MRIs can show narrowing in the spine, but here’s the catch: up to 67% of people over 60 have spinal stenosis on MRI and feel zero pain. So seeing narrowing on a scan doesn’t mean you have the problem. It’s the combination of your symptoms and the exam that matters most. That’s why skipping the history and jumping straight to imaging leads to misdiagnosis. One patient on Healthgrades said it took three doctors before someone asked, “Do you feel better when you lean forward?”
Conservative Treatment: What Works
Most people don’t need surgery right away. In fact, 82% of those with early-stage neurogenic claudication get good relief with conservative care. The goal isn’t to cure the narrowing-it’s to manage the symptoms and keep you moving. First line: pain relief. Over-the-counter NSAIDs like ibuprofen help reduce inflammation around the nerves. For some, acetaminophen is enough. If pain is severe, doctors might prescribe short-term muscle relaxants or low-dose nerve pain medications like gabapentin. Second: physical therapy. Not just stretching. Specific exercises that encourage forward bending-like pelvic tilts, seated marches, and knee-to-chest stretches-help open up space around the nerves. Therapists also train you to use your posture strategically. Leaning forward while walking, using a walker or shopping cart, or even riding a recumbent bike can extend how far you can go without pain. Studies show patients who learn these techniques can increase their walking distance by 40% or more. Third: activity modification. Don’t stop walking. Just change how you do it. Take frequent breaks. Walk uphill instead of flat ground-uphill naturally puts your spine in a flexed position. Use a cane or walker for support. Many patients report being able to shop for hours if they push a cart instead of walking upright. This phase usually lasts 3 to 6 months. If you’re not improving, it’s time to consider the next step.When Injections and Surgery Come In
If conservative care doesn’t help after 3 to 6 months, epidural steroid injections are the next option. These deliver anti-inflammatory medicine directly around the compressed nerves. About 50% to 70% of patients get temporary relief-usually lasting a few weeks to several months. It’s not a cure, but it can buy time and reduce pain enough to get back into physical therapy. For those with persistent weakness, numbness, or pain that’s getting worse, surgery becomes a real option. The most common procedure is a laminectomy-removing part of the bone and ligament that’s pressing on the nerves. Minimally invasive versions are now common, with smaller incisions and faster recovery. One FDA-approved device, the Superion interspinous spacer, is implanted between the bones of the spine to keep the canal open. In trials, 78% of patients reported satisfaction after two years. Surgery isn’t for everyone. But for those who are good candidates, 70% to 80% report significant improvement within a year. The key is timing. Waiting too long can lead to permanent nerve damage. If you’re losing strength in your legs or having trouble controlling your bladder or bowels, that’s a medical emergency-you need surgery right away.What Patients Really Say
On patient forums, the stories are strikingly similar. One Reddit user wrote: “I could only walk 200 feet before my legs turned to cement. But if I pushed a grocery cart, I could do the whole store.” Another said, “I thought I had poor circulation. Turns out, I just needed to stop standing straight.” The common thread? Relief through posture. The frustration? Being misdiagnosed. Many patients see vascular specialists first, get tests for artery blockages, and are told nothing’s wrong. Then they find a spine specialist who asks the right question-and everything clicks. Those who understand their condition tend to manage it better. One study showed 78% of patients who learned to use the “shopping cart sign” as a tool could walk longer and felt more in control of their lives.
What’s Changing in Treatment
The field is moving toward more precise, less invasive options. In 2023, the American Academy of Orthopaedic Surgeons updated its guidelines to make structured exercise the #1 recommendation for all new cases. That’s a big shift-from pills and injections to movement as the foundation. New diagnostic tools are also in the works. The International Spine Study Group is finalizing a standardized algorithm to better match symptoms with imaging findings. Right now, too many people get unnecessary surgery because scans show stenosis, but symptoms don’t match. This new tool aims to fix that. Minimally invasive techniques are growing fast. Between 2018 and 2022, the number of these procedures jumped 35%. That’s because patients want faster recovery and fewer risks. For many, it’s no longer about “fixing” the spine-it’s about creating space so the nerves can work again.What to Do If You Think You Have It
If you’re over 50 and you get leg pain when walking that goes away when you sit or bend forward:- Start keeping a symptom journal. Note how far you walk before pain starts, what relieves it, and how long it lasts.
- Try leaning forward while walking. Use a walker, cane, or even a shopping cart. Does it help? Write it down.
- See a physical therapist trained in spinal conditions. Ask for flexion-based exercises.
- Don’t assume it’s just “getting old.” Ask your doctor: Could this be neurogenic claudication?
- Bring up the shopping cart sign. Most doctors haven’t heard the term-but they’ll recognize the behavior.
Final Thoughts
Neurogenic claudication isn’t rare. It’s becoming more common as the population ages. But it’s often missed. The good news? You don’t need surgery to live well with it. Most people find relief through posture, movement, and smart lifestyle changes. The key is recognizing the pattern-and not letting it be mistaken for something else. You don’t have to give up walking. You just have to change how you do it. And sometimes, all it takes is leaning forward.What does neurogenic claudication feel like?
Neurogenic claudication feels like heaviness, cramping, numbness, or weakness in the buttocks, thighs, or calves that happens when walking or standing. The pain usually doesn’t go away with rest alone-it improves when you sit down or bend forward at the waist. Many people describe it as their legs turning to lead after walking just a few blocks.
Is neurogenic claudication the same as vascular claudication?
No. Vascular claudication is caused by poor blood flow to the legs, often from artery blockage. Pain from vascular claudication goes away with rest, no matter your posture. Neurogenic claudication is caused by nerve compression in the spine, and pain only eases when you bend forward-like leaning on a shopping cart. Checking foot pulses and asking about posture changes helps doctors tell them apart.
Can you have spinal stenosis without symptoms?
Yes. Up to 67% of people over 60 show signs of spinal stenosis on MRI scans but have no pain or leg symptoms. That’s why diagnosis isn’t based on imaging alone. It’s about matching your symptoms-like leg pain that improves when bending forward-with physical exam findings. Having narrowing on a scan doesn’t mean you need treatment.
How long does physical therapy take to help with neurogenic claudication?
Most patients need 6 to 8 weeks of consistent physical therapy to see real improvement. Therapy focuses on flexion-based exercises, posture training, and learning how to use assistive devices like walkers or shopping carts. The goal isn’t to reverse stenosis-it’s to teach your body to move in ways that reduce pressure on the nerves.
When should you consider surgery for neurogenic claudication?
Surgery is considered when conservative treatments-like physical therapy, medication, and activity changes-haven’t helped after 3 to 6 months, and symptoms are getting worse. Signs you may need surgery include increasing leg weakness, loss of sensation, or trouble controlling bladder or bowel function. About 70% to 80% of carefully selected patients report good to excellent results after nerve decompression surgery.
Does the shopping cart sign always mean spinal stenosis?
The shopping cart sign is a very strong indicator of neurogenic claudication, seen in over two-thirds of confirmed cases. But it’s not 100% specific. Other conditions can cause people to lean forward for comfort. However, when combined with leg pain that worsens with walking and improves with forward bending, it’s one of the most reliable clinical clues doctors use to diagnose spinal stenosis.

 Discover Hericium Erinaceus: The All-Natural Miracle Supplement You Need to Try Today
Discover Hericium Erinaceus: The All-Natural Miracle Supplement You Need to Try Today
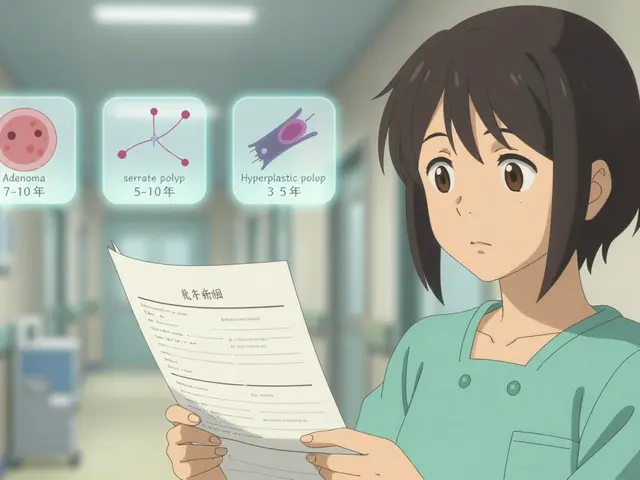 Repeat Colonoscopy: What Your Surveillance Interval Should Be After Polyp Removal
Repeat Colonoscopy: What Your Surveillance Interval Should Be After Polyp Removal
 How Clinician Communication Shapes Patient Trust in Generic Medications
How Clinician Communication Shapes Patient Trust in Generic Medications
 How to Safely Buy Cheap Generic Azithromycin Online
How to Safely Buy Cheap Generic Azithromycin Online
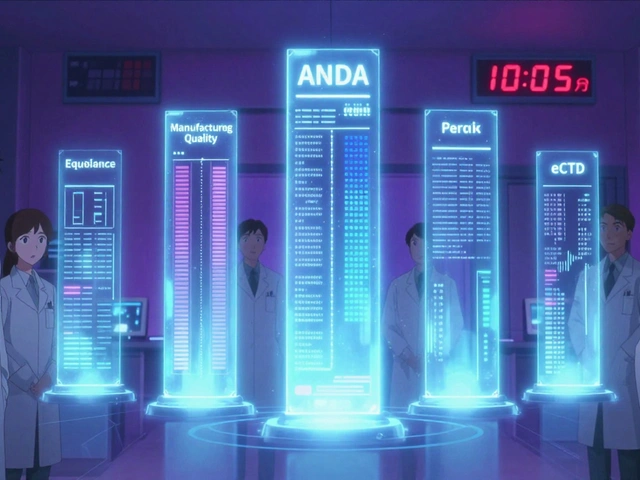 FDA Generic Drug Approval: Step-by-Step Process for ANDA Submission
FDA Generic Drug Approval: Step-by-Step Process for ANDA Submission
Nicholas Miter
January 25, 2026 AT 01:31Been there. Thought it was just getting old until I started pushing a cart at the grocery store and realized I could walk the whole aisle. Turns out my spine was the issue, not my legs. Took three doctors to get it right.
Now I walk with a cane and it’s life-changing.
Ashley Karanja
January 26, 2026 AT 17:46It’s fascinating how neurogenic claudication is such a classic example of somatic symptomatology being misattributed to vascular pathology-especially in aging populations where comorbidities muddy the clinical picture.
What’s underappreciated is the neuroplasticity potential in flexion-based rehab: the nervous system adapts to positional loading, and therapists who leverage proprioceptive feedback via controlled lumbar flexion can significantly modulate pain perception without pharmacological intervention.
It’s not just about decompression-it’s about retraining the sensorimotor loop. The shopping cart sign isn’t a quirk-it’s a biomarker of neural adaptation in real time.
Karen Droege
January 28, 2026 AT 15:49OH MY GOD. I spent YEARS going to cardiologists, getting stress tests, being told I had ‘poor circulation’-until one PT asked me if I leaned forward when I walked. I cried. I was so tired of being dismissed.
Now I walk with a walker and a smile. I can go to the mall again. My grandkids don’t have to carry me anymore. This isn’t just medicine-it’s dignity.
PLEASE, if you’re reading this and you’re over 50 and your legs feel like concrete after 10 minutes-STOP. BEND FORWARD. SEE A SPINE SPECIALIST. You’re not broken. You’re just compressed.
Napoleon Huere
January 28, 2026 AT 22:45It’s funny how society treats aging like a disease to be fixed, not a process to be understood. We’re told to ‘push through’ pain, to ‘stay active,’ but no one tells us how to move differently when our bodies change.
Neurogenic claudication isn’t a failure-it’s feedback. The body is saying, ‘Hey, your posture isn’t serving you anymore.’
Maybe the real question isn’t ‘How do we fix the spine?’ but ‘How do we redesign how we live in our bodies?’
Leaning forward isn’t weakness. It’s wisdom.
Shweta Deshpande
January 30, 2026 AT 10:28I’m so glad this was posted! My mom had this and we didn’t know what was going on for over a year. She thought she was just getting slower, but once she started doing those knee-to-chest stretches and used a shopping cart, she went from barely walking around the block to taking daily walks with her friends.
It’s not a miracle cure, but it’s a game-changer. Don’t give up-your body is still trying to talk to you. Just listen differently.
Ashley Porter
January 31, 2026 AT 20:23Interesting that the MRI stats are so high in asymptomatic populations. Reminds me of the whole ‘incidentalomas’ debate in radiology. Correlation ≠ causation, especially in degenerative spine imaging.
Still, the clinical correlation here is solid-posture-dependent symptomatology is a rare gem in neurology. Most conditions don’t come with such a clear behavioral trigger.
Kipper Pickens
February 2, 2026 AT 04:42As someone who’s worked in rehab across three continents, I’ve seen this exact pattern in the US, India, and the UK. The ‘shopping cart sign’ is universal. What varies is access to PT.
In rural India, patients use bamboo poles. In the UK, they use walking sticks. Here? They buy ergonomic carts. Same solution, different tools.
It’s not about tech-it’s about adaptation. The body doesn’t care about your insurance plan.
Aurelie L.
February 3, 2026 AT 14:04So you’re telling me I’ve been walking wrong my whole life?
Wow. Just… wow.
Joanna Domżalska
February 4, 2026 AT 12:53Of course it’s not vascular. Everything is always the spine. Always. They just want to sell you an MRI and then surgery. I’ve seen this script 10 times. The real issue? The healthcare system turns normal aging into a product.
Lean forward? That’s not treatment. That’s surrender.
bella nash
February 5, 2026 AT 22:03It is of paramount importance to underscore that the diagnostic paradigm for neurogenic claudication must be predicated upon a meticulous integration of patient-reported outcomes with objective physical examination findings, as opposed to the overreliance upon radiographic modalities, which, as elucidated in the aforementioned text, exhibit a marked prevalence of asymptomatic structural anomalies within the geriatric cohort.
Consequently, the clinical acumen of the practitioner remains the principal determinant of diagnostic fidelity.
Geoff Miskinis
February 7, 2026 AT 20:03Let’s be real: this is just the latest iteration of ‘movement is medicine’ propaganda dressed up as science. You’re telling people to lean on a shopping cart like it’s a miracle device? What’s next? Yoga for sciatica? Acupuncture for stenosis?
Meanwhile, real patients with real nerve damage are waiting months for decompression because everyone’s too busy ‘optimizing posture’ to admit when they need a scalpel.
Stop romanticizing suffering. Sometimes, you just need to cut it out.