When your lungs start to feel heavy, your chest aches, and you can’t catch your breath, it’s easy to assume it’s just a bad cold. But if symptoms don’t improve after a few days-or get worse-you could be dealing with pneumonia. This isn’t just a chest cold. It’s an infection that fills the tiny air sacs in your lungs with fluid or pus, making it hard to breathe. And not all pneumonia is the same. The cause changes everything: how you feel, how it’s diagnosed, and most importantly, how it’s treated.
Bacterial Pneumonia: The Sudden Onset
Bacterial pneumonia is the most common type, making up about half of all community-acquired cases. The main culprit? Streptococcus pneumoniae, or pneumococcus. This bacteria doesn’t just show up out of nowhere-it often follows a cold or flu, especially in kids under 5 and adults over 65. It’s also the leading cause of pneumonia hospitalizations in the U.S. You’ll know it when you feel it. Unlike a slow-burning virus, bacterial pneumonia hits fast. One day you’re fine; the next, you’re running a high fever-102°F to 105°F. Your cough turns thick and wet, coughing up yellow, green, or even bloody mucus. You might feel sharp pain when you breathe or cough, and your lips or fingernails could turn blue because your body isn’t getting enough oxygen. Doctors can often spot it on a chest X-ray: one lobe of the lung looks solid white, like a cloud filling up a space that should be full of air. That’s called lobar consolidation. Blood tests usually show high white blood cell counts, and sputum cultures can confirm the bacteria. Treatment? Antibiotics. Penicillin, amoxicillin, or macrolides like azithromycin are common first choices. For more resistant strains, fluoroquinolones like levofloxacin are used. The good news? Most people start feeling better within 48 to 72 hours of starting the right antibiotic. The bad news? If you don’t finish the full course, the bacteria can come back stronger-and harder to kill.Viral Pneumonia: The Slow Burn
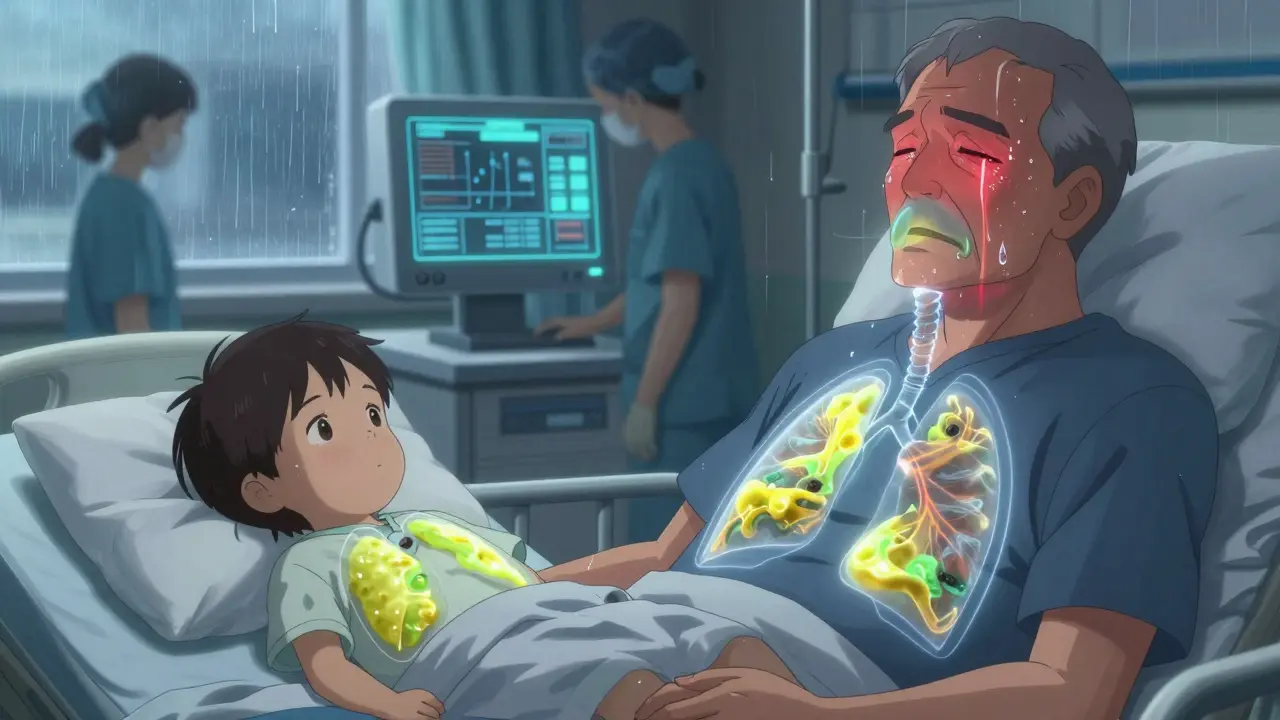
About one-third of pneumonia cases are viral. These are often caused by the same viruses that give you the flu: influenza A and B, respiratory syncytial virus (RSV), and SARS-CoV-2 (the virus behind COVID-19). Rhinovirus and human metapneumovirus are also common, especially in kids. This type doesn’t come on with a bang. It creeps in. You might start with a runny nose, sore throat, or mild cough. Over the next few days, your fever rises-but usually stays below 102°F. You feel achy, tired, and weak. Your cough becomes dry and persistent, not productive like bacterial pneumonia. Breathing feels harder, but not because your lungs are full of pus. It’s because the virus has inflamed the tiny airways and the tissue around them. On an X-ray, viral pneumonia looks different. Instead of one solid white patch, you’ll see a hazy, scattered pattern across both lungs. That’s called interstitial infiltrates. It means the inflammation is spread out, not stuck in one area. Antibiotics won’t help here. That’s a critical point. Taking them for a viral infection doesn’t cure you-it just adds to the growing problem of antibiotic resistance. In fact, the CDC says about 30% of outpatient antibiotic prescriptions are unnecessary, and viral pneumonia is one of the biggest reasons why. Treatment is mostly supportive: rest, fluids, fever reducers like acetaminophen, and oxygen if needed. For flu-related pneumonia, antivirals like oseltamivir (Tamiflu) can help if started within 48 hours of symptoms. For severe COVID-19 pneumonia, remdesivir or monoclonal antibodies might be used in hospitals. Here’s the scary part: viral pneumonia can open the door for bacterial pneumonia. About 25% to 30% of people with severe flu end up with a secondary bacterial infection-usually from Streptococcus pneumoniae or Staphylococcus aureus. That’s why doctors watch closely when someone with a viral infection starts getting worse after a few days.Fungal Pneumonia: The Hidden Threat
Fungal pneumonia is rare in healthy people. But if your immune system is weak-because of HIV, cancer treatment, an organ transplant, or long-term steroid use-it becomes a real danger. In the U.S., three fungi cause most cases: Coccidioides (Valley fever), Histoplasma capsulatum (histoplasmosis), and Blastomyces dermatitidis (blastomycosis). These aren’t caught from other people. You breathe them in from the soil. Farmers, construction workers, landscapers, and even people cleaning out bird coops are at higher risk. In places like the Ohio and Mississippi River valleys, nearly two-thirds of adults have been exposed to Histoplasma without even knowing it. Most never get sick. But if your body can’t fight back, the fungus can take root in your lungs. Symptoms mimic bacterial or viral pneumonia: fever, cough, chest pain, chills. But you might also have night sweats, weight loss, or even joint pain. Some people get rashes. The symptoms can last weeks or months, making it easy to mistake for tuberculosis or even cancer. Diagnosis is tricky. Standard tests won’t catch it. You need special cultures, blood tests for fungal antigens, or a biopsy. Chest X-rays often show nodules or cavities, not the solid white patches of bacterial pneumonia. Antibiotics? Useless. You need antifungals. Amphotericin B is used for severe cases. For milder ones, itraconazole or fluconazole are taken for months-even a year. Stopping too soon means the infection can come back.
How to Tell Them Apart
Knowing the difference isn’t just academic-it saves lives. Here’s how the three types compare:| Feature | Bacterial | Viral | Fungal |
|---|---|---|---|
| Onset | Sudden (hours to 1 day) | Gradual (3-7 days) | Slow (weeks) |
| Fever | High (102-105°F) | Mild to moderate (100-102°F) | Moderate to high (often persistent) |
| Cough | Productive (thick, colored mucus) | Dry, hacking | Productive, sometimes with blood |
| Chest X-ray | Lobar consolidation (one area) | Bilateral interstitial infiltrates | Nodules, cavities, or diffuse haze |
| Treatment | Antibiotics | Supportive care, antivirals if applicable | Antifungals (long-term) |
| Who’s at risk | All ages, especially young kids and seniors | Children, elderly, pregnant women | Immunocompromised, soil-exposed workers |
Prevention: What Actually Works
You can’t always avoid pneumonia, but you can lower your risk. For bacterial pneumonia, vaccines are your best tool. The pneumococcal vaccine (PCV20 or PPSV23) reduces infection risk by 60-70% in kids and 45-75% in adults. Yet, only 68% of adults over 65 have gotten it. That’s a huge gap. For viral pneumonia, the flu shot cuts pneumonia risk by 40-60% in good-match seasons. The updated COVID-19 vaccines reduce pneumonia risk by up to 90% in the first few months after vaccination. Fungal pneumonia? You can’t vaccinate against it. But you can reduce exposure. If you work with soil, dust, or bird droppings, wear a mask. Avoid digging or disturbing dirt in areas known for Valley fever-like Arizona or California’s Central Valley. Keep your immune system strong with good nutrition, sleep, and no smoking.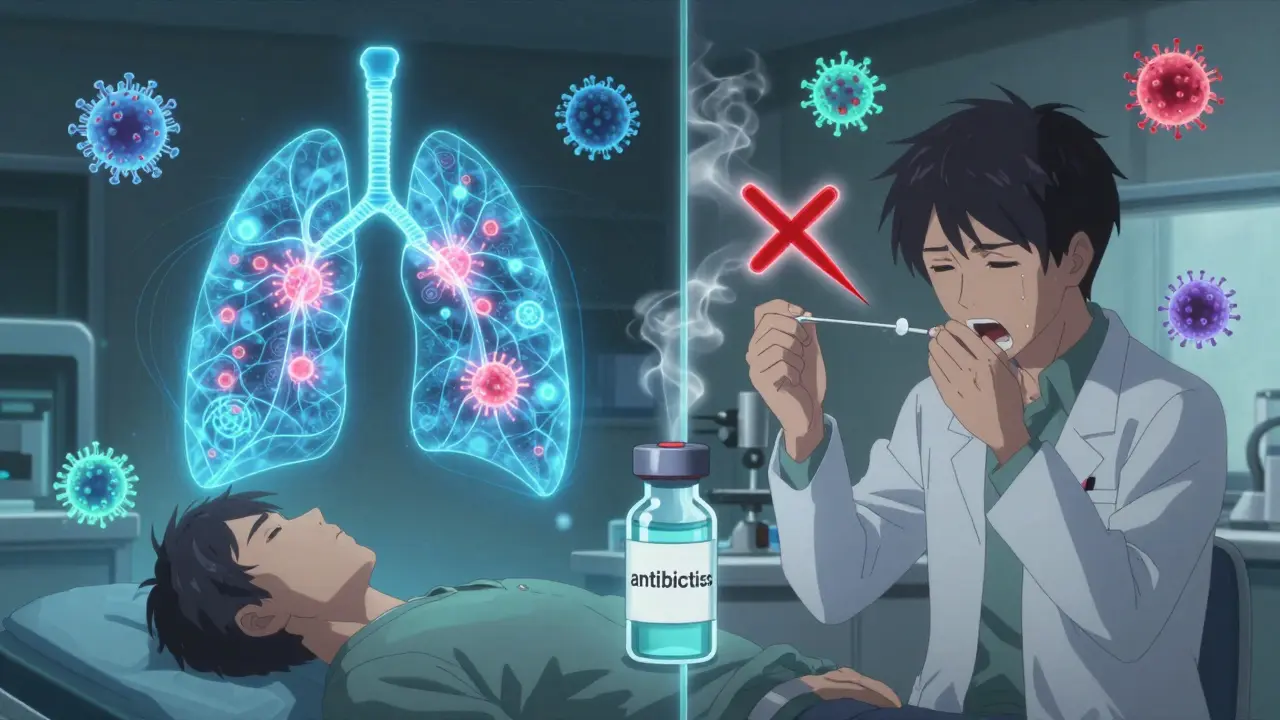
When to See a Doctor
Don’t wait until you’re gasping for air. Call your doctor if:- Your fever stays above 102°F for more than 48 hours
- You’re coughing up blood or thick green/yellow mucus
- Your breathing gets worse, even after resting
- Your lips or nails turn blue
- You feel confused or extremely weak
 Why Setting Boundaries Is Crucial for Living with Depressive Disorder
Why Setting Boundaries Is Crucial for Living with Depressive Disorder
 Top Natural Remedies for Asthma Relief: Magnesium, Caffeine, and Herbal Solutions Backed by Science
Top Natural Remedies for Asthma Relief: Magnesium, Caffeine, and Herbal Solutions Backed by Science
 FDA Generic Drug Approval: Step-by-Step Process for ANDA Submission
FDA Generic Drug Approval: Step-by-Step Process for ANDA Submission
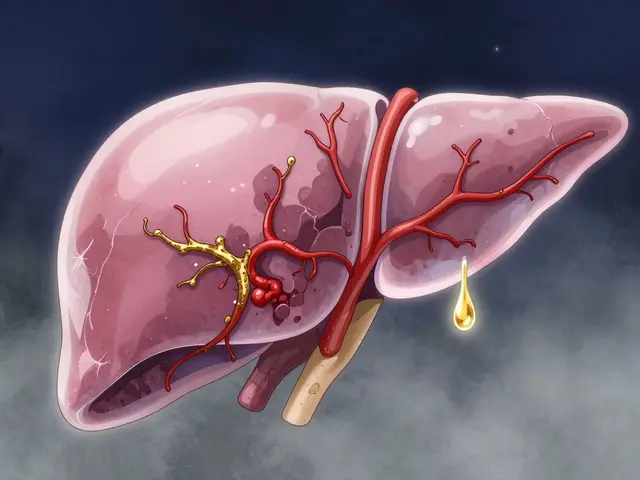 Cirrhosis: Understanding Liver Scarring, Failure Risk, and Transplant Options
Cirrhosis: Understanding Liver Scarring, Failure Risk, and Transplant Options
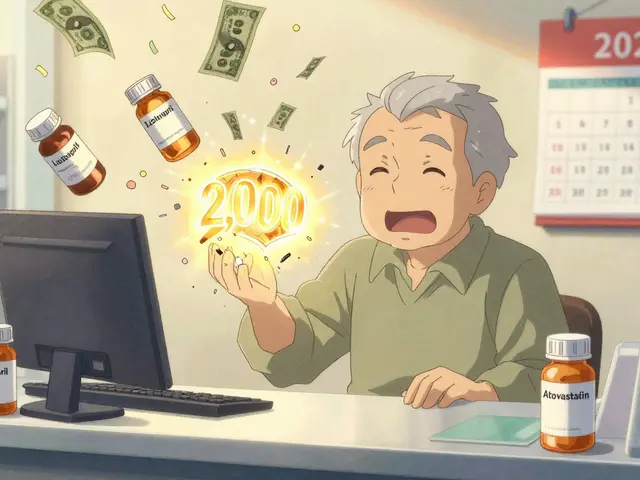 Medicare Drug Coverage and Cost Assistance Options in 2025-2026
Medicare Drug Coverage and Cost Assistance Options in 2025-2026
Jessica Bnouzalim
January 12, 2026 AT 08:56Ugh, I thought I had a cold last winter… turned out it was viral pneumonia. Took me 3 weeks to stop feeling like a ragdoll. No antibiotics helped. Just sleep, tea, and crying into my pillow. Don’t ignore a cough that lingers!!
Sumit Sharma
January 14, 2026 AT 07:45Incorrect assertion regarding fungal pneumonia diagnostics. Standard serological assays such as galactomannan ELISA and β-D-glucan testing are not merely ‘special’-they are gold-standard for immunocompromised hosts. Furthermore, histoplasmosis antigen detection in urine has >90% sensitivity in disseminated cases. Misinformation like this undermines public health literacy.
Jennifer Phelps
January 15, 2026 AT 17:23Wait so if you get the flu shot you’re basically protected from getting pneumonia from the flu? That’s wild I didn’t know that
beth cordell
January 16, 2026 AT 04:57My grandma had fungal pneumonia after her transplant… she was on antifungals for 14 months 😭. The docs said if she stopped even a week early it’d come back worse. So scary. 🕯️
Jay Powers
January 16, 2026 AT 13:02I work in a nursing home and we see bacterial pneumonia all the time in seniors. The biggest issue isn't the infection-it's the delay in getting them to the ER. They just say 'I'm tired' and keep going until they collapse. We need better community education
Sona Chandra
January 17, 2026 AT 18:40So you're telling me people in Arizona are just breathing in death spores and calling it a day? That's insane. Why isn't this on the news? Why aren't we spraying the desert with antifungals? This is a public health emergency and no one cares!
TiM Vince
January 19, 2026 AT 12:35My cousin got bacterial pneumonia after a flu shot. They said it was a coincidence. I still don’t believe it. Why do they keep pushing vaccines if they can trigger this?
George Bridges
January 21, 2026 AT 10:36Hey, I get why you're worried about the vaccine thing, but the stats show it actually lowers pneumonia risk by 40-60%. Most cases like your cousin's are just timing-catching a bug right after the shot, not because of it. It’s a tough thing to process though.
Bryan Wolfe
January 21, 2026 AT 17:10Just got my pneumococcal shot last week-finally did it after 10 years of ignoring it. I’m 62 and my doctor said if I don’t get it now, I might not get another chance. Also, if you’re around dirt or birds? Wear a mask. It’s not that hard. Seriously, your lungs will thank you.
Lauren Warner
January 22, 2026 AT 01:37Let’s be real-most people don’t care about pneumonia until they’re on a ventilator. The fact that 30% of antibiotic prescriptions are unnecessary is a direct result of lazy patients demanding pills and doctors too afraid to say no. This isn’t a medical issue-it’s a cultural one.
Craig Wright
January 23, 2026 AT 17:10It is regrettable that the American healthcare system continues to prioritize reactive interventions over preventive measures. In the United Kingdom, public health campaigns for pneumococcal vaccination in the elderly are mandatory and universally accessible. The disparity in outcomes is not merely statistical-it is moral.
steve ker
January 24, 2026 AT 02:42Why are we even talking about this? Just take antibiotics. Done.