Imagine this: You’re a pharmacist. A patient walks in with a new prescription for warfarin. You check their profile - no allergies, no history of kidney issues. But you don’t know they had a recent hospital stay where their creatinine levels spiked. You don’t know their cardiologist just changed their dose last week. You don’t know their insurance denied the last refill. So you dispense the script as written. Two days later, they end up in the ER with a dangerous bleed. That’s what happens when pharmacies and providers don’t talk.
That’s not a hypothetical. It’s the reality for most community pharmacies in the U.S. Even though 76% of prescriptions are sent electronically, only 15-20% of pharmacies can actually EHR integration with the provider’s system. That means most pharmacists are flying blind. They see the prescription, but not the full story behind it.
What EHR Integration Really Means for Pharmacies
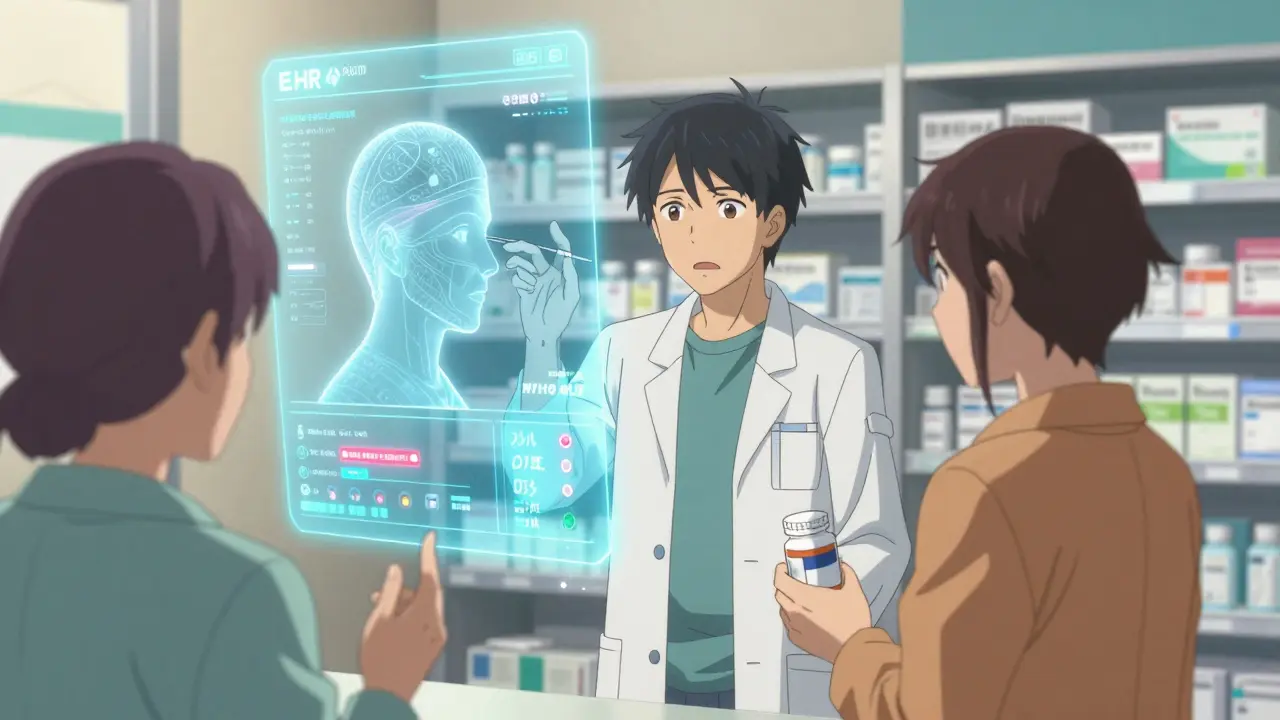
EHR integration isn’t just about sending a prescription from a doctor’s computer to the pharmacy. That’s e-prescribing - and it’s been around for years. True integration means two-way communication. The pharmacy system pulls in the patient’s full medical record: lab results, previous prescriptions, diagnoses, allergies, even notes from specialists. Then, the pharmacist can send back clinical insights - like a potential drug interaction, a missed refill, or a better alternative - directly into the provider’s EHR.
This isn’t science fiction. It’s built on two standards: NCPDP SCRIPT for sending prescriptions, and HL7 FHIR for sharing everything else. FHIR lets systems talk in plain language. Instead of a jumbled data dump, the pharmacy gets clean, structured information: "Patient has CHF, eGFR 32, on lisinopril, last lab drawn 3 days ago." That’s enough for a pharmacist to spot a problem before the patient leaves the store.
And it works. A 2021 study in East Tennessee showed pharmacists using integrated systems caught and resolved 4.2 medication problems per patient visit - more than double what they found without access. Providers accepted 92% of those suggestions. That’s not just efficiency. That’s saving lives.
Why Most Pharmacies Still Can’t Do It
So why aren’t all pharmacies doing this? Cost is the biggest wall. Independent pharmacies face $15,000 to $50,000 just to get started. That’s not just software - it’s staff training, API setup, compliance checks, and months of testing. Then there’s the $5,000-$15,000 annual fee to keep it running. For a small pharmacy making $200,000 a year in profit, that’s a huge gamble.
Then there’s the tech mess. There are over 120 different EHR systems in use across U.S. clinics. And more than 50 pharmacy management platforms. None of them talk the same language. Even when they try, data mapping fails. One system labels "hypertension" as "HTN." Another calls it "high BP." The integration tool doesn’t know they’re the same thing. That’s why 73% of health information exchanges say pharmacy data doesn’t fit cleanly into medical EHRs.
And time? Pharmacists are stretched thin. The average patient interaction lasts just 2.1 minutes. There’s no room to dig through a 50-page EHR summary. Even if they could, only 19 states pay pharmacists for reviewing that data. No reimbursement? No incentive. As one Wisconsin pharmacist told researchers: "We’re isolated. There’s nothing that connects us with information about a patient."
Who’s Doing It Right - And How
Some are breaking through. Surescripts, which handles over 22 billion transactions a year, offers a path: Medication History for Ambulatory, Eligibility checks, and Electronic Prior Authorization. Many chain pharmacies use it. CVS, Walgreens, and health system pharmacies have EHR integration built in - 89% of them, according to NCPA. They get real-time lab results, automatic refill alerts, and provider feedback loops.
Smaller players are catching up. SmartClinix and DocStation offer pharmacy-specific EMR platforms with FHIR APIs that connect to Epic, Cerner, and Meditech. One independent pharmacy in Ohio integrated with their local clinic’s Epic system and cut prior authorization time from 48 hours to 4. Another in Indiana reduced medication errors by 48% after adding automated alerts for drug-disease conflicts.
The real win? Time saved. Before integration, processing a prescription took 15.2 minutes on average. After? 5.6 minutes. That’s not just faster service - it’s more time to talk to patients. To ask, "Have you been taking this as prescribed?" To catch a dangerous combo before it’s too late.
The Hidden Benefits No One Talks About
Most people focus on safety. But the financial impact is just as powerful. Integrated systems cut medication-related hospital readmissions by 31%. That’s not just better care - it’s lower costs for hospitals, insurers, and patients. One study found $1,250 in annual savings per patient through better medication therapy management. That’s $1.2 million saved for a pharmacy serving 1,000 high-risk patients.
And then there’s the pharmacist’s role. Without integration, you’re a dispenser. With it, you become a consultant. You’re not just filling scripts - you’re managing therapy. You’re adjusting doses based on kidney function. You’re switching meds because of cost. You’re calling the doctor because the patient hasn’t refilled in 90 days. That’s clinical work. And it’s worth paying for.
Australia’s My Health Record system showed a 27% drop in preventable hospitalizations after full integration. The U.S. has the same tools - we just haven’t connected them yet.
What’s Changing in 2025 and Beyond
The tide is turning. CMS now requires Medicare Part D plans to have integrated pharmacy-provider communication by 2025 to qualify for top Star Ratings. California’s SB 1115 mandates EHR integration for medication therapy management by 2026. The ONC’s 2024 roadmap targets 50% of community pharmacies with bidirectional EHR access by 2027.
And new tech is coming. AI pilot programs at CVS and Walgreens are using machine learning to scan integrated data and flag high-risk patients before they have an adverse event. One program improved intervention accuracy by 37%. That’s not just automation - it’s prediction.
Even the law is catching up. The 2023 Pharmacy and Medically Underserved Areas Enhancement Act proposes Medicare reimbursement for pharmacist services delivered through integrated systems. If it passes, it could finally solve the biggest barrier: payment.
What You Can Do Today
If you’re a pharmacist or pharmacy owner, here’s what matters now:
- Check if your pharmacy software supports FHIR and NCPDP SCRIPT 2017071. If not, ask your vendor when it’s coming.
- Reach out to local clinics. Ask if they’re willing to share EHR access with your pharmacy. Start small - one provider, one patient type.
- Track your outcomes. How many drug interactions did you catch last month? How many refills were missed? Use that data to show ROI.
- Push for reimbursement. Talk to your state pharmacy association. Are there any pilot programs paying for MTM services?
If you’re a provider, don’t wait for the pharmacy to ask. Offer access. Your patients are seeing pharmacists more often than you. Give them the tools to help.
Integration isn’t about technology. It’s about trust. It’s about seeing the pharmacist not as a clerk, but as a partner. And it’s about making sure no one slips through the cracks because the systems don’t talk.
Frequently Asked Questions
What is the difference between e-prescribing and EHR integration?
E-prescribing is one-way: the doctor sends a prescription to the pharmacy. EHR integration is two-way: the pharmacy pulls in the patient’s full medical history - labs, diagnoses, allergies - and sends back clinical insights like medication adjustments or warnings. E-prescribing gets the script to the pharmacy. EHR integration helps the pharmacist keep the patient safe.
Why don’t all pharmacies have EHR integration?
Cost is the biggest barrier. Independent pharmacies face $15,000-$50,000 to implement, plus $5,000-$15,000 per year to maintain. Technical complexity is another issue - with over 120 EHR systems and 50 pharmacy platforms, data doesn’t always match up. And without reimbursement for pharmacist time spent reviewing records, there’s little financial incentive to invest.
Can small pharmacies afford EHR integration?
Yes, but it’s hard. Some vendors like SmartClinix and DocStation offer lower-cost EMR platforms with built-in integration tools, starting at under $250/month. Group purchasing through pharmacy associations can reduce costs. Some state programs offer grants for small pharmacies to adopt interoperability. The key is starting small - integrate with one clinic first, track results, then scale.
What standards do EHR-pharmacy systems use to communicate?
The NCPDP SCRIPT standard (version 2017071) handles prescription transmission. For broader clinical data - like lab results, allergies, and care plans - systems use HL7 FHIR Release 4 (R4). FHIR allows systems to exchange structured, readable data instead of messy files. The Pharmacist eCare Plan (PeCP) is a FHIR-based format specifically designed for pharmacists to share care summaries with providers.
Is EHR integration required by law?
Not yet for all pharmacies, but pressure is building. The 21st Century Cures Act bans information blocking, meaning providers can’t withhold data from pharmacists who request it. CMS requires Medicare Part D plans to have integrated pharmacy communication by 2025 to maintain high Star Ratings. California mandates it for MTM services by 2026. And the ONC aims for 50% of community pharmacies to be integrated by 2027.
How long does EHR integration take to implement?
Typically 3-6 months. It starts with a readiness assessment ($2,500-$5,000), then 8-12 weeks of technical setup, followed by 4-8 weeks of staff training. The biggest delays come from provider credentialing (averaging 28 days) and data mapping issues between systems. Pharmacies that partner with Surescripts or large EHR vendors often move faster due to pre-built connections.
What are the biggest benefits of EHR integration for patients?
Fewer dangerous drug interactions, fewer hospital readmissions, and fewer missed doses. Patients with chronic conditions like diabetes or heart failure see the biggest gains - studies show a 23% improvement in medication adherence and a 31% drop in avoidable hospital visits. Pharmacists with EHR access can catch problems early, adjust doses based on lab results, and ensure patients get the right meds at the right time.
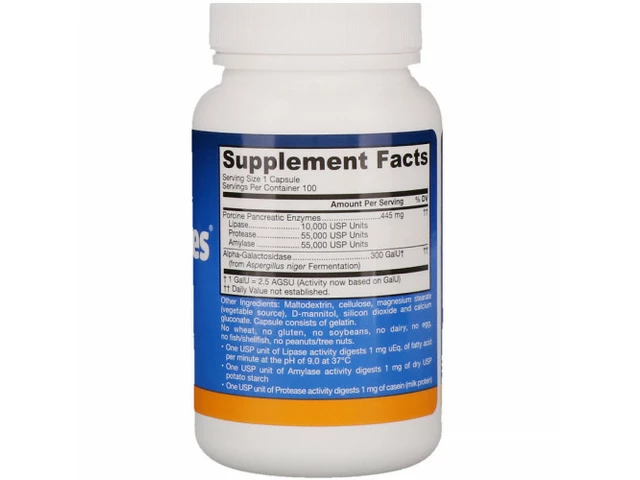 Unlock the Power of Lipase: The Ultimate Dietary Supplement for Improved Digestion
Unlock the Power of Lipase: The Ultimate Dietary Supplement for Improved Digestion
 Ginseng and Diabetes Medications: What You Need to Know About Blood Sugar Risks and Monitoring
Ginseng and Diabetes Medications: What You Need to Know About Blood Sugar Risks and Monitoring
 The Link Between Bimatoprost and Dry Eye Syndrome
The Link Between Bimatoprost and Dry Eye Syndrome
 How Sun Exposure Triggers Fungal Skin Discoloration (Tinea Versicolor)
How Sun Exposure Triggers Fungal Skin Discoloration (Tinea Versicolor)
 Hypernil (Lisinopril) vs Alternative Blood Pressure Drugs: A Practical Comparison
Hypernil (Lisinopril) vs Alternative Blood Pressure Drugs: A Practical Comparison
Virginia Seitz
December 16, 2025 AT 09:58Peter Ronai
December 17, 2025 AT 18:26Brooks Beveridge
December 18, 2025 AT 13:16Joe Bartlett
December 19, 2025 AT 20:58Naomi Lopez
December 21, 2025 AT 10:29Kent Peterson
December 23, 2025 AT 08:13Sachin Bhorde
December 25, 2025 AT 06:06Chris Van Horn
December 26, 2025 AT 13:08Michael Whitaker
December 27, 2025 AT 03:47Steven Lavoie
December 27, 2025 AT 19:39Anu radha
December 29, 2025 AT 16:22Jigar shah
December 30, 2025 AT 10:12Salome Perez
January 1, 2026 AT 06:40Marie Mee
January 1, 2026 AT 11:26amanda s
January 2, 2026 AT 03:08