FDA Biosimilars: What They Are, How They Work, and Why They Matter
When you hear FDA biosimilars, highly similar versions of complex biologic drugs approved by the U.S. Food and Drug Administration after proving they work the same way in the body. Also known as biologic generics, these drugs aren’t exact copies like traditional generics—they’re made from living cells, not chemicals, and require far more testing to prove they match the original in safety and effectiveness. Unlike regular generics, which copy simple chemical drugs, biosimilars tackle proteins made by living organisms—like insulin, cancer treatments, or autoimmune meds. That’s why they’re harder to make, harder to test, and still cost less than the brand-name version.
The FDA approval, the strict process the U.S. Food and Drug Administration uses to ensure drugs are safe and effective before reaching patients. Also known as regulatory review, it for biosimilars isn’t just a formality. It demands detailed studies showing the biosimilar behaves the same way in the body as the original—same absorption, same side effects, same results in clinical trials. The FDA doesn’t just check the label; they inspect the factory, analyze the molecule, and even compare how it interacts with immune cells. This is why a biosimilar isn’t just a cheaper version—it’s a scientifically verified alternative.
Many people confuse biosimilars with generic drugs, chemically identical copies of simple, small-molecule medications approved under the ANDA process. Also known as conventional generics, they. But here’s the key difference: generics copy aspirin or metformin—molecules you can replicate in a lab. Biosimilars copy Humira or Enbrel—complex proteins that can’t be perfectly copied, only closely matched. That’s why biosimilars are called "similar," not "identical." And that’s why the FDA requires more data. Still, once approved, they deliver the same clinical results, often at half the price.
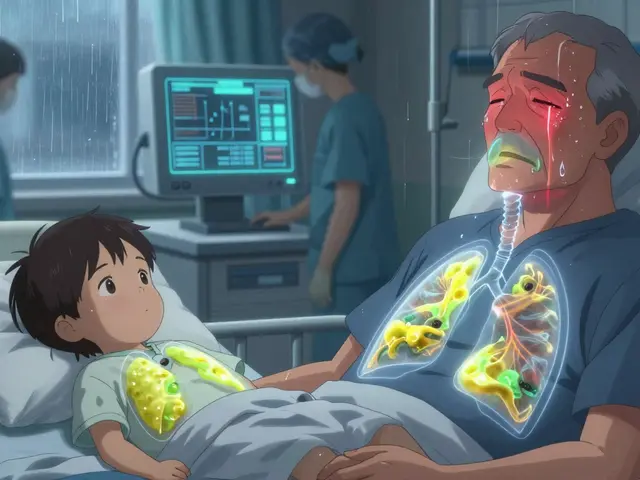
What does this mean for you? If you’re on a biologic drug for rheumatoid arthritis, Crohn’s, or cancer, a biosimilar could cut your out-of-pocket costs dramatically. Insurance companies are pushing them because they save billions. But you might notice a difference in the pill’s shape, color, or name—same active ingredient, different packaging. That’s normal. The FDA allows it, and your doctor or pharmacist will tell you if it’s safe to switch. Some patients worry biosimilars aren’t as good. But studies show no meaningful difference in effectiveness or safety. In fact, over 30 biosimilars are already approved in the U.S., used by millions.
Behind every biosimilar is a long road of science, testing, and regulation. It’s not magic—it’s medicine, refined. And it’s changing how we pay for life-saving drugs. The next time you hear "biosimilar," don’t think "cheap copy." Think "proven alternative." And if you’re switching from a brand-name biologic, know this: the FDA didn’t approve it unless it worked just as well.
Below, you’ll find real stories and facts about how biosimilars fit into everyday care—from insurance battles to patient trust, from manufacturing to side effect monitoring. These aren’t theory pieces. They’re what people actually deal with when they choose a biosimilar.