Donor Registry: Your Guide to Donating and Tracking
When you hear the term donor registry, a centralized system that records people willing to give organs or blood for medical use. Also known as donor database, it helps match donors with patients in need and ensures compliance with eligibility rules. If you're curious about how a donor registry works, keep reading.
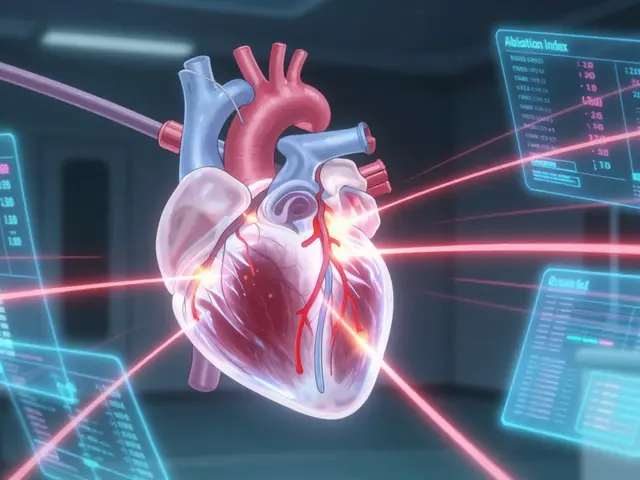
One of the biggest pieces of a donor registry is organ donation, the process of giving a healthy organ to someone who needs a transplant. The registry stores medical history, tissue type, and consent status, then feeds that data into the transplant waiting list, a prioritized queue of patients awaiting an organ match. This connection means a single entry in the registry can potentially save multiple lives over time.
Blood donation follows a similar logic. blood donation, the act of giving a portion of your blood for transfusions, emergencies, or research relies on rapid matching of blood type, antigen profile, and donation frequency. The registry flags eligible donors, alerts nearby collection centers, and tracks when you’re due for your next donation. Because blood has a short shelf‑life, the registry’s real‑time alerts are crucial for keeping hospitals stocked.
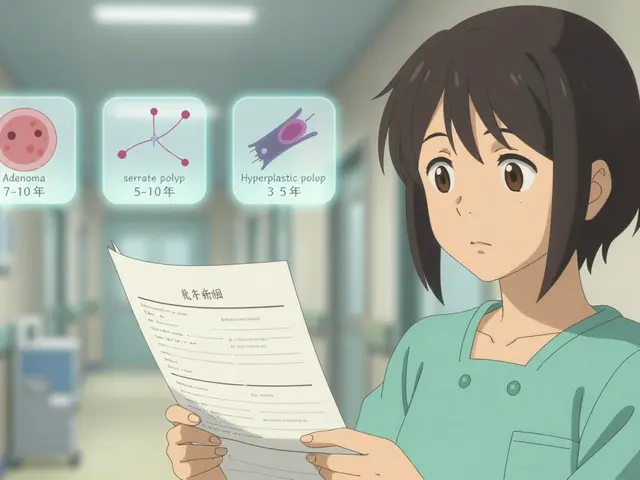
Eligibility is where medical details matter most. A donor must meet criteria around age, weight, recent illnesses, and the medications they’re taking. For example, certain antihypertensives like lisinopril, or antibiotics such as amoxicillin, are generally safe, while blood thinners or hormonal therapies might pause eligibility. The registry records these meds, so a patient with skin inflammation or psoriasis will see a clear note about any needed waiting period. This level of detail prevents complications during surgery or transfusion.
Hospitals and transplant centers access the registry through secure portals. They pull anonymized data to plan surgeries, allocate organs, and even run research on donation trends. Privacy safeguards mean your personal health info stays protected, while the aggregated data drives better matching algorithms. In practice, when a heart becomes available, the system instantly checks for compatible blood type, tissue match, and donor consent, then notifies the surgical team.
Getting onto the registry is straightforward. Most countries offer an online form where you enter basic demographics, consent choices, and a brief health questionnaire. After verification, you receive a donor card or a digital ID. Some platforms let you update your medical history in real time—so if you start a new prescription, you can log it immediately, keeping the registry current.
There are common myths that deter people. A frequent worry is that organ donation will limit the care you receive if you ever need a transplant yourself. In reality, donor status does not affect your own eligibility; the registry simply adds you to a pool of potential lifesavers. Another myth is that only “healthy” people can donate. While certain conditions—like uncontrolled diabetes or active infections—disqualify you temporarily, many chronic diseases are manageable and do not block donation after proper assessment.
Below you’ll find a curated set of articles that dive deeper into specific medical topics, drug safety, and step‑by‑step guides for buying affordable generic medicines online. These pieces complement the donor registry overview by explaining how various health conditions and medications intersect with donation eligibility, what you need to know before you sign up, and how to stay informed about the latest safety standards.