Confidence Interval: What It Means and How It Affects Your Medication Decisions
When you hear that a new drug reduces blood pressure by 10 mmHg, you might think that’s the exact number. But what if that number could be 5 mmHg—or 15 mmHg? That’s where a confidence interval, a range of values that shows how certain we are about a measured effect. It’s not just math—it’s your safety net when deciding if a drug really works. A 95% confidence interval means if you ran the same study 100 times, 95 of those times the true effect would fall inside that range. It doesn’t guarantee the result, but it tells you how much room for error there is. In medicine, that margin matters. A drug with a confidence interval of 8–12 mmHg drop in blood pressure is far more reliable than one with 1–19 mmHg. The wider the interval, the less sure you are.
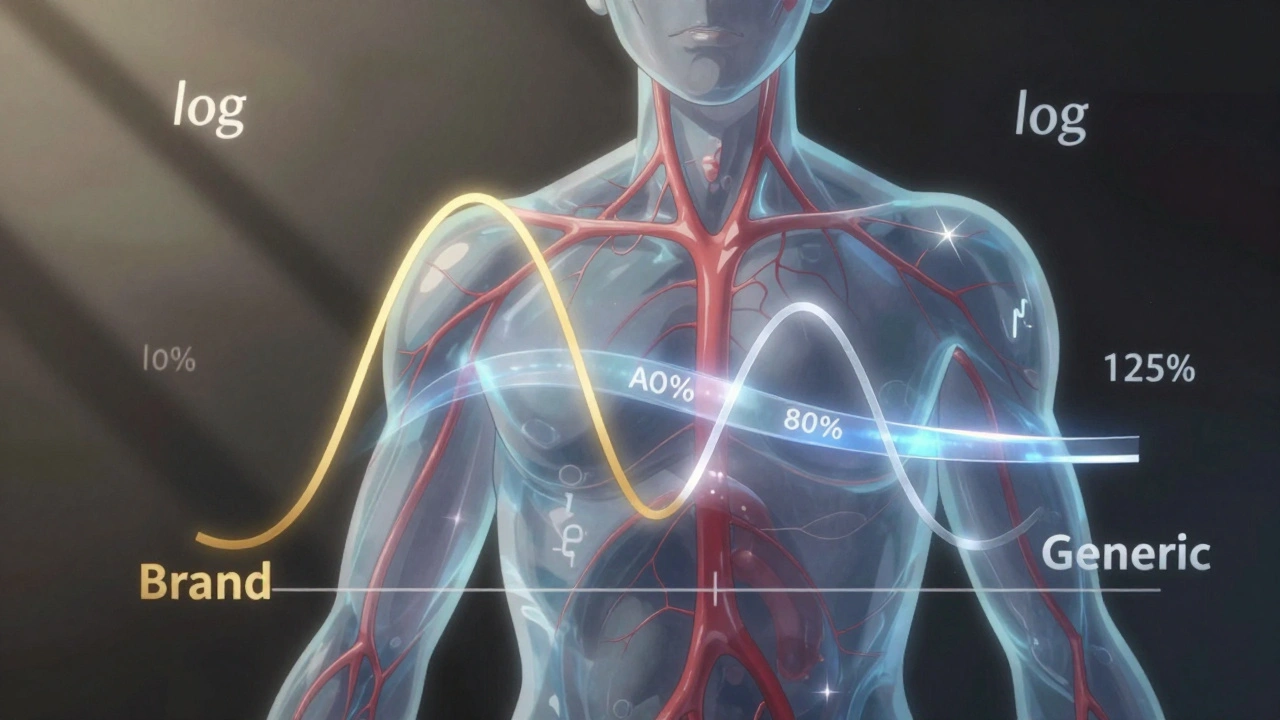
Every time you read about a new medication, clinical trial, or generic drug equivalence, you’re seeing confidence intervals hiding behind the numbers. The FDA doesn’t approve drugs based on a single number—they look at the full range. For example, when comparing a generic to a brand-name drug, the confidence interval for bioequivalence must stay within 80–125% of the original. If it doesn’t, the generic gets rejected. That’s why some generics pass and others don’t, even if they look identical. Same active ingredient, different confidence intervals. And it’s not just about effectiveness. When a study says a side effect occurs in 2% of users, the confidence interval might show it’s really between 0.5% and 4%. That’s the difference between a rare risk and a real concern.
Confidence intervals also explain why some studies contradict each other. Two trials might both say a drug helps with anxiety, but one shows a 30% improvement (25–35%) and another shows 15% (5–25%). The first is solid. The second? Too wide to trust. That’s why you’ll see headlines like "New Study Finds No Benefit"—but the real story is often buried in the interval. It’s not that the drug doesn’t work. It’s that the evidence isn’t clear enough yet. And when you’re choosing between medications, especially for chronic conditions like diabetes or hypertension, that uncertainty can change your outcome. You don’t need to calculate these numbers yourself—but knowing they exist, and why they matter, helps you ask better questions. When your doctor says "this drug works," ask: "How sure are you?" That’s the real power of a confidence interval.
Below, you’ll find real-world examples of how this concept shows up in medication safety, generic drug approvals, clinical trial results, and even how pharmacists explain risks to patients. No theory. No fluff. Just what you need to know to understand what the numbers really mean.