Anticoagulant Supplements: What They Are, How They Work, and What to Watch For
When you hear anticoagulant supplements, natural products used to reduce blood clotting. Also known as blood thinners, they include things like ginseng, garlic, fish oil, and vitamin E — all commonly taken for heart health or inflammation. But unlike prescription drugs, these aren’t regulated for strength or purity, and they can sneak up on you when mixed with real blood thinners like warfarin or apixaban.
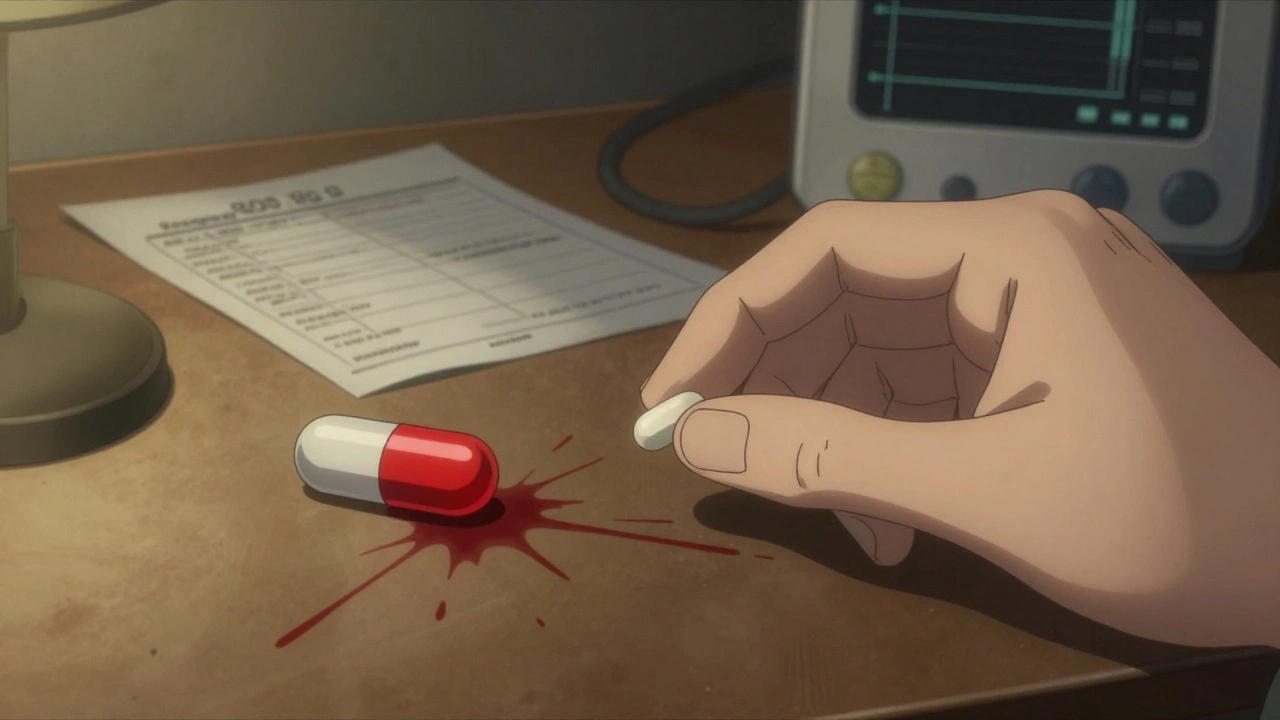
Many people think if it’s natural, it’s safe. That’s not true. A study in the Journal of the American Heart Association found that over 40% of patients on warfarin who took fish oil or ginseng had dangerous spikes in their INR levels — meaning their blood took too long to clot. That’s not a minor risk. It’s bleeding in the brain, in the gut, or after a fall. Even something as simple as a daily turmeric capsule can interfere with how your liver processes medications. And if you’re taking more than one supplement? The risks multiply. These aren’t just side effects — they’re hidden collisions inside your body.
It’s not just about what you take — it’s about what you don’t know. Your doctor might ask if you’re on blood thinners, but they rarely ask if you’re popping herbal pills. And pharmacies don’t always flag interactions between supplements and prescriptions. That’s why you need to track everything: name, dose, frequency. A single bottle of ginseng can contain wildly different amounts of active compounds depending on the brand. One study found some products had zero ginsenosides — the actual active ingredient — while others had five times the labeled amount. You can’t trust labels. You can only trust awareness.
Some supplements are outright dangerous when combined with anticoagulants. Garlic, for example, can double bleeding time. Ginger? Same issue. Even green tea extract, often taken for weight loss, can interfere with clotting factors. On the flip side, vitamin K-rich foods like kale or spinach can make blood thinners less effective — which is why people on warfarin are told to keep their intake steady. It’s not about avoiding greens. It’s about consistency. The same goes for supplements. If you start taking one, stick with it. If you stop, tell your doctor. No gray areas.
There’s a reason the FDA keeps a list of drugs you can flush down the toilet — because some medicines are too risky to leave around. The same logic applies to supplements. If you’re on a prescription anticoagulant, any new supplement is a potential emergency waiting to happen. You don’t need to avoid all natural products. You need to know which ones are playing with fire. And you need to talk to someone who understands how these things interact — not just a supplement store clerk.
Below, you’ll find real, practical posts that break down exactly what happens when herbal supplements meet blood thinners, how to spot dangerous interactions before it’s too late, and what to ask your pharmacist when you pick up your next prescription. No fluff. No marketing. Just what you need to stay safe.