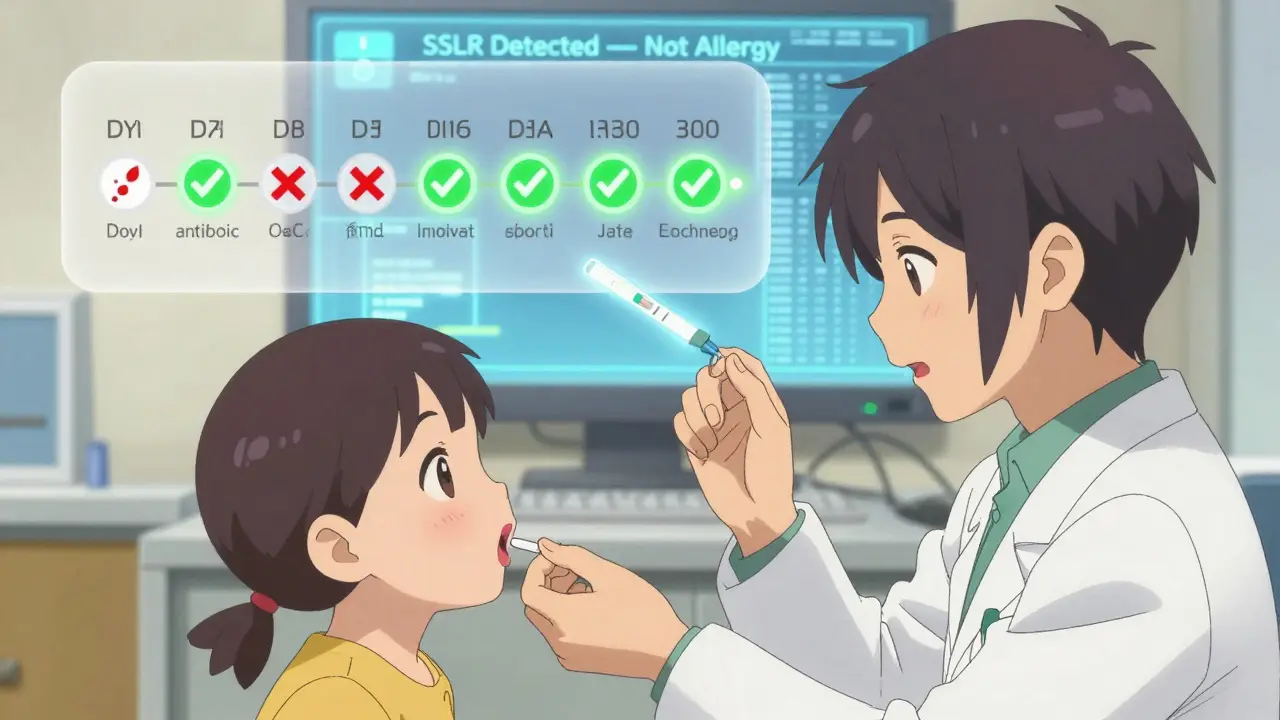
SSLR Diagnosis Checker
Is This a Serum Sickness-Like Reaction?
Use this tool to help determine if your child's reaction to antibiotics is likely SSLR (serum sickness-like reaction) or a true allergy.
When a child develops a rash, fever, and swollen joints a week after taking an antibiotic, it’s natural to panic. Was it an allergy? Is this life-threatening? Could they never take penicillin again? For many families, the answer isn’t as simple as it seems. What they’re experiencing might not be a true allergy at all - it could be a serum sickness-like reaction (SSLR), a delayed immune response tied to certain antibiotics, especially in young kids.
What Exactly Is a Serum Sickness-Like Reaction?
Serum sickness-like reaction isn’t serum sickness. That’s the key. True serum sickness, first described in 1906, happens after receiving animal-derived antiserum - like anti-rabies shots or snake antivenom. It’s caused by immune complexes floating in the blood, triggering inflammation, kidney damage, and sometimes severe joint pain. But SSLR? It’s different. It doesn’t involve those immune complexes. It doesn’t hurt the kidneys. It’s milder, more common in kids, and almost always linked to antibiotics - especially cefaclor.SSLR shows up 1 to 21 days after taking the drug, with most cases appearing around day 7 to 10. It’s not an immediate reaction like anaphylaxis. You won’t get swelling of the throat or trouble breathing right after the pill. Instead, symptoms creep in slowly. The classic trio? A bumpy, itchy rash that moves around the body, a low-grade fever (usually 38-39°C), and joint pain - often in the knees, wrists, or ankles. Kids might complain their legs ache, or refuse to walk. Lymph nodes might swell. They feel tired. But their lungs, liver, and kidneys? Usually fine.
And here’s the big deal: if you mistake this for a penicillin allergy, you could be locking your child into a lifetime of restricted antibiotics. That means more expensive, broader-spectrum drugs like vancomycin or azithromycin - drugs that disrupt gut bacteria, increase resistance, and carry their own risks. In fact, studies show that when SSLR is mislabeled as a true allergy, kids are 42% more likely to get unnecessary broad-spectrum antibiotics later on.
Which Antibiotics Cause It?
Not all antibiotics trigger SSLR. The big one is cefaclor, a second-generation cephalosporin. It’s responsible for 65% to 80% of pediatric cases. Why? Researchers think it has to do with how some kids metabolize it. A genetic variant in the CYP2C9 enzyme - found in about 72% of affected children - leads to buildup of a specific metabolite that the immune system reacts to. It’s not the antibiotic itself, but what the body turns it into.Other culprits include amoxicillin (especially in younger kids), and occasionally minocycline or other beta-lactams. But here’s the good news: if your child had SSLR from cefaclor, they’re very likely to tolerate other cephalosporins like cephalexin or cefdinir. Studies show 89% of kids with SSLR can safely take different antibiotics in the same class. That’s why avoiding all penicillins or cephalosporins after SSLR is outdated and unnecessary.
And no - this isn’t a sign you’re allergic to all antibiotics. SSLR is a distinct reaction pattern, not a generalized hypersensitivity. It’s like being sensitive to one type of citrus fruit but still being able to eat oranges and limes without issue.
How Is It Different From True Serum Sickness or Other Rashes?
It’s easy to confuse SSLR with other conditions. Viral rashes (like from strep throat or EBV) look similar. Acute urticaria (hives) can mimic the rash. Even rheumatic fever - which also causes joint pain - gets mixed up with it. But here’s how to tell them apart:| Feature | SSLR | True Serum Sickness | Common Viral Rash |
|---|---|---|---|
| Typical Age Group | 6 months to 6 years (78% of cases) | Adults (65% over age 18) | All ages |
| Trigger | Cefaclor, amoxicillin | Antivenom, infliximab, rituximab | Viruses like strep, EBV, parvovirus |
| Onset After Exposure | 1-21 days (median 7 days) | 7-21 days | 1-5 days |
| Rash Type | Migratory urticaria (comes and goes) | Fixed or maculopapular | Fixed, non-itchy, widespread |
| Fever | 85% of cases | 98% of cases | Common |
| Joint Pain | 72% of cases | 80% of cases | Uncommon |
| Kidney Involvement | None | 15-25% (proteinuria) | None |
| Immune Complexes in Blood | Absent | Present | Absent |
| Resolution Time | 3-7 days after stopping drug | 2-4 weeks | 3-10 days |
Lab tests help too. In SSLR, complement levels (C3, C4) stay normal. Urine is clean - no protein. No cryoglobulins. No vasculitis on biopsy. In true serum sickness, all those markers go haywire. If a doctor orders a blood test and finds normal results but the child still has the classic triad, SSLR is the most likely answer.
What Happens After the Reaction?
The good news? Most kids bounce back fast. Once the antibiotic is stopped - and it should be stopped within 24 hours of symptoms starting - the rash fades, the fever drops, and the joints feel better. In 92% of cases, everything clears up in 3 to 7 days. A small number (8%) might have lingering itchiness or joint discomfort for up to 3 months, but that’s rare.Some parents worry: “Can we ever give this antibiotic again?” The answer is no - not cefaclor, not the one that triggered it. But for other antibiotics? Absolutely. Many families are terrified to try penicillin again. But studies show that when kids are properly tested - through supervised oral challenges - 92% tolerate non-cefaclor beta-lactams without issue. That’s why allergists recommend rechallenge between 6 and 36 months after the reaction. The window? Around 12 months is typical.
And here’s something most people don’t know: SSLR doesn’t affect vaccines. You can still give your child the rabies vaccine, tetanus shot, or any other immunization. The risk of SSLR from vaccines is so low - 0.003% - it’s not a concern. That’s a myth that needs to die.
How Is It Treated?
There’s no magic cure. Treatment is about comfort and stopping the trigger.- Stop the antibiotic immediately. This is the single most important step.
- Antihistamines. Second-gen ones like cetirizine (0.25 mg/kg every 12 hours) help with itching. They don’t speed up healing, but they make the child feel better.
- NSAIDs. Ibuprofen (10 mg/kg every 8 hours) reduces fever and joint pain. Avoid aspirin in kids.
- Corticosteroids. Only for severe cases - like when the child can’t walk or sleep because of pain. Prednisone at 1 mg/kg/day for 7-10 days, then slowly tapered, works well. But don’t use them lightly.
Don’t use epinephrine. This isn’t anaphylaxis. Don’t give antibiotics to “treat the rash.” That’s how you make it worse.
Why Misdiagnosis Is So Dangerous
Here’s the hidden cost: when a doctor writes “penicillin allergy” in a child’s chart because of SSLR, it changes everything. That child is now more likely to get vancomycin, clindamycin, or azithromycin - drugs that are more expensive, harder on the gut, and contribute to antibiotic resistance. In the U.S. alone, misdiagnosed SSLR leads to $187 million in unnecessary healthcare costs every year.And it’s not just money. One parent on a Reddit thread shared: “My son got labeled allergic after amoxicillin SSLR. Now every infection? Vancomycin. He’s had three C. diff infections. I wish I’d known this wasn’t a true allergy.”
Another problem? 74% of pediatricians still label SSLR as “allergy” in electronic health records. That’s because they’re not trained to distinguish the two. That’s why 68% of cases need referral to an allergist - not just for confirmation, but to fix the record.
What’s Next? Research and Better Tools
The medical world is catching up. In 2024, SSLR got its own ICD-11 code: RA43.1. That means doctors can finally code it correctly - not as an allergy, not as a rash, but as its own distinct condition.Research is moving fast. The University of California is testing a urine test that looks for specific metabolites linked to SSLR. Early results show 94% accuracy. If it works, we could have a simple, non-invasive way to diagnose it in the doctor’s office - no blood draws, no waiting.
And in Boston, Boston Children’s Hospital is piloting an AI tool that scans electronic records for patterns: “Child had rash + fever + joint pain 8 days after cefaclor.” If the system flags it, it auto-suggests “SSLR, not allergy” to the provider. In a 2023 trial, it had 88% sensitivity and 91% specificity. That’s huge.
By 2030, experts predict misdiagnosis rates will drop below 15% in high-income countries. But in places where labs are scarce - like parts of Southeast Asia - the rate is still 40%. That’s a global health gap we can’t ignore.
What Should You Do If You Suspect SSLR?
If your child develops a rash, fever, and joint pain after an antibiotic:- Stop the antibiotic right away.
- Call your pediatrician - don’t wait for it to get worse.
- Ask: “Could this be a serum sickness-like reaction?”
- Request a referral to a pediatric allergist - not just for testing, but to correct the medical record.
- Don’t accept a label of “penicillin allergy” without proof.
- Keep a written record of the timing, symptoms, and antibiotic name.
Most kids recover fully. With the right diagnosis, they can go on to take penicillin again - safely - if they ever need it. That’s not just medical accuracy. It’s better care. It’s less risk. It’s peace of mind.

 Vitamin E and Warfarin: What You Need to Know About the Bleeding Risk
Vitamin E and Warfarin: What You Need to Know About the Bleeding Risk
 How and Where to Buy Keppra Online: Safe Ordering & Tips
How and Where to Buy Keppra Online: Safe Ordering & Tips
 10 Health Benefits of Adding Sundew to Your Supplement Routine
10 Health Benefits of Adding Sundew to Your Supplement Routine
 Polypharmacy and Side Effects: How Taking Too Many Medications Increases Health Risks
Polypharmacy and Side Effects: How Taking Too Many Medications Increases Health Risks
 Zovirax Cream vs Topical Antiviral Alternatives: A Detailed Comparison
Zovirax Cream vs Topical Antiviral Alternatives: A Detailed Comparison