When you're pregnant, taking folic acid isn't just a suggestion-it's a medical necessity. The neural tube, which becomes your baby's brain and spine, closes by day 28 after conception. Most women don't even know they're pregnant that early. That's why doctors recommend starting folic acid before you conceive. But here's the part no one talks about: folic acid doesn't play nice with every medication you might be taking.
Why Folic Acid Matters More Than You Think
Folic acid is the synthetic form of vitamin B9, and it's not the same as the folate you get from spinach or lentils. Your body processes it differently. Synthetic folic acid is absorbed 100% when taken on an empty stomach, compared to just 50% from food. That's why prenatal vitamins contain it-not because it's natural, but because it works better.
The CDC recommends 400 micrograms (mcg) daily for anyone who could get pregnant. Once you're pregnant, that jumps to 600 mcg. Most prenatal vitamins give you 600-1,000 mcg. That’s not a coincidence. Research from the 1990s showed that taking this dose before and during early pregnancy cuts the risk of neural tube defects-like spina bifida-by 50 to 70%.
The U.S. government started requiring folic acid in bread, pasta, and rice back in 1998. Since then, NTD rates have dropped by nearly half. But supplements still matter. Why? Because not everyone eats fortified foods. And even if they do, the dose from food alone isn’t enough to reach the protective level.
What Medications Can Interfere With Folic Acid?
Folic acid isn’t harmless. It can weaken the effect of some drugs-or be weakened by them. Here are the big ones:
- Anticonvulsants: Phenytoin (Dilantin), carbamazepine (Tegretol), and valproic acid (Depakote) are used to control seizures. Folic acid can reduce their effectiveness. There are real cases where women on these drugs had breakthrough seizures after starting prenatal vitamins. Women with epilepsy often need 4,000-5,000 mcg daily-but only under a neurologist’s supervision.
- Methotrexate: Used for rheumatoid arthritis, psoriasis, and sometimes ectopic pregnancies. Folic acid doesn’t cancel out methotrexate’s benefits; it actually helps reduce its side effects like nausea and liver damage. But timing matters. Doctors often prescribe low-dose folic acid (1-5 mg) on different days than methotrexate.
- Pyrimethamine: Used to treat toxoplasmosis during pregnancy. Folic acid can make this drug less effective. Pharmacists report that 32% of pregnant women on this medication need dose adjustments when adding folic acid.
- Sulfasalazine: Used for ulcerative colitis and Crohn’s disease. This drug blocks folic acid absorption. The UK’s NICE guidelines warn that women on sulfasalazine should not take folic acid without medical oversight.
- Antacids and calcium supplements: These aren’t drugs per se, but they interfere. Taking folic acid with calcium-rich foods or antacids cuts absorption by 25-50%. That means if you’re popping Tums or drinking milk with your prenatal, you’re not getting the full dose.
Iron in Prenatal Vitamins Can Block Folic Acid Too
Most prenatal vitamins combine folic acid with iron. That makes sense-pregnancy increases blood volume, and iron prevents anemia. But here’s the catch: iron and folic acid compete for absorption in the gut. A 2017 study in the American Journal of Clinical Nutrition found that taking them together reduces folic acid absorption by 20-30%.
That’s why so many women report nausea and stomach upset with prenatal vitamins. It’s not just the iron-it’s the combo. A 2023 survey by What to Expect found that 78% of women felt sick from iron-containing prenatal vitamins. Of those, 62% switched to taking folic acid separately, at a different time of day.
Practical tip: Take your prenatal vitamin with breakfast, and if you’re also taking a standalone folic acid supplement, take it at night. Or take the folic acid on an empty stomach with water in the morning, and the iron later with food. Space them out by at least 4 hours.
What About MTHFR Gene Mutations?
Some people have a genetic variation called MTHFR 677C>T. It’s found in 10-15% of Caucasians and up to 25% of Hispanics. This mutation makes it harder for the body to convert folic acid into its active form, L-methylfolate.
Does that mean you should avoid folic acid? No. But it does mean you might need a different kind of supplement. In 2023, the FDA approved the first prenatal vitamin with Quatrefolic®, a form of L-methylfolate that doesn’t need conversion. It’s priced higher-around $46/month-but it’s a game-changer for people with MTHFR mutations.
Don’t get tested for MTHFR unless your doctor recommends it. Most people with the mutation do fine on standard folic acid. But if you’ve had a previous pregnancy affected by a neural tube defect, or you’re on high-dose folic acid and still seeing elevated homocysteine levels, talk to your provider about switching.
How Much Is Too Much?
The upper limit for folic acid is 1,000 mcg per day for adults. That’s the amount most prenatal vitamins contain. But some women take more-sometimes without knowing why.
There’s a myth that more folic acid = better protection. It’s not true. Studies show that beyond 1,000 mcg, there’s no added benefit for preventing neural tube defects. And there might be risks.
Some researchers, like Dr. Joseph Selhub from Tufts University, worry about unmetabolized folic acid building up in the blood. This can happen when people take high doses regularly. The CDC says there’s no confirmed harm, but they also say more research is needed.
One concern: high folic acid might mask a vitamin B12 deficiency. That’s dangerous because B12 deficiency can cause nerve damage. If you’re over 50, vegetarian, or have had gastric surgery, your doctor should check your B12 levels before you start high-dose folic acid.

What About Autism Risk?
There’s been a lot of buzz about folic acid and autism. A 2022 study of over 45,000 children found that taking folic acid before and during early pregnancy was linked to a 40% lower risk of autism. But a 2021 Danish study of 35,000 children found no link.
Why the difference? The Israeli study looked at women who took folic acid consistently. The Danish study included women who started late-or didn’t take it at all. Timing matters. The benefit seems strongest when you start before conception and keep taking it through the first trimester.
Right now, the CDC is testing a new initiative: adding folic acid to corn masa flour. Why? Hispanic women have 20-30% higher rates of neural tube defects. Many eat corn tortillas daily but not fortified wheat products. This change could close the gap.
What Should You Actually Do?
Here’s your simple action plan:
- If you’re trying to get pregnant, start taking 400-800 mcg of folic acid at least one month before conception.
- Choose a prenatal vitamin with 600-800 mcg folic acid. If you’re on anticonvulsants, ask your neurologist if you need 4,000-5,000 mcg.
- If you’re on methotrexate, pyrimethamine, or sulfasalazine, tell your OB-GYN and pharmacist. They may need to adjust your doses.
- Take your prenatal vitamin with food to reduce nausea. Take folic acid separately if you’re also using a standalone supplement.
- Avoid taking folic acid with antacids, calcium supplements, or dairy at the same time.
- Don’t take more than 1,000 mcg unless your doctor says so.
- If you’ve had a previous pregnancy with a neural tube defect, talk to your doctor about higher doses and genetic testing.
Folic acid isn’t magic. It’s science. And like all science, it works best when you understand how it fits into your whole health picture-not just as a pill you swallow without thinking.
Can I get enough folic acid from food alone during pregnancy?
No. Even if you eat a lot of leafy greens, beans, and fortified grains, you won’t get the 600 mcg DFE needed during pregnancy. The body absorbs only about half the folate from food. Supplements are necessary to reach protective levels.
Is it safe to take folic acid with my prenatal vitamin if I’m also on an antidepressant?
Yes, most antidepressants don’t interact with folic acid. SSRIs like sertraline or fluoxetine are safe to take with prenatal vitamins. But always tell your doctor what you’re taking. Some rare medications, like certain anticonvulsants used for mood disorders, can interact.
What if I didn’t start folic acid until I was already pregnant?
Start immediately. While the neural tube closes by week 4, continuing folic acid through the first trimester supports healthy brain and spinal cord development. It’s not too late. Many women don’t know they’re pregnant until week 5 or 6. Taking it now still helps.
Do I need to take folic acid after the first trimester?
Yes. While the neural tube closes early, folic acid continues to support your baby’s rapid cell growth, placental development, and your own increased blood volume. Most doctors recommend continuing through pregnancy and even while breastfeeding.
Can I take a separate folic acid supplement if my prenatal doesn’t have enough?
Only if your doctor recommends it. Most prenatal vitamins already provide 600-1,000 mcg. Taking extra without medical advice can push you over the 1,000 mcg daily limit. High doses without a medical reason aren’t proven to help and could mask other issues like B12 deficiency.
Are there prenatal vitamins without folic acid?
No, not in the U.S. All prenatal vitamins sold legally must contain folic acid. If you find one without it, it’s not FDA-compliant. Even those marketed as “natural” or “food-based” still include synthetic folic acid to meet regulatory standards.
What should I do if I accidentally took too much folic acid?
If you took 2,000 mcg once by accident, don’t panic. Your body will excrete the excess. But if you’ve been taking more than 1,000 mcg daily for weeks, talk to your doctor. They may check your B12 levels and blood homocysteine to make sure there’s no hidden issue.

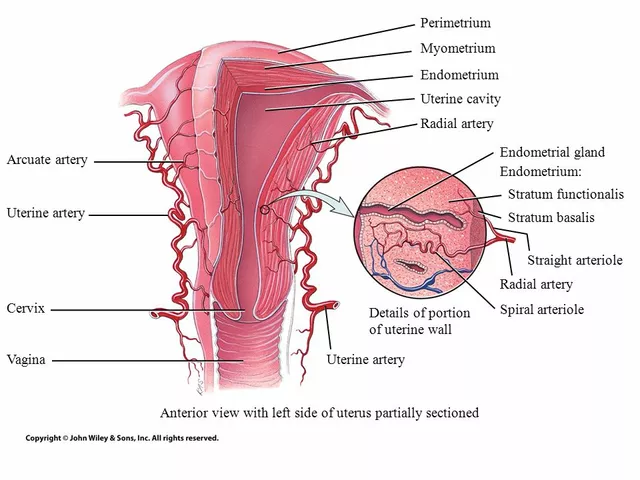 The Connection Between Overgrowth in the Uterine Lining and Migraines
The Connection Between Overgrowth in the Uterine Lining and Migraines
 St. John’s Wort and Prescription Drug Interactions: What You Need to Know
St. John’s Wort and Prescription Drug Interactions: What You Need to Know
 Grifulvin V: Uses, Side Effects, and Essential Tips for Antifungal Treatment
Grifulvin V: Uses, Side Effects, and Essential Tips for Antifungal Treatment
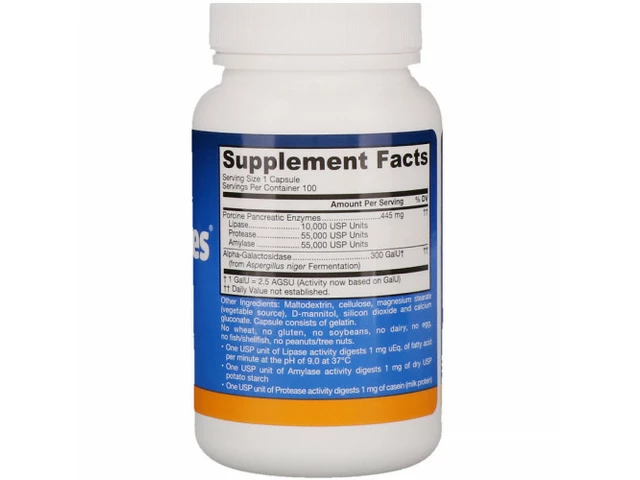 Unlock the Power of Lipase: The Ultimate Dietary Supplement for Improved Digestion
Unlock the Power of Lipase: The Ultimate Dietary Supplement for Improved Digestion
Glendon Cone
December 30, 2025 AT 15:33srishti Jain
December 31, 2025 AT 05:56Henry Ward
December 31, 2025 AT 10:16Hayley Ash
January 2, 2026 AT 01:08kelly tracy
January 3, 2026 AT 11:25Shae Chapman
January 5, 2026 AT 09:19Aayush Khandelwal
January 6, 2026 AT 15:24Kunal Karakoti
January 6, 2026 AT 23:08henry mateo
January 7, 2026 AT 10:44Sandeep Mishra
January 7, 2026 AT 18:01Kelly Gerrard
January 8, 2026 AT 22:57Cheyenne Sims
January 9, 2026 AT 15:44Joseph Corry
January 10, 2026 AT 11:39Nadia Spira
January 10, 2026 AT 16:02