Digital Therapeutic Interaction Checker
Select Your Condition
FDA-Cleared Digital Therapeutics
No selection yet
Select a condition to see relevant FDA-cleared DTx
Interaction Results
Select your condition and medications to see interaction results
When you take a pill every day, it’s not just about the drug-it’s about you. Whether you’re managing diabetes, depression, or high blood pressure, missing even one dose can throw off your whole treatment. That’s where digital therapeutics (DTx) come in. These aren’t apps that track steps or remind you to drink water. These are FDA-cleared, clinically proven software tools designed to help you stick to your meds, understand side effects, and even adjust your behavior in real time. And now, they’re being used alongside traditional medications more than ever before.
What Exactly Are Digital Therapeutics?
Digital therapeutics are software programs that deliver medical treatment. They’re not supplements. They’re not wellness trackers. They’re medical devices-approved by the FDA-to treat, manage, or prevent disease. The first one cleared was reSET in 2018 for substance use disorder. Since then, dozens more have followed, including DaylightRx, approved on September 4, 2024, for generalized anxiety disorder in adults 22 and older.
Unlike a simple pill reminder app, DTx uses algorithms to deliver personalized therapy. For diabetes, platforms like DarioEngage analyze your glucose readings and suggest insulin adjustments. For ADHD, EndeavorRx uses video-game-like tasks to train attention skills. For mental health, DTx apps guide users through cognitive behavioral therapy (CBT) modules tailored to their symptoms and medication side effects.
These tools work on smartphones or tablets, requiring iOS 13+ or Android 8+ with at least 2GB of RAM. Some, like EndeavorRx, need a gaming-capable device because they rely on fast visual feedback loops. Most are prescribed by a doctor and integrated into your care plan-not optional add-ons.
How DTx Improves Medication Adherence
One in three prescriptions go unfilled after being written. That’s not because people don’t want to get better-it’s because of cost, confusion, fear of side effects, or just forgetting. Traditional methods like pharmacy calls or printed instructions only improve first-fill rates by 15-20%. DTx fixes this.
Medisafe, a leading digital drug companion, found that patients using their platform saw a 25% increase in adherence for chronic conditions like diabetes, asthma, and anticoagulant therapy. Why? Because DTx doesn’t just remind you. It reacts.
- If you skip a dose, it asks why-was it too expensive? Too scary? Too confusing?
- If you report nausea after taking your antidepressant, it offers coping strategies or alerts your provider.
- If you’re about to refill your warfarin, it checks your recent INR readings and flags potential risks.
For patients on high-risk meds like insulin, antiretrovirals, or blood thinners, this isn’t convenience-it’s life-saving. A 6-month trial with DarioEngage showed patients using it alongside standard medication reduced HbA1c levels 1.2% more than those on meds alone. That’s the difference between uncontrolled diabetes and avoiding kidney failure or amputation.
When DTx and Medications Interact-The Real Risks
Most people assume digital tools don’t interact with pills. That’s a dangerous myth. DTx doesn’t contain chemicals, but it changes how your body responds to them.
Take mental health. A 2023 study in Psychiatry Advisor found that some patients using CBT-based DTx for anxiety reported increased agitation when combined with SSRIs. Why? The therapy pushed them to confront fears they weren’t emotionally ready to handle-something their medication was helping them tolerate. Without proper monitoring, this could lead to worsening symptoms.
Another example: EndeavorRx, approved for ADHD, caused non-serious side effects in 7% of users-headaches, dizziness, nausea, even emotional outbursts. In kids already on stimulants like Adderall, these effects overlapped. Some parents didn’t realize the DTx was contributing, not just the medication.
And it’s not just side effects. DTx can influence dosing decisions. A 2023 ASCPT paper suggested that real-time data from DTx apps could one day trigger automatic dose adjustments. Imagine your insulin pump adjusting based on your stress levels tracked by a DTx app. Sounds smart-until you realize no one’s studied how cortisol spikes from anxiety apps might interfere with glucose metabolism long-term.
Right now, there’s no standardized way to report DTx-medication interactions. Pharmacovigilance systems track drug side effects-but not when a digital therapy makes a drug less effective-or more dangerous.
Who Benefits Most? Who Gets Left Behind?
DTx shines for chronic conditions where behavior matters as much as biology. Diabetes, COPD, depression, opioid use disorder-all show strong results.
For opioid addiction, one DTx paired with buprenorphine led to a 16.3% greater reduction in illicit drug use at 12 weeks compared to medication alone. That’s huge.
But it doesn’t work for everyone.
Patients over 65 have a 45% higher chance of quitting DTx within a month if they don’t get in-person help. Seniors without tech experience, or those with vision or memory issues, struggle with small buttons, complex menus, or voice-guided instructions that don’t adapt to their pace.
And let’s not forget the digital divide. A 2024 JMCP study found that low-income patients were 30% less likely to be offered DTx by their providers-even when it was clinically appropriate-because of assumptions about smartphone access or literacy.
Even when patients use DTx successfully, integration with pharmacies and EHRs is messy. Over 60% of negative reviews mention poor syncing with refill systems. You get a perfect adherence score in the app, but your pharmacy still doesn’t know you’re on track-so they don’t prioritize your refill.
What’s Changing in 2026?
The DTx market hit $3.8 billion in 2023 and is projected to grow to $14.2 billion by 2028. That’s not hype-it’s reality. Major pharma companies like Pfizer, Novo Nordisk, and Eli Lilly now include DTx as part of their core product strategy. Why? Because they’re seeing real results.
By 2026, 40% of chronic disease management will include some form of DTx. Specialty pharmacies are already moving toward mandatory enrollment: by 2027, 65% of high-cost prescriptions will require a DTx companion to qualify for insurance coverage.
The FDA is preparing new guidance for Q2 2025 focused on combination studies-how DTx works alongside drugs. That’s a big deal. Right now, DTx gets cleared based on small trials. Soon, regulators will demand data on how these tools interact with medications over time.
And the biggest shift? DTx is becoming part of the treatment algorithm. No longer an add-on. Not a bonus. A core part of care. Think of it like a new kind of medicine-one you download, not dispense.

What Should You Do?
If you’re on chronic medication:
- Ask your doctor: Is there an FDA-cleared DTx that pairs with my treatment?
- Don’t assume all health apps are the same. Only look for ones labeled “prescription digital therapeutic” or cleared by the FDA.
- Track how you feel-not just your numbers. If you’re more anxious, dizzy, or overwhelmed after starting a DTx, tell your provider. It might not be your drug.
- Insist on support. If you’re over 60 or not tech-savvy, ask for a “DTx navigator”-a staff member who walks you through setup.
- Check if your pharmacy integrates with the app. If not, bring a printed report to your next visit.
If you’re a provider:
- Don’t hand out apps like brochures. Prescribe them like you would a drug-with dosage, duration, and follow-up.
- Learn how to interpret DTx data. A spike in skipped doses might mean financial stress, not noncompliance.
- Document DTx use in your EHR. If it’s not recorded, it’s not part of your patient’s treatment plan.
Frequently Asked Questions
Are digital therapeutics the same as health apps?
No. Health apps track fitness, sleep, or mood without clinical validation. Digital therapeutics are FDA-cleared medical devices designed to treat specific conditions. Only those with FDA clearance (like DaylightRx or DarioEngage) are considered true DTx. Apps without regulatory approval are not substitutes for medical treatment.
Can digital therapeutics replace my medication?
Sometimes, but rarely. DaylightRx is approved as a standalone treatment for generalized anxiety disorder, but most DTx are designed as adjuncts. They help you take your meds better, manage side effects, or adjust behaviors-not replace the drug. Never stop medication without consulting your doctor, even if your DTx app says you’re doing well.
Do DTx interact with over-the-counter drugs or supplements?
DTx itself doesn’t chemically interact with OTCs or supplements-but the behavior changes it drives might. For example, a DTx encouraging you to exercise more could affect how your body metabolizes blood pressure meds. Or a mindfulness app reducing stress might lower your need for sleep aids. Always tell your provider about every DTx you’re using, even if it’s not a prescription.
Is DTx covered by insurance?
Coverage is growing but inconsistent. Medicare and some private insurers now cover FDA-cleared DTx for diabetes, mental health, and opioid use disorder-especially if prescribed by a provider. However, many plans still treat them as “wellness tools.” Ask your insurer for a list of covered DTx and always get a written prescription to submit with your claim.
What if I don’t have a smartphone?
Some DTx platforms offer web-based versions or phone-based support. Others partner with clinics to provide tablets. If you can’t use a smartphone, ask your provider about alternatives. You shouldn’t be denied effective care because of tech access. Many programs now include loaner devices or home visits for patients who need them.

 Eastern Hemlock: The Groundbreaking Dietary Supplement You Can't Afford to Miss Out On
Eastern Hemlock: The Groundbreaking Dietary Supplement You Can't Afford to Miss Out On
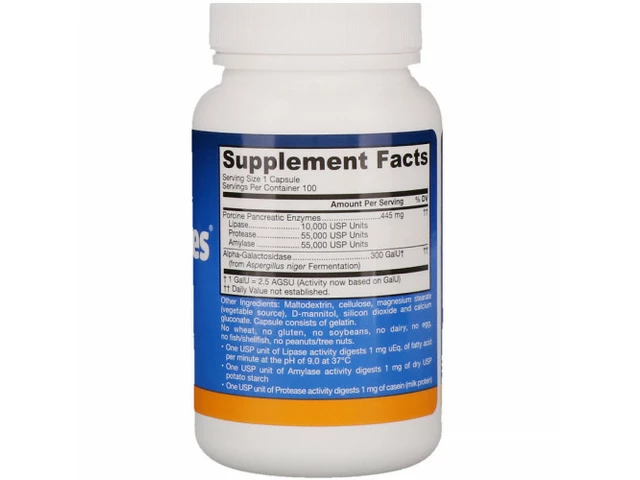 Unlock the Power of Lipase: The Ultimate Dietary Supplement for Improved Digestion
Unlock the Power of Lipase: The Ultimate Dietary Supplement for Improved Digestion
 Allergic Reactions to Generics: When to Seek Medical Care
Allergic Reactions to Generics: When to Seek Medical Care
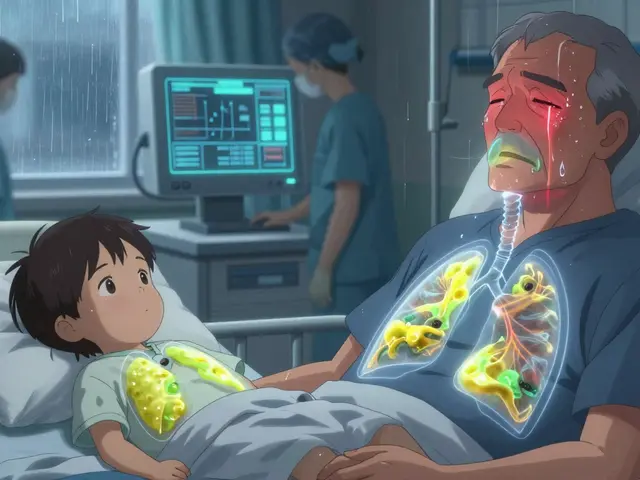 Pneumonia Types: Bacterial, Viral, and Fungal Lung Infections Explained
Pneumonia Types: Bacterial, Viral, and Fungal Lung Infections Explained
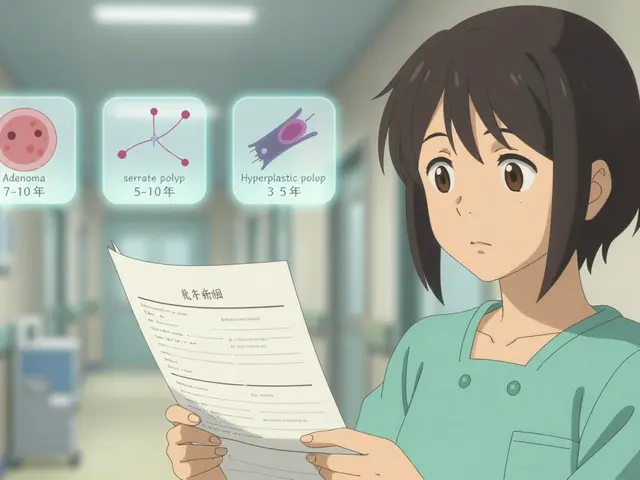 Repeat Colonoscopy: What Your Surveillance Interval Should Be After Polyp Removal
Repeat Colonoscopy: What Your Surveillance Interval Should Be After Polyp Removal