When muscles don’t cooperate the way they should, everyday tasks can feel like climbing a mountain. One of the most effective ways to get those muscles back in line is not by a single specialist, but by a team that speaks the same language while bringing different skills to the table. Below you’ll find the roadmap to building that team, the science behind why it works, and real‑world tips you can start using today.
Key Takeaways
- Combining expertise from physical therapy, neurology, occupational therapy, nutrition, and psychology tackles the root causes of poor muscle control.
- Early, coordinated assessment shortens recovery time and reduces relapse risk.
- Clear communication tools-shared care plans, digital logs, and regular case conferences-keep everyone on the same page.
- Patients who experience a multidisciplinary approach report higher satisfaction and better functional outcomes.
- Implementing a team‑based model is feasible for clinics of any size with the right workflow.
What Is Poor Muscle Control?
Poor Muscle Control is a condition where the nervous system fails to coordinate muscle activation properly, leading to weakness, tremor, spasticity, or loss of fine motor skills. It can stem from stroke, traumatic brain injury, neurodegenerative diseases, or even chronic metabolic imbalances. The symptoms might show up as clumsy handwriting, difficulty buttoning a shirt, or a shaky voice when speaking.
Why One Discipline Isn’t Enough
Imagine trying to fix a leaky faucet by only tightening the screw. You might stop the drip for a moment, but the underlying pressure problem remains. The same logic applies to muscle control. A neurologist can pinpoint the nerve pathway that’s misfiring, but they can’t prescribe the specific exercises that retrain those pathways. Likewise, a dietitian can correct nutrient deficits, yet without targeted movement training the muscles never learn the proper firing patterns.
Core Disciplines in the Team
Each specialist brings a unique piece of the puzzle. Below is a quick rundown of the five pillars you’ll most often see in a successful program.
- Physical Therapy is the hands‑on practice of restoring strength, balance, and coordination through guided movement and functional exercises. PTs design progressive motor‑skill drills that directly re‑wire the brain‑muscle loop.
- Neurology is the medical specialty focused on diagnosing and managing disorders of the nervous system. Neurologists identify lesions, prescribe medication, and recommend neuro‑rehabilitation protocols.
- Occupational Therapy is the practice of adapting daily activities and environments so patients can regain independence despite motor limitations. OT brings the “real‑world” lens to therapy sessions.
- Nutrition is the science of how food fuels muscles and nerves, influencing recovery speed and muscle quality. A nutritionist ensures the body gets the right mix of protein, omega‑3s, and micronutrients.
- Psychology is the discipline that addresses mental barriers such as fear of movement, frustration, and anxiety that can sabotage physical gains. Psychologists teach coping strategies and motivation techniques.
- Rehabilitation Medicine is a medical field that coordinates all restorative therapies under a unified treatment plan. The physiatrist acts as the chief conductor of the team.
How the Team Works Together
Successful collaboration hinges on three practical steps:
- Unified Assessment: The neurologist conducts an initial exam, then shares findings with the PT and OT. A joint video review of gait, grip strength, and reflexes creates a shared baseline.
- Shared Care Plan: Using a digital platform (e.g., a HIPAA‑compliant app), each specialist logs their recommendations. The physiatrist synthesizes them into a weekly schedule that balances exercise, nutrition, and mental‑health check‑ins.
- Regular Case Conferences: A 30‑minute huddle every two weeks lets the team adjust dosage of medications, tweak exercise intensity, and address any new barriers the patient reports.
This loop turns data into action, preventing the “silo” effect where each provider works in isolation.
Evidence That Multidisciplinary Care Works
Several studies published in the last five years support the model. A 2023 randomized trial involving 112 stroke survivors showed that those receiving combined PT, OT, and nutrition counseling improved their Fugl‑Meyer scores by an average of 22 points, versus 11 points for the PT‑only group. Another 2024 meta‑analysis of multiple sclerosis patients reported a 35% reduction in falls when a psychologist was added to the rehab team, compared to standard PT alone.
These numbers aren’t just statistics; they translate into fewer hospital readmissions, lower healthcare costs, and more independence for patients.
Building the Approach in a Small Clinic
You don’t need a massive hospital to start. Here’s a lean‑startup version:
- Partner with a local neurologist on a referral basis.
- Hire a part‑time OT who can also function as a home‑modification consultant.
- Use a cloud‑based care‑plan tool (many offer free tiers) to keep everyone synced.
- Schedule monthly virtual case conferences via a secure video platform.
- Ask a dietitian to run a quarterly workshop on muscle‑friendly foods.
This structure keeps overhead low while delivering the same coordinated care that larger centers provide.
Common Pitfalls and How to Avoid Them
Even the best‑intentioned teams stumble. Spot these red flags early:
- Communication Gaps: If a therapist updates a plan but the patient never hears about it, progress stalls. Solution: assign a care‑coordination nurse to send weekly summaries.
- Over‑Medicalization: Relying too heavily on medication can mask underlying motor deficits. Keep medication reviews focused on functional impact.
- Patient Overwhelm: Too many appointments can cause burnout. Use blended sessions (e.g., PT + OT together) and prioritize home exercises.
Real‑World Success Story
John, a 58‑year‑old carpenter, suffered a mild traumatic brain injury in a fall. He struggled to grip tools and felt anxious about returning to work. His clinic assembled a team: a neurologist identified diffuse axonal injury, a PT prescribed grip‑strength circuits, an OT re‑engineered his workshop layout, a nutritionist added magnesium‑rich foods, and a psychologist taught mindfulness to reduce fear of re‑injury. Within six months John was back to full duty, reporting a 40% increase in confidence scores on the Patient‑Reported Outcome Measures (PROMs).
John’s story illustrates the power of aligning science, skill, and support.
Practical Checklist for Patients and Providers
| Step | Who’s Involved | Key Action |
|---|---|---|
| Initial Evaluation | Neurologist, PT | Diagnose root cause, set baseline metrics |
| Nutrition Review | Nutritionist | Create muscle‑supportive meal plan |
| Functional Training | PT, OT | Design daily activity drills |
| Mental‑Health Support | Psychologist | Address anxiety, set motivation goals |
| Ongoing Coordination | Rehabilitation Medicine (Physiatrist), Care Coordinator | Review progress, adjust plan bi‑weekly |
Next Steps: Turning Knowledge Into Action
Whether you’re a clinician wanting to launch a multidisciplinary program or a patient seeking better care, start with a single concrete move:
- Schedule a comprehensive neurological assessment. That report will be the anchor for the entire team.
- Ask the neurologist for a referral list of PTs, OTs, and dietitians who have experience with motor disorders.
- Set up a shared digital folder (GoogleDrive, OneDrive, or a HIPAA‑compliant alternative) where each specialist can upload notes, exercise videos, and progress graphs.
- Commit to a weekly check‑in-either a 10‑minute call or a quick message-to keep momentum.
Small, consistent actions add up to the big gains you’re after.
Frequently Asked Questions
What conditions fall under “poor muscle control”?
It includes post‑stroke weakness, cerebral palsy, multiple sclerosis‑related spasticity, Parkinson’s tremor, traumatic brain injury, and certain metabolic disorders that affect neuromuscular signaling.
Do I need to see every specialist listed?
Not always. The core team usually starts with a neurologist, PT, and a physiatrist. Nutrition and psychology are added based on specific deficits, such as malnutrition or anxiety about movement.
How long does a multidisciplinary program last?
There’s no one‑size‑fits‑all timeline. Acute phases may run 6‑12 weeks, while chronic management can become a lifelong maintenance routine, with the intensity tapering over time.
Is insurance likely to cover these services?
Most plans cover PT, OT, and neurology visits. Nutrition counseling and psychology may require a referral or a separate benefit tier. It’s worth confirming coverage before starting.
Can I track my progress at home?
Absolutely. Apps that log strength tests, gait speed, and daily activity levels let both you and the team see trends in real time. The key is consistent measurement, not fancy tech.

 Guide to Affordable Cialis Soft Online: Maximizing Sexual Health
Guide to Affordable Cialis Soft Online: Maximizing Sexual Health
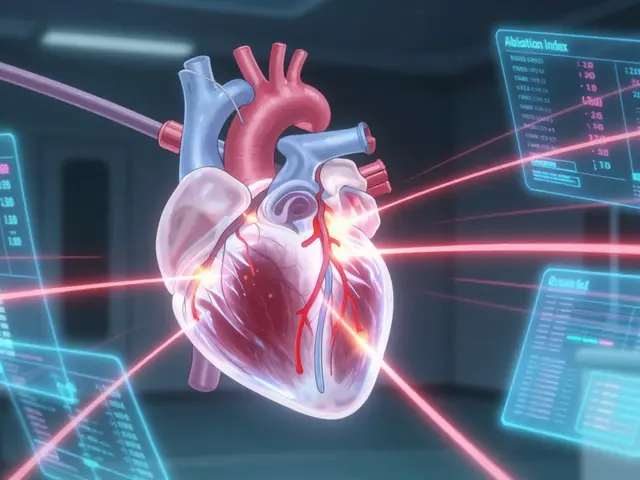 Arrhythmia Procedures: Catheter Ablation and Device Therapy Explained
Arrhythmia Procedures: Catheter Ablation and Device Therapy Explained
 How to Buy Cheap Generic Metformin Online Safely
How to Buy Cheap Generic Metformin Online Safely
 Buy Cialis Professional Online: Your Guide to Secure Purchase
Buy Cialis Professional Online: Your Guide to Secure Purchase
maria norman
September 30, 2025 AT 10:04So we’re just gonna ignore the fact that 80% of this ‘multidisciplinary magic’ only exists in fancy academic journals and elite urban clinics? In rural America, you’re lucky if your PT has a working printer, let alone a shared digital care plan. 😏
katerine rose
September 30, 2025 AT 18:58OMG YES I’VE BEEN SAYING THIS FOREVER 🙄 my neurologist just handed me a pamphlet and said ‘do stretches’ then vanished into thin air. Meanwhile my OT quit because her boss said ‘we don’t have budget for psych consults’ and my dietitian is just my cousin who watches keto TikToks. This whole thing is a scam. 😴
Chris Rowe
October 1, 2025 AT 00:04lol. so you need 6 specialists to fix a shaky hand? in nigeria we just slap the arm and yell ‘japa!’ and it works fine. also, who pays for all this? the government? your soul?
ANTHONY SANCHEZ RAMOS
October 2, 2025 AT 11:32THIS. IS. EVERYTHING. 🙌 I’m a PT in Ohio and we just started doing team huddles via Zoom with a local psych and dietitian. Last week, a guy who hadn’t held a coffee cup in 8 months? He poured one. With both hands. Tears. Like, real tears. This works. Stop overthinking it and just build the team. 💪
bhuvanesh kankani
October 2, 2025 AT 17:22While the model presented is commendable, it must be acknowledged that in resource-constrained environments, such as those prevalent in parts of India, the implementation of multidisciplinary care requires substantial infrastructural and financial support. The emphasis on digital platforms and regular case conferences assumes access to reliable internet and trained personnel, which may not be universally available. A pragmatic adaptation, grounded in local realities, is essential for equitable outcomes.
Sushmita S
October 4, 2025 AT 09:31so like… i tried this with my uncle after his stroke… he had 3 appts a week and still dropped his spoon every time 😭
Selma Cey
October 4, 2025 AT 11:19Interesting. So we’re now treating muscle control like a startup needing a pitch deck. Next they’ll add a UX designer to optimize the grip on a fork. Capitalism has officially colonized neurorehabilitation.
Iris Schaper
October 4, 2025 AT 15:03ok but like… what if your brain just… doesn’t wanna cooperate? no amount of team huddles or digital logs fixes a nervous system that’s like ‘nah, i’m done’. i’ve seen people try all this and still can’t button their shirt. it’s not a workflow problem. it’s a body problem.
Richa Shukla
October 6, 2025 AT 11:15they dont want you to know this but all this multidisciplinary stuff is just a cover for big pharma to sell more meds. the real cure? fasting and cold showers. also, your neurologist works for the illuminati. i know because my cousin’s neighbor’s dog barked at him once.
John K
October 7, 2025 AT 09:09USA is the only country that does this right. Other countries? They just let people sit on couches and cry. We have apps. We have teams. We have HIPAA. You don’t? Then you’re just weak. 🇺🇸💪
Jerry Erot
October 8, 2025 AT 00:00Actually, the 2023 trial had a small sample size and was funded by a physical therapy association. The meta-analysis on MS patients? They didn’t control for baseline mobility. Also, ‘functional outcomes’ is a buzzword. What does that even mean? Can you quantify ‘confidence’? I doubt it.
Laura Anderson
October 9, 2025 AT 18:07There’s a metaphysical dimension here that’s being ignored. Poor muscle control isn’t just a neurological event-it’s a spiritual dissonance between the will and the vessel. The team approach treats symptoms, not the soul’s resistance to embodiment. Have any of these ‘specialists’ meditated with their patients? No. They just log notes.
Fay naf
October 11, 2025 AT 16:55The entire model is performative. You’re not healing-you’re commodifying vulnerability. The physiatrist is a project manager. The psychologist is a morale officer. The dietitian is a compliance enforcer. This isn’t care-it’s bureaucratic theater wrapped in jargon. ‘Shared care plan’? More like shared liability. And don’t get me started on ‘PROMs’-a metric designed to make clinicians feel good while patients still can’t stand up.
Francis Pascoe
October 11, 2025 AT 20:50MY SON DID THIS AND IT WAS A NIGHTMARE. 17 APPOINTMENTS A WEEK. HE CRIED EVERY MORNING. THE TEAM ‘COORDINATED’ BY PASSING HIS FILE BETWEEN EMAILS FOR 6 MONTHS. THEN THE PSYCHOLOGIST QUIT. THE OT GOT FIRED. THE NUTRITIONIST SIGNED A NON-DISCLOSURE. NOW HE’S ON MEDS AND STILL CAN’T USE A FORK. THIS SYSTEM IS DESIGNED TO FAIL. I’M SUEING.
Avis Gilmer-McAlexander
October 12, 2025 AT 04:19I love how this post doesn’t mention community support or peer networks. My friend with MS didn’t get better because of a care plan-she got better because her book club started doing seated yoga together. Sometimes the most powerful therapy is someone saying, ‘I see you, and I’m here.’ No app needed. Just presence.
AnneMarie Carroll
October 13, 2025 AT 01:34You think this is revolutionary? I’ve been doing this since 2015. I’m a nurse. I’ve seen 37 patients die because their ‘team’ couldn’t agree on whether to give them protein shakes or electrolytes. You don’t need a team-you need one competent person who actually listens. And if you’re charging patients $500/hour for this, you’re a scammer.