Vaccine Storage Deployment: How to Keep Vaccines Safe from Factory to Injection
When you get a vaccine, you're not just receiving a shot—you're receiving the result of a complex, tightly controlled system called vaccine storage deployment, the end-to-end process of maintaining vaccines at precise temperatures from manufacturing to administration. Also known as the vaccine cold chain, it’s the reason your flu shot still works after being shipped across the country. If even one link in this chain breaks, the vaccine can lose potency. That’s not a small risk—it’s a public health threat.
Not all vaccines are the same. Some, like the original Pfizer-BioNTech COVID-19 vaccine, need to be kept at -70°C. Others, like the Moderna shot, can survive at -20°C. And many routine vaccines, like MMR or hepatitis B, just need standard refrigeration between 2°C and 8°C. Each type requires different tools: ultra-cold freezers, temperature-monitored transport boxes, insulated coolers, and real-time data loggers. This isn’t just about having a fridge—it’s about knowing exactly where each dose is, what temperature it’s been at, and whether it’s still good to use.
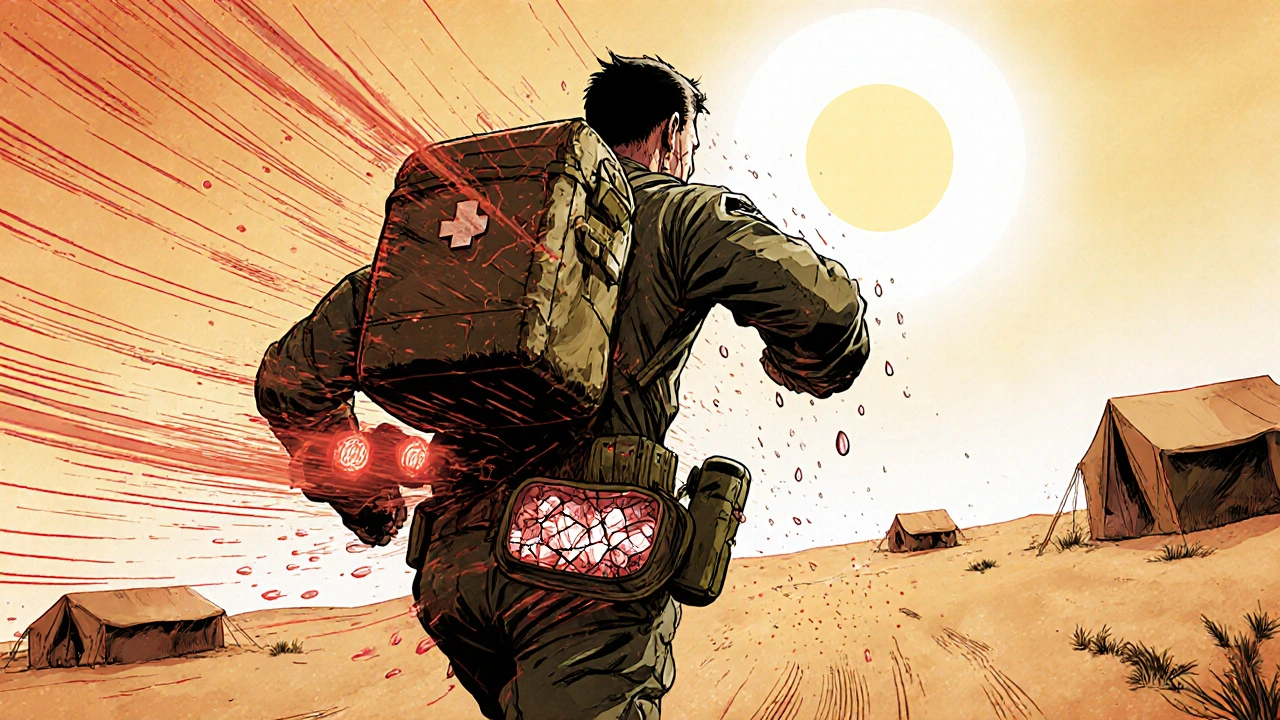
vaccine cold chain, the network of people, equipment, and procedures that maintain vaccine integrity during transport and storage involves pharmacies, clinics, hospitals, delivery trucks, and even remote field teams in rural areas. In the U.S., the CDC tracks vaccine temperatures across thousands of sites. In low-resource regions, solar-powered refrigerators and temperature-sensitive labels help bridge the gap. The goal? Zero tolerance for temperature excursions. One study found that vaccines exposed to heat above recommended levels lost up to 40% of their effectiveness—even if they looked fine.
It’s not just about freezing or cooling. vaccine temperature control, the precise management of thermal conditions to preserve biological activity also means avoiding freezing for vaccines that shouldn’t be frozen, like some flu shots. Shaking, light exposure, and delays during transport can also damage them. That’s why trained staff, clear protocols, and backup power systems are just as important as the equipment.
When vaccine storage deployment fails, people don’t just miss out on protection—they might get sick because they thought they were safe. That’s why every step matters: from the factory’s quality checks, to the warehouse’s monitoring system, to the nurse pulling the vial from the cooler at your appointment. It’s a silent system, but one that saves millions of lives every year.
Below, you’ll find real-world guides on how vaccines are handled, what goes wrong when things slip, and how to spot the signs of compromised doses. Whether you’re a healthcare worker, a logistics manager, or just someone who wants to understand why your shot works, these posts give you the facts—not the fluff.