Sexual Arousal Disorder – What It Is, Why It Happens, and How to Treat It
When talking about sexual arousal disorder, a condition where the body struggles to generate or maintain sexual excitement. Also known as sexual dysfunction, it can affect anyone regardless of age or gender and often signals deeper health issues.
Breaking Down the Main Subtypes
The umbrella of sexual arousal disorder includes several specific problems. In men, the most common form is erectile dysfunction, the inability to achieve or keep an erection sufficient for intercourse. Women experience a parallel condition called female sexual dysfunction, difficulty with desire, arousal, or orgasm. Both subtypes share risk factors like cardiovascular disease, diabetes, and stress, but each also has unique triggers that need targeted attention.
Sexual arousal disorder encompasses these subtypes, meaning any treatment plan must first identify whether the issue is primarily male or female focused. This classification guides doctors toward the right tests and therapies, ensuring you don’t waste time on unrelated remedies.
Hormonal balance plays a huge role, too. Hormonal imbalance, abnormal levels of testosterone, estrogen, or thyroid hormones, can blunt desire and make physical response sluggish. Likewise, problems with the pelvic floor—like pelvic floor dysfunction, weak or uncoordinated muscles that control urinary and sexual function—can reduce sensation and interfere with orgasm.
Psychological stress and medication side effects act as invisible culprits. Anxiety, depression, or relationship conflict often dampen arousal, while drugs such as antidepressants or antihypertensives may directly suppress sexual response. In this way, psychological factors influence sexual arousal disorder just as much as physical ones.
Getting a clear diagnosis starts with a thorough medical history and a few focused tests. Blood work checks hormone levels, a cardiovascular exam rules out blood‑flow issues, and a pelvic floor assessment evaluates muscle strength. For men, an erection test with a medication called alprostadil can pinpoint vascular problems. Women may undergo a vaginal pressure test to see how well pelvic muscles are coordinating during arousal.
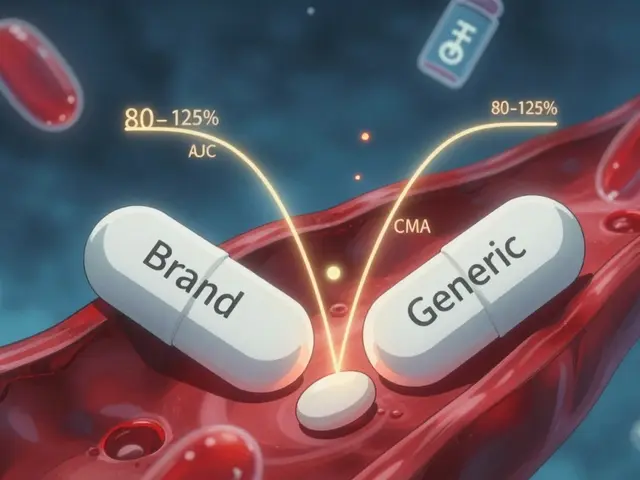
Once the root cause is known, treatment can be customized. Lifestyle changes—regular exercise, balanced diet, and quitting smoking—boost overall circulation and hormone health. Psychological counseling or sex therapy helps untangle mental blocks. Medications like PDE‑5 inhibitors (for erectile dysfunction) or low‑dose testosterone (for hormonal deficits) address specific physiological gaps. Physical therapy targeting the pelvic floor rebuilds muscle control, and lubricants or vibrators can enhance sensory input for both sexes.
Below you’ll find a curated selection of articles that dive deeper into each of these areas. Whether you’re looking for medical explanations, practical tips, or the latest research on sexual arousal disorder, the posts ahead will give you clear, actionable information to move forward with confidence.